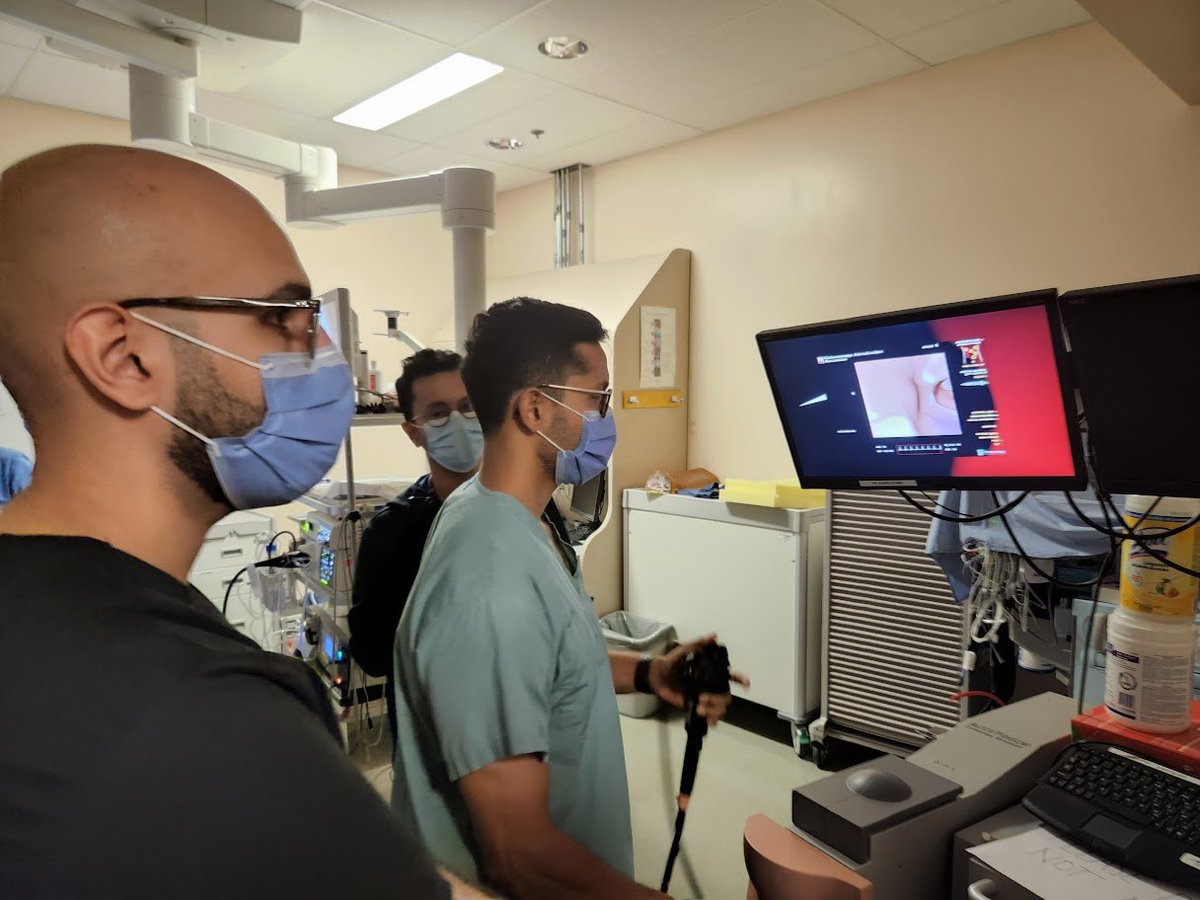
How do you train beginners at #endoscopy?
This week we are running the endoscopy #simulation course @UofTGastroHep @SMH_GI.
Our training to novices before they start endoscopic rotations is based on three educational principles.
#MedEd #GITwitter
This week we are running the endoscopy #simulation course @UofTGastroHep @SMH_GI.
Our training to novices before they start endoscopic rotations is based on three educational principles.
#MedEd #GITwitter
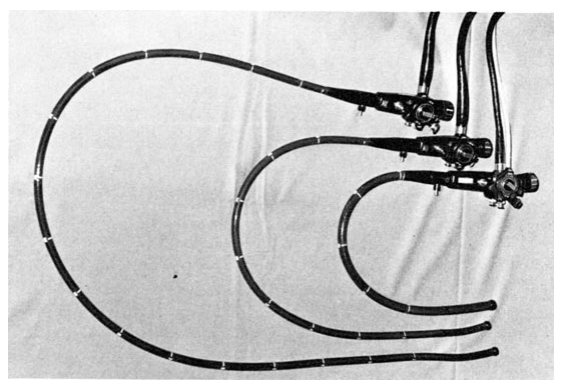
1. Modifying cognitive load
We use low fidelity simulators for basic skills (dial/button control, torque, stance, etc.) in a low risk envt. This allows the trainee to focus on basics without being overloaded by complex tasks - no patient, vital signs, assistants, sedation, etc.
We use low fidelity simulators for basic skills (dial/button control, torque, stance, etc.) in a low risk envt. This allows the trainee to focus on basics without being overloaded by complex tasks - no patient, vital signs, assistants, sedation, etc.
2. Optimizing challenge points
We favor matching complexity of task being taught to the skill of learner. If task is too simple - there is nothing to learn. If the task is too complex, the trainee will struggle to learn anything.
We favor matching complexity of task being taught to the skill of learner. If task is too simple - there is nothing to learn. If the task is too complex, the trainee will struggle to learn anything.

We operationalized this in novice colonoscopist simulation training with "progressive learning" - recurrent assessment during training, progression to next task when optimal challenge identified.
Led to superior transfer of skills to the clinical setting
sciencedirect.com/science/articl…
Led to superior transfer of skills to the clinical setting
sciencedirect.com/science/articl…

3. Mastery learning
Each skill is practiced to the point of mastery in the simulated setting - where learners practice deliberately w/ feedback/coaching until a high performance threshold is reached. Best described by @giendo_roy in a study in simulated EGD in @AGA_Gastro in 2020
Each skill is practiced to the point of mastery in the simulated setting - where learners practice deliberately w/ feedback/coaching until a high performance threshold is reached. Best described by @giendo_roy in a study in simulated EGD in @AGA_Gastro in 2020

Additionally we espouse emerging technologies and adopt them quickly - e.g. augmented reality, 3D printing for design and some low-cost and home learning sims.
Will put up some videos of some of our experimental sims as the week progresses.
Will put up some videos of some of our experimental sims as the week progresses.

• • •
Missing some Tweet in this thread? You can try to
force a refresh