#AKIConsultSeries Middle-aged male ➡️🏥 for painful knee and fever. Now in shock 🚨
📂Chart review: PMH EtOH Cirrhosis, right knee arthroplasty.
It is always a good practice review previous PACS images🩻: Nodular liver, colateral vessels and prosthetic right knee
1/11
📂Chart review: PMH EtOH Cirrhosis, right knee arthroplasty.
It is always a good practice review previous PACS images🩻: Nodular liver, colateral vessels and prosthetic right knee
1/11
On exam: BP 72/48, HR 82, O2Sat 95%.
CRT 7 sec, 🧠somnolent, confused. No edema, no obvious ascites.
Warm, swollen and erythematous knee: Tap with obvious purulent fluid🧫
Cr 2.8 mg/dl (baseline 0.5), K 6.7, Urine 🔬: hyaline casts, some urothelial cells
2/11
CRT 7 sec, 🧠somnolent, confused. No edema, no obvious ascites.
Warm, swollen and erythematous knee: Tap with obvious purulent fluid🧫
Cr 2.8 mg/dl (baseline 0.5), K 6.7, Urine 🔬: hyaline casts, some urothelial cells
2/11
Loos like hemodynamic AKI (AKA Pre-renal)
Usual causes in Cirrhosis:
🔷Distributive: Septic, "Hepatorenal physiology" 🔷Hypovolemic: Laxatives, vomiting, large volume paracentesis
🔷Congestive: Porto-pulmonary HTN, Co-existing cardiomyopathy
3/11
Usual causes in Cirrhosis:
🔷Distributive: Septic, "Hepatorenal physiology" 🔷Hypovolemic: Laxatives, vomiting, large volume paracentesis
🔷Congestive: Porto-pulmonary HTN, Co-existing cardiomyopathy
3/11
What is the usual initial guideline-recommended treatment in this scenarios?
Cirrhosis + AKI: Albumin, fluids
Sepsis: Antibiotics, source control (prosthesis removal), fluids
¿Can we do better?
Yes, quick screen for fluid tolerance in 1 minute #POCUS: #IVC and #LUS
4/11
Cirrhosis + AKI: Albumin, fluids
Sepsis: Antibiotics, source control (prosthesis removal), fluids
¿Can we do better?
Yes, quick screen for fluid tolerance in 1 minute #POCUS: #IVC and #LUS
4/11
Lung Ultrasound (#LUS) looks ok, but IVC is plethoric 🚩🚩🚩
I have wrote about thus scenario before: criticalcarenow.com/albumin-for-vo…
Venous congestion needs further evaluation!
5/11
I have wrote about thus scenario before: criticalcarenow.com/albumin-for-vo…
Venous congestion needs further evaluation!
5/11

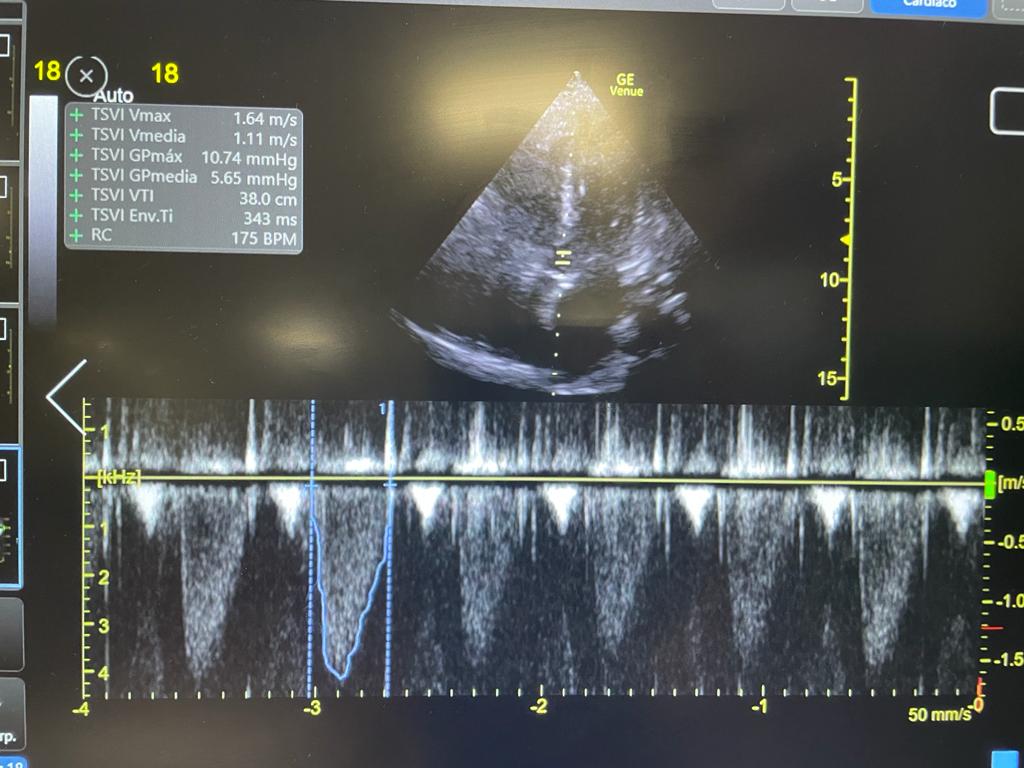
#Echofirst PLAx, PSAx, A4ch (RV view).
Good LV, Septal Shift (D-Sign), Dilated RV and RA, RV systolic disfunction and Severe Tricuspid regurgitation!
6/11
Good LV, Septal Shift (D-Sign), Dilated RV and RA, RV systolic disfunction and Severe Tricuspid regurgitation!
6/11
#Hemodynamics
#VExUS HV: S wave reversal, PV: Non pulsatile (Not reliable in Cirrhosis), IRVD: Monophasic.
RVOT Doppler: Notched Envelope
TRVMax: 2.8 m/sec (note triangular shape, because of severe TR, this can't be used to estimate sPAP)
LVOT VTI: 18 (not so bad)
7/11
#VExUS HV: S wave reversal, PV: Non pulsatile (Not reliable in Cirrhosis), IRVD: Monophasic.
RVOT Doppler: Notched Envelope
TRVMax: 2.8 m/sec (note triangular shape, because of severe TR, this can't be used to estimate sPAP)
LVOT VTI: 18 (not so bad)
7/11

This hemodynamic evaluation is compatible with pre-capillary pulmonary hypertension with severe venous congestion (monophasic IRVD)!
As previous echo (2 yrs ago) showed no evidence of PH, we got AngioCT: It ruled out PE
8/11
As previous echo (2 yrs ago) showed no evidence of PH, we got AngioCT: It ruled out PE
8/11

Working Dx: Septic arthritis with underlying Porto-pulmonary hypertension
#HemodynamicAKI: distributive + congestive
Fluids and albumin were 🛑
Vasopressin, NE, Levosimendan and Furosemide were started. Source was controlled
Despite MAP >80. Patient remained Oliguric
9/11
#HemodynamicAKI: distributive + congestive
Fluids and albumin were 🛑
Vasopressin, NE, Levosimendan and Furosemide were started. Source was controlled
Despite MAP >80. Patient remained Oliguric
9/11
CRRT was initiated and a negative fluid balance of 3-4 L daily was obtained. After 48 hrs, pt started producing urine. We kept decongesting with diuretics.
Patient was fully decongested, AKI resolved.
Repeat #echofirst showed persistent severe PH and severe TR
10/11

Patient was fully decongested, AKI resolved.
Repeat #echofirst showed persistent severe PH and severe TR
10/11


Lessons:
1) AKI-Fluid reflex prevented by #POCUS (#IVC + #LUS to check for Fluid Tolerance)
2) In Cirrhosis, use intra-renal doppler for #VExUS (PV not reliable)
3) #VExUS can be used to monitor decongestion even in severe TR
POCUS Always
/END
1) AKI-Fluid reflex prevented by #POCUS (#IVC + #LUS to check for Fluid Tolerance)
2) In Cirrhosis, use intra-renal doppler for #VExUS (PV not reliable)
3) #VExUS can be used to monitor decongestion even in severe TR
POCUS Always
/END
• • •
Missing some Tweet in this thread? You can try to
force a refresh