‼️ #CriticalCare #Tweetorial ‼️
🫁 Tracheostomy Basics & Trach Emergencies 🫁
Join me on a review tracheostomy tube basics and can't miss emergency situations!
#EmoryNCCTweetorials
#FOAMcc for #CritCare #EmergencyMedicine #HospitalMedicine #MedEd #Neurocrit #PulmCrit
1/🧵
🫁 Tracheostomy Basics & Trach Emergencies 🫁
Join me on a review tracheostomy tube basics and can't miss emergency situations!
#EmoryNCCTweetorials
#FOAMcc for #CritCare #EmergencyMedicine #HospitalMedicine #MedEd #Neurocrit #PulmCrit
1/🧵

Goals for this #Tweetorial
1-Review basics of the tracheostomy tube
2- Review anatomy relevant to tracheostomy placement
3- Safety tips for your inpatients with trachs
4- Review emergency situations relevant to trachs
2/🧵
1-Review basics of the tracheostomy tube
2- Review anatomy relevant to tracheostomy placement
3- Safety tips for your inpatients with trachs
4- Review emergency situations relevant to trachs
2/🧵
Lets start with a case...
60s y/o male with a left basal ganglia ICH 🧠 who is now s/p bedside percutaneous tracheostomy placement 4 days ago. You are called into the room for a high pressure alarm 🚨
What is your first step?
3/🧵
60s y/o male with a left basal ganglia ICH 🧠 who is now s/p bedside percutaneous tracheostomy placement 4 days ago. You are called into the room for a high pressure alarm 🚨
What is your first step?
3/🧵
Evaluate the patient!
Lets review the head/neck anatomy relevant to tracheostomy tubes!
A percutaneous trach is typically placed between the 1st and 2nd tracheal rings. This image from @derangedphys shows the relevant portions of the trachea
4/🧵
Lets review the head/neck anatomy relevant to tracheostomy tubes!
A percutaneous trach is typically placed between the 1st and 2nd tracheal rings. This image from @derangedphys shows the relevant portions of the trachea
4/🧵

From an internal aspect, the tracheostomy lies below the level of the vocal cords as shown.
Another important anatomical relation to note is the locational of the innominate artery on this image.
5/🧵
Another important anatomical relation to note is the locational of the innominate artery on this image.
5/🧵

Now that you know where the tracheostomy is, what are the components of the tube itself?
1- Outer cannula/Faceplate
2- Pilot balloon
3- Cuff
4- Inner Cannula
5- Obturator
6/🧵
1- Outer cannula/Faceplate
2- Pilot balloon
3- Cuff
4- Inner Cannula
5- Obturator
6/🧵

At placement when sizing a trach the proceduralist may consider placing a standard or XLT trach.
Proximal XLT is useful for patients w/thick necks
Distal XLT is useful for patients w/tracheal stenosis
7/🧵
Proximal XLT is useful for patients w/thick necks
Distal XLT is useful for patients w/tracheal stenosis
7/🧵

Now that you have a handle on the head/neck anatomy and the components of a tracheostomy tube, what are the other "must haves" in your patient's room?
8/🧵
8/🧵
Patients with a trach in an ICU setting should have the following:
1- Sign on door describing trach
2- Extra trach in the room
3- Obturator/syringe in the room
4- BVM
5- End-Tidal Co2 Monitor
6- Knowledge of where your emergency equipment is! (Airway box, fiberoptic etc)
9/🧵
1- Sign on door describing trach
2- Extra trach in the room
3- Obturator/syringe in the room
4- BVM
5- End-Tidal Co2 Monitor
6- Knowledge of where your emergency equipment is! (Airway box, fiberoptic etc)
9/🧵

Back to our case... you have your room prepared, you know your airway anatomy, and the components of the tracheostomy.
So what is causing the ventilator to alarm?
10/🧵
So what is causing the ventilator to alarm?
10/🧵
Approaching any trach emergency, prepare backup airway and ventilate the patient as you troubleshoot
3 easy steps (your room has all these materials at bedside!):
1- Deflate the cuff on the trach
2- Bag-Valve Mask ventilate patient via mouth
3- Monitor your EtCO2
11/🧵
3 easy steps (your room has all these materials at bedside!):
1- Deflate the cuff on the trach
2- Bag-Valve Mask ventilate patient via mouth
3- Monitor your EtCO2
11/🧵
Frame Tracheostomy Emergencies in your head based on timing and into 3 main categories:
Timing:
Early: <7-14 days
Late: >7-14 days
Categories:
1- Obstruction
2- Decannulation
3- Bleeding
12/🧵
Timing:
Early: <7-14 days
Late: >7-14 days
Categories:
1- Obstruction
2- Decannulation
3- Bleeding
12/🧵
⏳Early Obstruction:
Causes: Mucus plugging, clotting, *always consider decannulation*
Fixes: Pass suction catheter, remove inner canula, direct visualization w/fiberoptic
⌛️Late Obstruction:
Causes: Same as above
Fixes: Same, consider replacing trach at bedside
13/🧵
Causes: Mucus plugging, clotting, *always consider decannulation*
Fixes: Pass suction catheter, remove inner canula, direct visualization w/fiberoptic
⌛️Late Obstruction:
Causes: Same as above
Fixes: Same, consider replacing trach at bedside
13/🧵
⏳Early Decannulation:
Causes: Physical manipulation
Fixes: 🛑 CAUTION 🛑 reinsertion is high risk for creating false tract due to immature tract!
-Call for help early, ventilate from above, prepare to intubate
-Trained provider can reinsert w/direct visualization
14/🧵
Causes: Physical manipulation
Fixes: 🛑 CAUTION 🛑 reinsertion is high risk for creating false tract due to immature tract!
-Call for help early, ventilate from above, prepare to intubate
-Trained provider can reinsert w/direct visualization
14/🧵

⌛️Late Decannulation:
Causes: Physical manipulation
Fixes: Ventilate from above, prepare backup airway, reinsert or replace trach with obturator in place
15/🧵
Causes: Physical manipulation
Fixes: Ventilate from above, prepare backup airway, reinsert or replace trach with obturator in place
15/🧵
⏳Early Bleeding:
Causes: Typically related to surgical site, frequent suctioning, trauma to external site or trachea, or tracheitis
Fixes: Identify the source of the bleed, if external consider silver nitrite or direct pressure
16/🧵
Causes: Typically related to surgical site, frequent suctioning, trauma to external site or trachea, or tracheitis
Fixes: Identify the source of the bleed, if external consider silver nitrite or direct pressure
16/🧵
⌛️Late Bleeding:
Causes: 🛑CAUTION🛑 tracheoinominate fistula is a potential cause and is a surgical emergency!
Fixes: Early help from vascular/IR. Remove trach & intubate from above and hyperinflate cuff. Digital compression through stoma (as shown)
17/🧵
Causes: 🛑CAUTION🛑 tracheoinominate fistula is a potential cause and is a surgical emergency!
Fixes: Early help from vascular/IR. Remove trach & intubate from above and hyperinflate cuff. Digital compression through stoma (as shown)
17/🧵

Thats it for a brief overview of tracheostomies and trach emergencies!
Please comment with additional teaching, corrections, or additional comments!
@caseyalbin @drdangayach @Capt_Ammonia @neuro_intensive @JackieKraft4 @EmmGeezee @criticalbeansmd @AvrahamCooperMD
18/🧵
Please comment with additional teaching, corrections, or additional comments!
@caseyalbin @drdangayach @Capt_Ammonia @neuro_intensive @JackieKraft4 @EmmGeezee @criticalbeansmd @AvrahamCooperMD
18/🧵
References/Additional Resources:
@nickmmark @OnePagerICU has an exceptional resource on Tracheostomy Emergencies:
static1.squarespace.com/static/5e6d5df…
Excellent review article from UK Guidelines:
…-publications.onlinelibrary.wiley.com/doi/10.1111/j.…
19/🧵
@nickmmark @OnePagerICU has an exceptional resource on Tracheostomy Emergencies:
static1.squarespace.com/static/5e6d5df…
Excellent review article from UK Guidelines:
…-publications.onlinelibrary.wiley.com/doi/10.1111/j.…
19/🧵
The UK also has an entire society dedicated to trach emergencies:
tracheostomy.org.uk
Review Book chapter on Trach Emergencies:
pubmed.ncbi.nlm.nih.gov/30454773/
TIF Management:
optechtcs.com/article/S1522-…
20/🧵
tracheostomy.org.uk
Review Book chapter on Trach Emergencies:
pubmed.ncbi.nlm.nih.gov/30454773/
TIF Management:
optechtcs.com/article/S1522-…
20/🧵
@MaxHockstein @EmoryEM @maness_caroline @JayKinariwala @EmoryNeuroCrit @gradydoctor @GradyTraumaDoc @RandiSmithMD @pyang88 @gsmartinmd @NeuroBMNP @alchemyfinderAg @kellyperonti3 @drdangayach @aartisarwal @msiuba @emily_fri @namorrismd @BrookefPharmaC @grepmeded
21/🧵
21/🧵
@EmoryCCC @EmoryCritAPP @NaomiNiznick @shwetagoswamimd @MedTweetorials @iBookCC @internatwork @feras_akbik @clhallmd @CajalButterfly @DrSamanthaF @rishikumarmd @TracyVettese @tracyshirey @SitaraKoneru
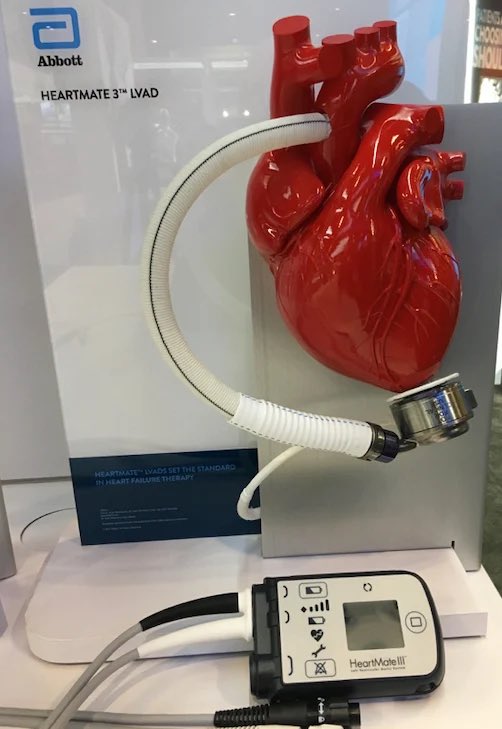
Be sure to check out my other #CriticalCare #Tweetorials on LVADs and CRRT!
https://twitter.com/EricLawson90/status/1506663696269029385
• • •
Missing some Tweet in this thread? You can try to
force a refresh