1/ What were the historical reasons for the resistance to recognizing airborne transmission during the COVID-19 pandemic?
Our peer-reviewed open-access paper is now published:
onlinelibrary.wiley.com/doi/10.1111/in…
Our peer-reviewed open-access paper is now published:
onlinelibrary.wiley.com/doi/10.1111/in…

2/ Soon after COVID-19 pandemic started, it was clear to many scientists (inc. those who understand aerosols) that AIRBORNE trans. was an important contributor
E.g. as soon as we talked to the Skagit choir, it was obvious that was airborne-dominated:
doi.org/10.1111/ina.12…
E.g. as soon as we talked to the Skagit choir, it was obvious that was airborne-dominated:
doi.org/10.1111/ina.12…
3/ However, major public health organizations such as @WHO and @CDCgov were in complete denial, saying that airborne transmission was MISINFORMATION!
(Disgracefully, @WHO has not deleted this tweet or clearly stated that it was an ENORMOUS error)

(Disgracefully, @WHO has not deleted this tweet or clearly stated that it was an ENORMOUS error)
https://twitter.com/WHO/status/1243972193169616898

4/ How was that possible?
- Many scientists are concluding that airborne transmission is important
- Major public health organizations such as @WHO say that it is misinformation!
Historical trends and errors (this thread) are important to explain this, but NOT the only reason
- Many scientists are concluding that airborne transmission is important
- Major public health organizations such as @WHO say that it is misinformation!
Historical trends and errors (this thread) are important to explain this, but NOT the only reason
5/ This major error (IMHO one of most important errors in the entire history of Public Health) has had major consequences:
- In early pandemic we focused on surfaces, which are minor or negligible
- we ignored air, which was the dominant mode
=> lack of controlling transmission
- In early pandemic we focused on surfaces, which are minor or negligible
- we ignored air, which was the dominant mode
=> lack of controlling transmission
6/ Since then, research has clearly shown that airborne transmission is the DOMINANT mode of transmission of COVID-19:
thelancet.com/article/S0140-…
thelancet.com/article/S0140-…
7/ To this day, 0 proven cases of surface transmission
And droplet transmission has NEVER been demonstrated, not just for COVID-19... but for ANY disease in the history of medicine!
[Paper from Prof. Yuguo Li, member of @WHO IPC Committee]
sciencedirect.com/science/articl…
And droplet transmission has NEVER been demonstrated, not just for COVID-19... but for ANY disease in the history of medicine!
[Paper from Prof. Yuguo Li, member of @WHO IPC Committee]
sciencedirect.com/science/articl…

8/ So how did we get into this mess?
PH organizations tell us that unproven transmission mechanisms are dominant, and that the dominant trans. mechanism is misinformation
We'll soon delve into the history in our paper.
onlinelibrary.wiley.com/doi/10.1111/in…
PH organizations tell us that unproven transmission mechanisms are dominant, and that the dominant trans. mechanism is misinformation
We'll soon delve into the history in our paper.
onlinelibrary.wiley.com/doi/10.1111/in…
9/ But before we go into the history, there are other reasons to review.
Most importantly, surface-droplet transmission is very CONVENIENT to those in power. And AIRBORNE trans. is an inconvenient truth (just like climate change, dealt with similarly)
telegraph.co.uk/global-health/…
Most importantly, surface-droplet transmission is very CONVENIENT to those in power. And AIRBORNE trans. is an inconvenient truth (just like climate change, dealt with similarly)
telegraph.co.uk/global-health/…

10/ There is at least one more reason for the resistance:
those who made this enormous error at @WHO, its IPC committee, @CDCgov, & health ministries around the world DO NOT WANT to admit their error
Govt advisor privately: "we need to find a way to allow us to save face"
those who made this enormous error at @WHO, its IPC committee, @CDCgov, & health ministries around the world DO NOT WANT to admit their error
Govt advisor privately: "we need to find a way to allow us to save face"
11/ And those Public Health officials that continue to resist and obfuscate about airborne transmission are in control of the PH institutions.
Aerosol scientists are almost complete outsiders, and have been almost systematically excluded to this day.
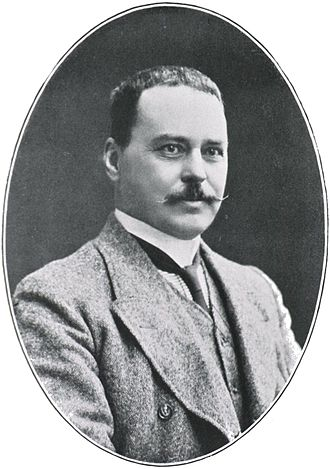
wellcomeopenresearch.org/articles/6-126
Aerosol scientists are almost complete outsiders, and have been almost systematically excluded to this day.
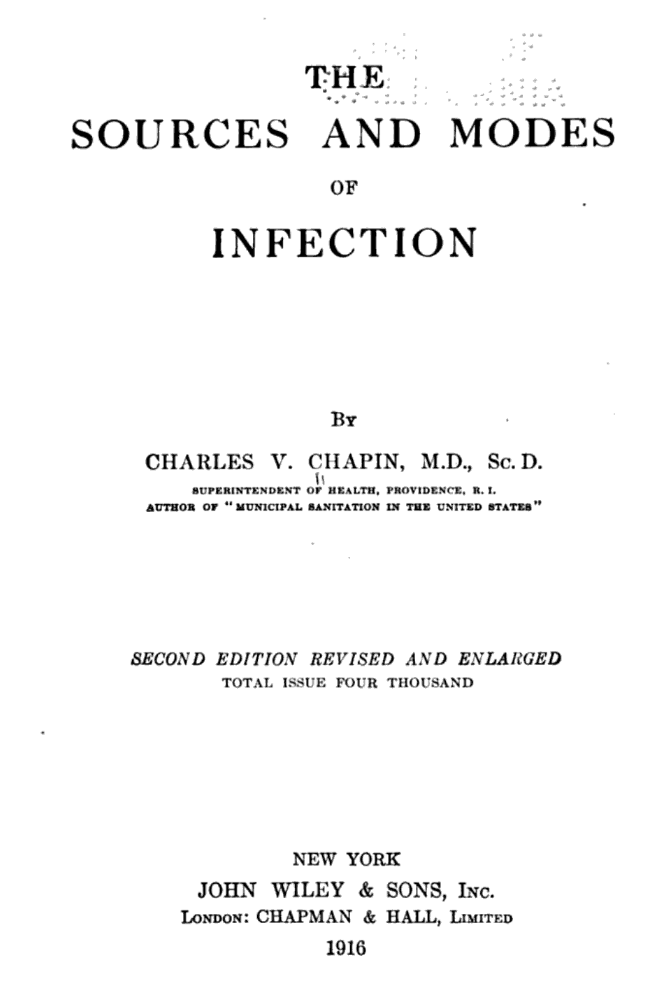
wellcomeopenresearch.org/articles/6-126

12/ So what about the contribution of history to the denial of and resistance to airborne transmission by Public Health authorities worldwide?
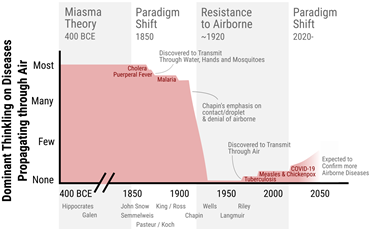
It is summarized in this diagram, which I'll explain in this thread:
onlinelibrary.wiley.com/doi/10.1111/in…
It is summarized in this diagram, which I'll explain in this thread:
onlinelibrary.wiley.com/doi/10.1111/in…
13/ Sorry, I need to take a break for some meetings (we are starting classes this week at @CUBoulder). I'll continue with the thread in 1 hr.
If you can't wait to read it, it is all in the paper:
onlinelibrary.wiley.com/doi/10.1111/in…
If you can't wait to read it, it is all in the paper:
onlinelibrary.wiley.com/doi/10.1111/in…
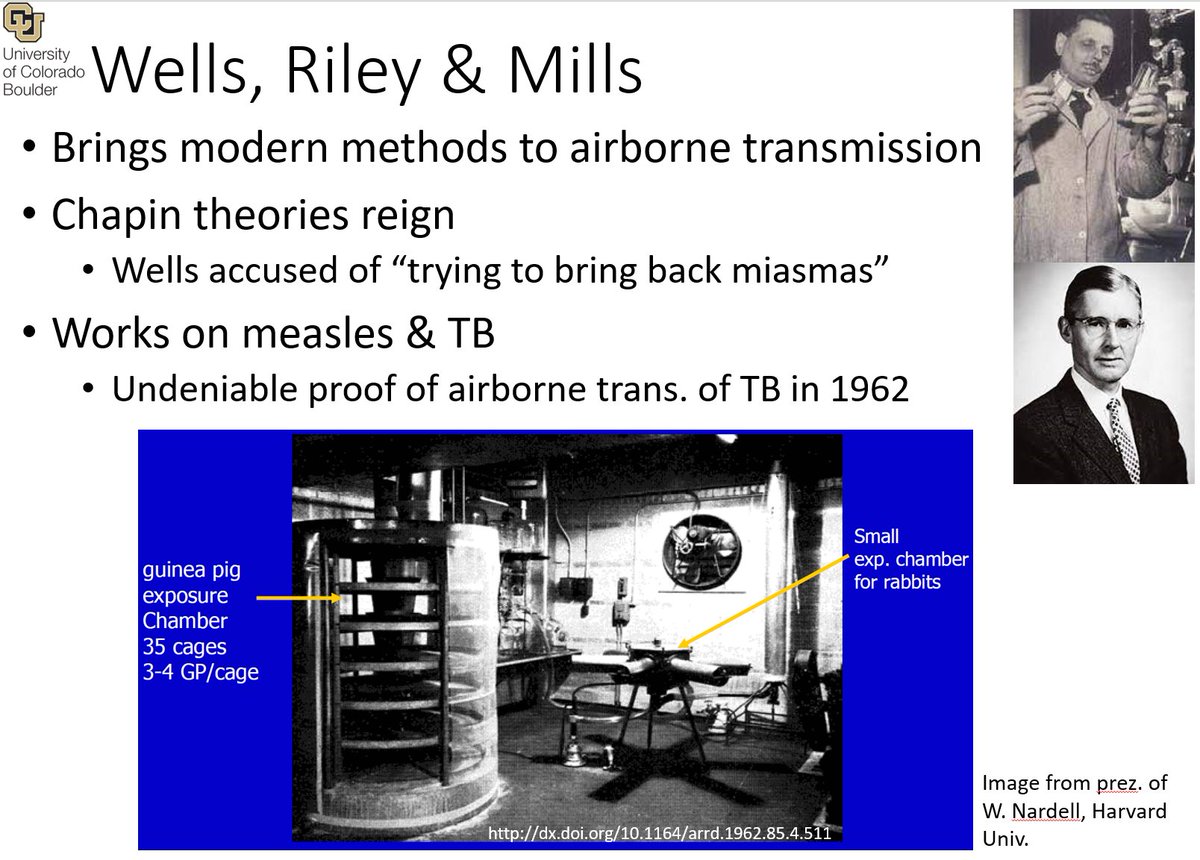
14/ So to understand the errors that led to the denial and resistance of #COVIDisAirborne, we need to go back to Hippocrates! (~400 BCE)
en.wikipedia.org/wiki/Hippocrat…
en.wikipedia.org/wiki/Hippocrat…

15/ Hippocratic writings in ancient Greece first proposed that diseases were caused by imbalance of humors in the body, which could be triggered by a “miasma” transmitted through the air
loebclassics.com/view/hippocrat…
loebclassics.com/view/hippocrat…

16/ Throughout much of subsequent human history, the belief persisted that diseases were transmitted through air
Because the actual agents remained a mystery for centuries, explanations were given in general terms such as “miasmas,” or “bad air”
en.wikipedia.org/wiki/Miasma_th…
Because the actual agents remained a mystery for centuries, explanations were given in general terms such as “miasmas,” or “bad air”
en.wikipedia.org/wiki/Miasma_th…

17/ For example, the etymological root of the term "malaria" (a disease that we now know is transmitted by mosquitos) is “mala aria,” medieval Italian for “bad air”
doi.org/10.1186/1475-2…
doi.org/10.1186/1475-2…
17/ Some origin theories were more specific. E.g. Roman scholar Varro (116–27 BCE) wrote that swamps were a particular breeding ground for minute creatures that “float in the air and enter the body through mouth & nose and there cause serious diseases.”
doi.org/10.1186/1475-2…
doi.org/10.1186/1475-2…
18/ Thus it became a policy of the Roman Empire to drain swamps, removing breeding grounds for mosquitos, reducing malaria, an example of a mistaken theory giving good results
and increasing faith on the theory
We see this many times through history
doi.org/10.1186/1475-2…
and increasing faith on the theory
We see this many times through history
doi.org/10.1186/1475-2…
19/ The concept of person-to-person contagion came much later, most clearly in work of Italian physician Girolamo Fracastoro in 1546
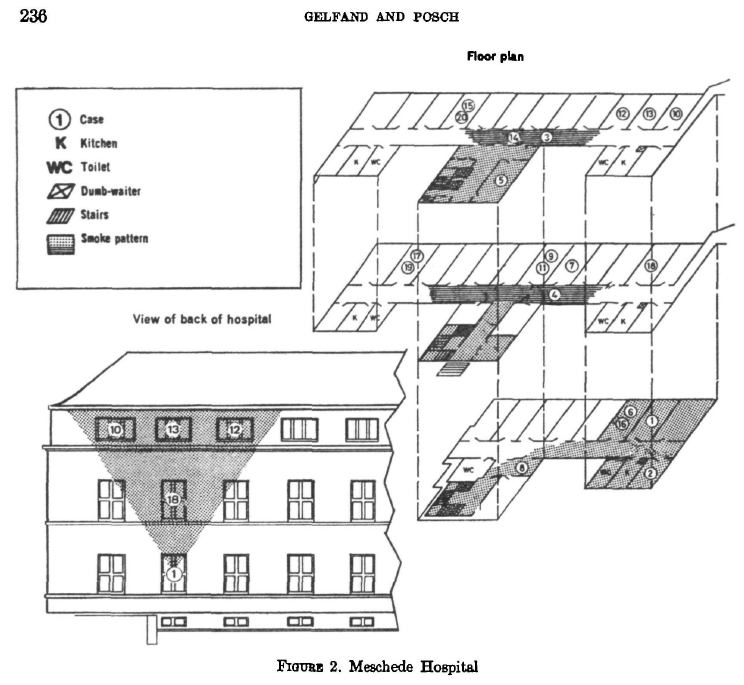
[This is actually a subject of current debate, with some scholars thinking that the role of F may have been overstated]
en.wikipedia.org/wiki/Girolamo_…
[This is actually a subject of current debate, with some scholars thinking that the role of F may have been overstated]
en.wikipedia.org/wiki/Girolamo_…

20/ What ensued after Fracastoro, however, was a centuries-long debate between “miasmatists,” who held fast to the idea that diseases floated through the air over distances, and “contagionists,” who accepted person-to-person spread of disease
sciencedirect.com/science/articl…
sciencedirect.com/science/articl…
21/ Because it was (and it still IS) very difficult to determine how, why, and from where someone became infected, the miasmas vs. contagion debate failed to reach a resolution and persisted for centuries.
22/ A middle ground was proposed, “contingent contagionism”: malaria, or cholera might be contagious in an impure atmosphere, but not in a healthy atmosphere
This idea therefore captured some grains of truth (eg. now we know ventilation reduces airborne)
archive.org/details/390020…
This idea therefore captured some grains of truth (eg. now we know ventilation reduces airborne)
archive.org/details/390020…
23/ Miasma theory was dominant till the mid/late 19thy Century. Florence Nightingale (1820–1910) like most Victorians was raised to believe that diseases were caused by ‘miasma’ or foul air.
en.wikipedia.org/wiki/Florence_…
en.wikipedia.org/wiki/Florence_…

24/ In her Notes on Hospitals, Nightingale referred to the idea of contagion as absurd:
[She was nevertheless very practical and effective in reducing disease, e.g. with ventilation and phys. distance, and later accepted germ theory, as we'll see later]
play.google.com/store/books/de…
[She was nevertheless very practical and effective in reducing disease, e.g. with ventilation and phys. distance, and later accepted germ theory, as we'll see later]
play.google.com/store/books/de…

25/ We enter a critical period around 1850. Miasma theory is still dominant, although contagion (mostly through the air) also has proponents.
Microorganisms have been observed for 2 centuries since the invention of the microscope, but haven't clearly been connected to disease
Microorganisms have been observed for 2 centuries since the invention of the microscope, but haven't clearly been connected to disease
26/ Cholera strikes London in 1854.
The public health establishment believed it to be caused by a miasma. English sanitary reformers (e.g. Chadwick), who initiated many modern public health practices, found miasma appealing, as it appeared to explain...
en.wikipedia.org/wiki/Edwin_Cha…
The public health establishment believed it to be caused by a miasma. English sanitary reformers (e.g. Chadwick), who initiated many modern public health practices, found miasma appealing, as it appeared to explain...
en.wikipedia.org/wiki/Edwin_Cha…

27/ ...the prevalence of diseases in the undrained, filthy, and foul-smelling areas where the poor lived, and helped justify their efforts to address those conditions.
[They had made a huge error, and they resisted accepting it, just as @WHO today]
doi.org/10.1136/bmj.32…
[They had made a huge error, and they resisted accepting it, just as @WHO today]
doi.org/10.1136/bmj.32…
28/ John Snow was a wealthy doctor but outsider to public health.
His work in anesthesia made him familiar with the behavior of gasses. He realized that the spread of chlore was NOT consistent with what would be expected for a gas.
en.wikipedia.org/wiki/John_Snow
His work in anesthesia made him familiar with the behavior of gasses. He realized that the spread of chlore was NOT consistent with what would be expected for a gas.
en.wikipedia.org/wiki/John_Snow

29/ Snow noticed how cases had clustered in a specific London borough and persuaded the local council to remove the handle of the Broad street water pump, which halted the epidemic.
archive.org/details/b28985…
ph.ucla.edu/epi/snow/snowc…
blog.rtwilson.com/john-snows-cho…
archive.org/details/b28985…
ph.ucla.edu/epi/snow/snowc…
blog.rtwilson.com/john-snows-cho…

30/ However, cholera was already in decline. The Board of Health refused to accept contaminated water, stating:
“we see no reason to adopt this belief [that cholera was water-borne]”
and dismissing Snow's conclusions as mere “suggestions"
google.com/books/edition/…
“we see no reason to adopt this belief [that cholera was water-borne]”
and dismissing Snow's conclusions as mere “suggestions"
google.com/books/edition/…
31/ The Board of Health had strong incentives for rejecting water as the source of cholera. To remove the sources of the miasma (filth), they had spearheaded the effort to build sewers that dumped raw sewage into the Thames, the source of much of London's drinking water...
32/ ...thus effectively helping the spread of cholera. They had much to lose by admitting cholera transmitted through water
[Technology has advanced, but human nature has changed less. @WHO has avoided saying LOUD & CLEAR that #COVIDisAirborne, as their denials helped it spread]
[Technology has advanced, but human nature has changed less. @WHO has avoided saying LOUD & CLEAR that #COVIDisAirborne, as their denials helped it spread]
@WHO 33/ Also around 1850, Ignaz Semmelweis in Vienna showed that handwashing greatly reduced deaths by childbed fever in a maternity clinic.
en.wikipedia.org/wiki/Ignaz_Sem…
en.wikipedia.org/wiki/Ignaz_Sem…

34/ These are some of Semmelweis' data, which would seem worth following up on:
However, his ideas conflicted with established medical and scientific beliefs that STILL described diseases as due to an imbalance of humors triggered by a miasma in the air.
doi.org/10.1556/650.20…
However, his ideas conflicted with established medical and scientific beliefs that STILL described diseases as due to an imbalance of humors triggered by a miasma in the air.
doi.org/10.1556/650.20…

35/ However, he was dismissed from his hospital and harassed by Vienna medical community, forced to move to Budapest. There he broke down, was interned and beaten by the guards, and ultimately died from an infected wound
Like Snow, he died years before his theories were accepted
Like Snow, he died years before his theories were accepted
36/ Ironically, Semmelweis' name lives on not only for advances of hand sanitation, but also in “Semmelweis reflex,” which describes the reflex-like tendency to reject new knowledge or evidence when it contradicts established beliefs, norms, or paradigms
en.wikipedia.org/wiki/Semmelwei…
en.wikipedia.org/wiki/Semmelwei…
37/ That is especially ironic, as the chief deniers of airborne transmission (John Conly -- chairman of key IPC @WHO committee, Dr. Seto, @DidierPittet,
@CollignonPeter) are handwashing experts...
... following Semmelweis' scientific advances, while forgetting about the reflex
@CollignonPeter) are handwashing experts...
... following Semmelweis' scientific advances, while forgetting about the reflex
38/ The 2nd half of the 19th Century is a period of rapid progress on disease transmission.
Pasteur and Koch proposed the GERM THEORY of disease. Microscopic germs enter the body and are the cause of many diseases.
en.wikipedia.org/wiki/Germ_theo…
worldcat.org/title/memoire-…

Pasteur and Koch proposed the GERM THEORY of disease. Microscopic germs enter the body and are the cause of many diseases.
en.wikipedia.org/wiki/Germ_theo…
worldcat.org/title/memoire-…


39/ Germ theory was NOT accepted overnight.
E.g. experiments by others in which water containing organic matter was boiled in a vessel, but microorganisms still appeared (later shown to be an imperfect seal or insufficient boiling) created controversy:
doi.org/10.1093/jhmas/…
E.g. experiments by others in which water containing organic matter was boiled in a vessel, but microorganisms still appeared (later shown to be an imperfect seal or insufficient boiling) created controversy:
doi.org/10.1093/jhmas/…
40/ However, by the late 1880s, miasma theory was waning in popularity, and in 1888, the Institut Pasteur was created in Paris, reflecting the ascendancy of germ theory.
pasteur.fr/en/institut-pa…
pasteur.fr/en/institut-pa…
41/ Florence Nightingale did accept the new ideas of germ theory, in fact before many physicians did.
E.g. in 1882, she wrote:
books.google.com/books?id=dDDcy…
E.g. in 1882, she wrote:
books.google.com/books?id=dDDcy…

42/ Initial results on plant pathogens in 1890s & the identification of bacteriophage in 1917 paved the way for recognition of viruses.
A “golden era” followed, with the identification of the actual microorganisms that cause many infectious diseases.
doi.org/10.1002/bies.2…
A “golden era” followed, with the identification of the actual microorganisms that cause many infectious diseases.
doi.org/10.1002/bies.2…
43/ The discovery and identification of the organisms causing different diseases did NOT, however, eliminate the great difficulty in conclusively determining the mode by which they transferred from one person to another.
Malaria was still thought to go through the air in 1880
Malaria was still thought to go through the air in 1880
44/ French physician Charles Laveran identified the pathogen responsible for malaria in 1880 (got Nobel Prize in 1907), but the manner of transmission was still thought to be through the air.
doi.org/10.1186/1475-2…
en.wikipedia.org/wiki/Charles_L…
doi.org/10.1186/1475-2…
en.wikipedia.org/wiki/Charles_L…

45/ American physician A. King proposed that malaria was transmitted by mosquitos, but encountered general skepticism
In 1883, he presented a list of 19 facts supporting m. as vector of malaria
[Reminds me of 10 scientific reasons for #COVIDisAirborne]
en.wikipedia.org/wiki/Albert_Fr…
In 1883, he presented a list of 19 facts supporting m. as vector of malaria
[Reminds me of 10 scientific reasons for #COVIDisAirborne]
en.wikipedia.org/wiki/Albert_Fr…

46/ In 1898 British surgeon R. Ross provided definitive evidence:
- confirming the presence of the malarial parasites in mosquitoes
- demonstrating transmission of bird malaria by mosquitoes
World Mosquito day commemorates him
doi.org/10.1186/1475-2…
en.wikipedia.org/wiki/Ronald_Ro…
- confirming the presence of the malarial parasites in mosquitoes
- demonstrating transmission of bird malaria by mosquitoes
World Mosquito day commemorates him
doi.org/10.1186/1475-2…
en.wikipedia.org/wiki/Ronald_Ro…
47/ Looking back at period 1850-1900, belief on transmission of many diseases through AIR was still strong
But cholera, malaria, puerperal fever had been shown to transmit OTHERWISE
It was a fluid time. It was debated if air was actually important
onlinelibrary.wiley.com/doi/10.1111/in…
But cholera, malaria, puerperal fever had been shown to transmit OTHERWISE
It was a fluid time. It was debated if air was actually important
onlinelibrary.wiley.com/doi/10.1111/in…

48/ In the 1890s, Carl Flügge in Germany set out to disprove the then-dominant transmission theory for tuberculosis, one of the major infectious diseases of the time. Most experts believed that tuberculosis was transmitted when dust of dried sputum that had landed on floors... 

49/ ...blankets, bowls, & other objects was dispersed into air. In contrast, Flügge thought that it was not DRIED secretions from sick that caused infection, but rather FRESH secretions that ppl were exposed to IN AIR BEFORE they reached the ground
doi.org/10.1098/rsfs.2…
doi.org/10.1098/rsfs.2…

50/ Some contemporaries of Flügge such as Cornet argued that tuberculosis was transmitted only through large droplets, which were easily visible to the naked eye.
Perhaps because droplets were more CONVENIENT and airborne disease VERY INCONVENIENT?
google.com/books/edition/…
Perhaps because droplets were more CONVENIENT and airborne disease VERY INCONVENIENT?
google.com/books/edition/…

51/ However, although term “Flügge's droplets” has been used to describe ONLY those large particles that fell to the ground quickly near the infected person and that were assumed to dominate transmission, that does NOT accurately capture Flügge's results
journals.sagepub.com/doi/10.1177/00…
journals.sagepub.com/doi/10.1177/00…
52/ Rather, Flügge and collaborators used the term “droplet” to refer to fresh particles of ALL SIZES, including AEROSOLS for which the researchers waited 5 hours to settle from the air on their collection plates.
doi.org/10.1098/rsfs.2…
doi.org/10.1098/rsfs.2…
53/ In 1905, microbiologist M.H. Gordon was commissioned to study the atmospheric hygiene of the UK House of Commons after an epidemic of influenza among members
He famously performed the following experiment: after gargling with a broth culture of Serratia marcescens...
He famously performed the following experiment: after gargling with a broth culture of Serratia marcescens...
54/ ... he loudly recited passages from Shakespeare in an empty House to an audience of agar plates. Although growth of colonies was more numerous on plates near the speaker, cultures were apparent on some plates over 21 m away.
bmj.com/content/4/5686…
bmj.com/content/4/5686…
55/ However, experimental progress in early 1900s was hampered by the limitations of the experimental techniques available at the time. In particular high-quality measurements of large droplets & aerosols would only be routinely available decades later.
onlinelibrary.wiley.com/doi/10.1111/in…
onlinelibrary.wiley.com/doi/10.1111/in…
56/ We get to the CRITICAL POINT of this history.
Throughout most of human history, the dominant belief was transmission of many diseases through the air.
The last half of the 19th Century proves otherwise for major diseases.
Strong debate ensues: "is air major or minor?"
Throughout most of human history, the dominant belief was transmission of many diseases through the air.
The last half of the 19th Century proves otherwise for major diseases.
Strong debate ensues: "is air major or minor?"

57/ Charles V. Chapin was a prominent American epidemiologist. He worked only a couple of decades after Germ Theory was accepted, during a period of intense research on pathogens & their transmission.
en.wikipedia.org/wiki/Charles_V…
en.wikipedia.org/wiki/Charles_V…

58/ The period when Chapin's worked on disease transmission was a fluid one, following a major paradigm shift, in which it was easier to change the dominant scientific discourse than during normal times
[See e.g. Kuhn en.wikipedia.org/wiki/The_Struc…]
[See e.g. Kuhn en.wikipedia.org/wiki/The_Struc…]
59/ He summarized the evidence of transmission of different diseases in his 1910 seminal book, “The Sources and Modes of Infection.”
[A must read if you are interested in this subject, esp. chapter on airborne transmission]
play.google.com/store/books/de…
[A must read if you are interested in this subject, esp. chapter on airborne transmission]
play.google.com/store/books/de…
60/ Chapin conceptualized “contact infection,” infection by germs that did NOT come from the environment, but from other PEOPLE through DIRECT CONTACT OR CLOSE PROXIMITY.
play.google.com/books/reader?i…
play.google.com/books/reader?i…

61/ Chapin believed contact was main mode of transmission of many diseases
But he encountered resistance: “I have sometimes been told I lay too much emphasis on contact infection [although] until recently very little attention has been paid to it.”
play.google.com/books/reader?i…
But he encountered resistance: “I have sometimes been told I lay too much emphasis on contact infection [although] until recently very little attention has been paid to it.”
play.google.com/books/reader?i…
62/ Chapin also reviewed the possibility of airborne infection, which he conceived especially as infections from afar. Lingering belief on air infection was making it difficult to promote contact infection:
play.google.com/books/reader?i…
play.google.com/books/reader?i…

63/ Chapin realized that airborne infection may explain infection in close proximity (CP). However, he argued that ease of infection in CP was better explained by “spray-borne” droplets, large visible droplets considered by Cornet
Same as @WHO's droplets:
Same as @WHO's droplets:
https://twitter.com/WHO/status/1244258441880797184
64/ This is the key. The evidence was insufficient, but Chapin turned absence of evidence into evidence of absence, and stated that airborne disease was almost impossible, and that "mouth spray" (large droplets) are only effective at short distances.
onlinelibrary.wiley.com/doi/10.1111/in…
onlinelibrary.wiley.com/doi/10.1111/in…

65/ As we have explained in another recent paper, Chapin conflates an empirical fact ("distance reduces transmission") with a mechanism: GRAVITY, which makes the droplets fall close to the infected person.
doi.org/10.1111/ina.13…
doi.org/10.1111/ina.13…
66/ Problem: the more correct explanation (of why distance reduces trans.) is NOT gravity but DILUTION:
Like exhaled smoke, you breathe less exhaled air farther from someone.
And error in PHYSICS made by MEDICAL professionals who do not study physics!
onlinelibrary.wiley.com/doi/10.1111/in…
Like exhaled smoke, you breathe less exhaled air farther from someone.
And error in PHYSICS made by MEDICAL professionals who do not study physics!
onlinelibrary.wiley.com/doi/10.1111/in…

67/ Despite the lack of evidence, Chapin was too successful.
He was much better positioned than Snow or Semmelweis as the long-serving Health Officer of Providence and w/ success of reducing contact transmission iin a new hospital. In 1927, he became President of @PublicHealth
He was much better positioned than Snow or Semmelweis as the long-serving Health Officer of Providence and w/ success of reducing contact transmission iin a new hospital. In 1927, he became President of @PublicHealth
68/ Chapin was described in 1967 as “the greatest American epidemiologist” by A. Langmuir, 1st & long-time director (1949–1969) of epidemiology branch of @CDCgov
As late as the 1980s, Chapin's views were dominant there.
doi.org/10.1093/aje/14…
en.wikipedia.org/wiki/Alexander…
As late as the 1980s, Chapin's views were dominant there.
doi.org/10.1093/aje/14…
en.wikipedia.org/wiki/Alexander…

69/ CRITICALLY, Chapin's unproven hypothesis was accepted as true:
Ease of infection in close proximity is accepted proof of transmission from sprayed droplets
This KEY ERROR conditioned the evolution of this field over the next century, and into the COVID-19 pandemic
Ease of infection in close proximity is accepted proof of transmission from sprayed droplets
This KEY ERROR conditioned the evolution of this field over the next century, and into the COVID-19 pandemic
69/ The 1918 flu led to lots of work and discussion in this area, but did not blunt the ascendance of of Chapin's theory:
onlinelibrary.wiley.com/doi/10.1111/in…
onlinelibrary.wiley.com/doi/10.1111/in…

70/ In the 1930s, Harvard engineering professor William Wells and physician Mildred Wells, his wife, started applying more contemporary experimental methods to the investigation of airborne transmission.
en.wikipedia.org/wiki/William_F…
en.wikipedia.org/wiki/William_F…

71/ But Chapin had successfully shifted the paradigm and his theory was now viewed as scientific progress.
The Wellses were accused of a retrograde approach to science, which sought to bring back the miasma theory.
jamanetwork.com/journals/jama/…
The Wellses were accused of a retrograde approach to science, which sought to bring back the miasma theory.
jamanetwork.com/journals/jama/…

72/ Wells was 1st to rigorously study size of sprayborne droplets vs. airborne aerosols
Conceptualized dichotomy of sprayborne droplets (≳100 μm), reach the ground before drying
Vs. aerosols (≲100 μm), dry before they reach ground ( “droplet nuclei”)
academic.oup.com/aje/article-ab…
Conceptualized dichotomy of sprayborne droplets (≳100 μm), reach the ground before drying
Vs. aerosols (≲100 μm), dry before they reach ground ( “droplet nuclei”)
academic.oup.com/aje/article-ab…

73/ Wells understood connection w/ meteorology where this is common knowledge, stating:
“A raindrop 2 mm in diameter can fall miles without completely evaporating under conditions which would cause a 0.2 mm droplet to evaporate before it had fallen from the height of a man.”
“A raindrop 2 mm in diameter can fall miles without completely evaporating under conditions which would cause a 0.2 mm droplet to evaporate before it had fallen from the height of a man.”

74/ Shockingly, Public Health and Infectious Diseases have published for decades that large droplets are those heavier than 5 microns (!!). Including in the latest @WHO Scientific Brief on COVID Transmission that addresses this issue: 

@WHO 75/ We pointed out this glaring error many times. I.e. see that even at 50 microns, they don't fall quickly:
Not too important per se, but makes glaringly obvious the ignorance of physics by those in charge at @WHO and its IPC committee.
Not too important per se, but makes glaringly obvious the ignorance of physics by those in charge at @WHO and its IPC committee.
https://twitter.com/MicroLevitator/status/1283556047471378432
76/ We investigated the history of the 5 micron / 2 meters error in a previous paper led by @linseymarr and the extraordinary @katierandall, with support from @EThomasEwing, Lydia Bourouiba of @MIT and yours truly:
royalsocietypublishing.org/doi/10.1098/rs…
royalsocietypublishing.org/doi/10.1098/rs…
77/ I am getting slightly out of order. I'll explain the reason for the "5 micron particles fall within the meters of the person" enormous error later in the thread, once I have explained the background.
So we were talking about the work of William Wells on airborne infection.
So we were talking about the work of William Wells on airborne infection.
78/ The Wellses suspected that tuberculosis and measles were airborne, but BOTH were already believed to be droplet diseases, and they encountered intense resistance from the epidemiological community.
79/ Measles was thought to be a droplet/fomite disease. At the time of Wells... and as late as 1985, because of:
- ease of transmission in close proximity (= sprayborne droplets per Chapin)
- cases of lack of infection w/ shared air
pediatrics.aappublications.org/cgi/pmidlookup…
- ease of transmission in close proximity (= sprayborne droplets per Chapin)
- cases of lack of infection w/ shared air
pediatrics.aappublications.org/cgi/pmidlookup…

80/ Wells thought that measles was airborne (and now we know he was correct, though he died 2 decades before this was accepted)
Wells has some initial success showing that UV lights installed in the ceiling of classrooms greatly reduced measles infection
ajph.aphapublications.org/doi/10.2105/AJ…
Wells has some initial success showing that UV lights installed in the ceiling of classrooms greatly reduced measles infection
ajph.aphapublications.org/doi/10.2105/AJ…

81/ However, subsequent attempts to replicate these findings produced mixed results.
In retrospect, in schools where UV prevented measles transmission, children were together indoors only in the school, not elsewhere. In other schools, children shared other spaces (e.g. buses)
In retrospect, in schools where UV prevented measles transmission, children were together indoors only in the school, not elsewhere. In other schools, children shared other spaces (e.g. buses)
82/ Wells established the scientific basis of airborne infection
But he was working in a period of intense hostility in public health and inf. diseases towards airborne tr., ushered by the success of the 1910 paradigm shift of Chapin after 2 millenia of belief in miasmas
But he was working in a period of intense hostility in public health and inf. diseases towards airborne tr., ushered by the success of the 1910 paradigm shift of Chapin after 2 millenia of belief in miasmas

83/ General skepticism against airborne tr. is illustrated by 1951 quote of Langmuir (first and longtime director of epidemiology @CDCgov) :
“It remains to be proved that airborne infection is an important mode of spread of naturally occurring disease"
jstor.org/stable/4587679
“It remains to be proved that airborne infection is an important mode of spread of naturally occurring disease"
jstor.org/stable/4587679
84/ Langmuir worked preventing disease trans. among US military in WW II
Substantial resources were dedicated to the effort, generating knowledge “which would have taken decades to accumulate under peacetime conditions” & established leaders for decades
doi.org/10.1093/aje/14…
Substantial resources were dedicated to the effort, generating knowledge “which would have taken decades to accumulate under peacetime conditions” & established leaders for decades
doi.org/10.1093/aje/14…
85/ Langmuir et al. studied airborne transmission, but MISINTERPRETED the results of their own studies:
Distance reduced transmission, therefore it was droplets. Ignoring that distance reduces airborne transmission by dilution.
doi.org/10.1093/aje/14…
doi.org/10.1111/ina.13…
Distance reduced transmission, therefore it was droplets. Ignoring that distance reduces airborne transmission by dilution.
doi.org/10.1093/aje/14…
doi.org/10.1111/ina.13…

86/ However, Langmuir's work renewed interest in airborne infection, as he concluded that WEAPONS of airborne disease could be created, which became a topic of intense interest during the cold war.
jstor.org/stable/4587679
jstor.org/stable/4587679
87/ Despite stubborn resistance to the idea that airborne transmission had relevance for natural diseases, Wells, Robert Riley [pic] & Cretyl Mills succeeded in demonstrating airborne transmission of tuberculosis (TB) in 1962 through extensive efforts
doi.org/10.1164/arrd.1…
doi.org/10.1164/arrd.1…

88/ They routed air from TB hospital ward to 150 guinea pigs (GP) for 2 yrs. ~3 GP / month were infected
No GP infected in control group where the only difference was that the air was irradiated with germicidal ultraviolet light, killing the TB bacterium
doi.org/10.1164/ajrccm…
No GP infected in control group where the only difference was that the air was irradiated with germicidal ultraviolet light, killing the TB bacterium
doi.org/10.1164/ajrccm…
89/ Because of this, TB was the first important natural disease to be accepted as airborne in modern times
It was shown that pulmonary TB can ONLY infect if bacterium-containing aerosols reach the alveoli, for which they need to be smaller than 5 microns
epa.gov/pmcourse/parti…
It was shown that pulmonary TB can ONLY infect if bacterium-containing aerosols reach the alveoli, for which they need to be smaller than 5 microns
epa.gov/pmcourse/parti…

90/ Here is when we think that the ERROR of "5 micron particles fall to the ground in 1-2 m" originated:
Only TB and bioweapons were important, someone at @CDCgov confused the size that goes to alveoli with size that falls to ground
Repeated till 2020
royalsocietypublishing.org/doi/10.1098/rs…
Only TB and bioweapons were important, someone at @CDCgov confused the size that goes to alveoli with size that falls to ground
Repeated till 2020
royalsocietypublishing.org/doi/10.1098/rs…
91/ The fascinating story of how @katierandall, @linseymarr et al. figured out the cause of the 5 micron error was told in this article in @WIRED by @MeganMolteni.
Reads like a spy novel, one of the best of the pandemic!
wired.com/story/the-teen…
Reads like a spy novel, one of the best of the pandemic!
wired.com/story/the-teen…
92/ In paper we characterize the years after the demonstration of TB as "Reluctant acceptance of as little airborne transmission as possible (1962–2020)"
Airborne disease was not impossible, but required an extremely high (undeniable) standard of proof.
onlinelibrary.wiley.com/doi/10.1111/in…
Airborne disease was not impossible, but required an extremely high (undeniable) standard of proof.
onlinelibrary.wiley.com/doi/10.1111/in…
93/ Unfortunately, standards of evidence were v. different for different routes of trans.
Many diseases accepted as “droplet” w/o any substantive proof—let alone extensive and time-consuming experiments
Only the hypothesis of Chapin, ease of infection in close prox. = droplets
Many diseases accepted as “droplet” w/o any substantive proof—let alone extensive and time-consuming experiments
Only the hypothesis of Chapin, ease of infection in close prox. = droplets
94/ Remember, large droplet transmission has NEVER been demonstrated DIRECTLY for ANY disease in the entire history of medicine
[Paper from Prof. Yuguo Li, lone airborne specialist in @WHO IPC Committee]
sciencedirect.com/science/articl…
[Paper from Prof. Yuguo Li, lone airborne specialist in @WHO IPC Committee]
sciencedirect.com/science/articl…

95/ An example of the resistance to airborne: an obvious case of long-distance airborne transmission of smallpox in Germany in 1970.
SP airborne trans. debated for centuries, only definitely accepted in the complete absence of community transmission
pubmed.ncbi.nlm.nih.gov/5313258/
SP airborne trans. debated for centuries, only definitely accepted in the complete absence of community transmission
pubmed.ncbi.nlm.nih.gov/5313258/

96/ An infected person arrived from Pakistan to Germany, where there were no cases at all.
Only possible explanation was transmission through air. In latter tests, smoke from index case room went to rooms of secondary cases.
academic.oup.com/aje/article-ab…
pubmed.ncbi.nlm.nih.gov/5313258/
Only possible explanation was transmission through air. In latter tests, smoke from index case room went to rooms of secondary cases.
academic.oup.com/aje/article-ab…
pubmed.ncbi.nlm.nih.gov/5313258/
97/ The case report shows the prevailing bias against airborne in Public Health:
“The only remaining route of transmission considered reasonable was airborne spread of a virus-containing aerosol, **a possibility against which all of the investigators were initially prejudiced**”
“The only remaining route of transmission considered reasonable was airborne spread of a virus-containing aerosol, **a possibility against which all of the investigators were initially prejudiced**”
98/ Measles and chickenpox were similar, described as droplet diseases till mid-1980s, and only accepted when superspreading events with long-distance transmission made airborne undeniable.
publications.aap.org/pediatrics/art…
nejm.org/doi/full/10.10…
publications.aap.org/pediatrics/art…
nejm.org/doi/full/10.10…

99/ Interestingly the @WHO IPC commitee members stated that COVID could not be airborne as it was much less transmissible than measles. Otherwise they would have recognized it quickly
Except... it took their profession 70 years to recognize it...
aricjournal.biomedcentral.com/articles/10.11…
Except... it took their profession 70 years to recognize it...
aricjournal.biomedcentral.com/articles/10.11…
100/ Note that it is always the same error, going back to Chapin.
Assuming that ease of transmission in close proximity (and decreasing transmission w/ distance) is proof of large droplets, and that airborne is very unlikely.
For TB, measles, chickenpox... and COVID-19
Assuming that ease of transmission in close proximity (and decreasing transmission w/ distance) is proof of large droplets, and that airborne is very unlikely.
For TB, measles, chickenpox... and COVID-19
101/ SARS-1 in 2003 brought renewed attention to airborne transmission
Superspreading was clearly observed. Airborne spread was implicated in several outbreaks in hospitals, and also in large Amoy Gardens outbreak in Hong Kong
doi.org/10.3201/eid100…
doi.org/10.1111/j.1600…
Superspreading was clearly observed. Airborne spread was implicated in several outbreaks in hospitals, and also in large Amoy Gardens outbreak in Hong Kong
doi.org/10.3201/eid100…
doi.org/10.1111/j.1600…
102/ Same dynamic played out for SARS-1:
- observed ease of infection in close proximity was considered evidence of droplet transmission
- airborne transmission was considered unlikely, and only accepted if evidence was undeniable
From IPC member:
sciencedirect.com/science/articl…
- observed ease of infection in close proximity was considered evidence of droplet transmission
- airborne transmission was considered unlikely, and only accepted if evidence was undeniable
From IPC member:
sciencedirect.com/science/articl…
103/ During last several decades, until the COVID-19 pandemic, with available antibiotics, vaccines, and no major respiratory pandemics, studies further probing the details of droplet vs. airborne transmission had NOT been a major public health priority.
onlinelibrary.wiley.com/doi/10.1111/in…
onlinelibrary.wiley.com/doi/10.1111/in…
104/ High standards of ventilation & filtration ain modern hospitals mean that airborne risks have been substantially mitigated in these settings, where many key infection control scientists work.
cdc.gov/infectioncontr…
techstreet.com/ashrae/standar….
cdc.gov/infectioncontr…
techstreet.com/ashrae/standar….
105/ Adherents of droplet transmission were in control of all key public health institutions.
Scientists proposing airborne transmission were typically ignored (as we saw later for COVID-19, and explaining persistence of errors)
royalsocietypublishing.org/doi/10.1098/rs…
wellcomeopenresearch.org/articles/6-126…
Scientists proposing airborne transmission were typically ignored (as we saw later for COVID-19, and explaining persistence of errors)
royalsocietypublishing.org/doi/10.1098/rs…
wellcomeopenresearch.org/articles/6-126…
106/ This schematic qualitatively captures the situation before COVID-19 appeared:
onlinelibrary.wiley.com/doi/10.1111/in…
onlinelibrary.wiley.com/doi/10.1111/in…

108/ Importantly, substantial scientific evidence had accumulated (BEFORE COVID) of airborne transmission of the flu, as reviewed in this paper in @ScienceMagazine (led by @ChiaWang8 and @kprather88):
science.org/doi/10.1126/sc…
science.org/doi/10.1126/sc…

109/ But the evidence of airborne transmission of the flu had been ignored, and @WHO and @CDCgov pages on the flu ONLY mention droplets & surfaces
who.int/news-room/fact…
cdc.gov/flu/about/dise…
who.int/news-room/fact…
cdc.gov/flu/about/dise…

110/ Airborne transmission is well accepted in veterinary medicine, including several coronaviruses and flu viruses.
And sometimes over many kilometers (facilitated by large animal concentrations)
Every veterinary I've talked to is dismayed about COVID
onlinelibrary.wiley.com/doi/10.1111/in…
And sometimes over many kilometers (facilitated by large animal concentrations)
Every veterinary I've talked to is dismayed about COVID
onlinelibrary.wiley.com/doi/10.1111/in…

111/ Finally we get to the COVID-19 pandemic. It is so massive and disruptive that every researcher that can contribute in some way gets to work doing so.
Includes lots of aerosol researchers (e.g. yours truly), with fast collaboration with medical researchers, virologists etc.
Includes lots of aerosol researchers (e.g. yours truly), with fast collaboration with medical researchers, virologists etc.
112/ Some early scientific and public health reports out of China state that COVID-19 has airborne transmission:
doi.org/10.1038/s41586…
bbc.com/zhongwen/simp/…
doi.org/10.1038/s41586…
bbc.com/zhongwen/simp/…
113/ Despite a lack of direct evidence in favor of droplet or fomite transmission of COVID, by Mar 2020 @WHO concluded that ease of transmission in close proximity proved that COVID-19 was transmitted by those mechanisms, continuing Chapin's 1910 error
https://twitter.com/who/status/1243972193169616898
114/ The same errors described for other diseases are repeated for COVID-19. And the bar is moved higher: unlike TB, animal transmission is not enough. Unlike measles, superspreading and long-distance transmission is not enough...
onlinelibrary.wiley.com/doi/10.1111/in…
onlinelibrary.wiley.com/doi/10.1111/in…

115/ However, accumulating evidence in favor of airborne, and critical LACK of evidence for droplets or surfaces tilts the balance
Airborne transmission is (reluctantly and slowly) accepted.
E.g. one summary of evidence for #COVIDisAirborne:
Airborne transmission is (reluctantly and slowly) accepted.
E.g. one summary of evidence for #COVIDisAirborne:
https://twitter.com/jljcolorado/status/1383566908797059078
116/ @WHO commissioned some reviews on the modes of transmission of COVID-19. The one on airborne included no airborne experts, and has been rejected by the reviewers:
f1000research.com/articles/10-23…
f1000research.com/articles/10-23…

116/ Shockingly, no review has appeared (to my knowledge) on the evidence in favor of large droplet transmission, despite @WHO being so sure for a long time that it was dominant.
117/ A @WHO-sponsored review has been written on "close contact transmission" == "close proximity".
But that is a measurement of distance, NOT a mechanism of transmission!
Still carrying the error of Chapin, confusing close proximity w/ spray droplets
f1000research.com/articles/10-280
But that is a measurement of distance, NOT a mechanism of transmission!
Still carrying the error of Chapin, confusing close proximity w/ spray droplets
f1000research.com/articles/10-280
118/ That @WHO-sponsored review on close prox. transmission has also NOT been accepted for publ., and remains in limbo after over a year
Even though THEY GET TO CHOOSE REVIEWERS!
Read the comments that we posted on both articles:
f1000research.com/articles/10-280
f1000research.com/articles/10-23…
Even though THEY GET TO CHOOSE REVIEWERS!
Read the comments that we posted on both articles:
f1000research.com/articles/10-280
f1000research.com/articles/10-23…
119/ "Aerosol-generating medical procedures" were the only accepted cause of airborne transmission for over a year (e.g. by @WHO).
They originated from low-quality research in SARS-1. Research has show that real AGPs are talking, singing...
onlinelibrary.wiley.com/doi/10.1111/in…
They originated from low-quality research in SARS-1. Research has show that real AGPs are talking, singing...
onlinelibrary.wiley.com/doi/10.1111/in…

120/ @WHO has finally accepted airborne transmission, including the fact that transmission in close proximity includes short-range airborne transmission.
But only in Dec. 2021, after we pushed them a lot.
But only in Dec. 2021, after we pushed them a lot.

121/ But both @WHO and @CDCgov communicate poorly about this, not explaining it to the public, and avoiding the word "airborne" (which is the clearest for the public) as much as they can
E.g. no mention of airborne COVID in @WHO's extensive Twitter feed:
twitter.com/search?q=airbo…
E.g. no mention of airborne COVID in @WHO's extensive Twitter feed:
twitter.com/search?q=airbo…
122/ And especially no clear description of the control measures. As @kprather88 keeps saying, it is totally doable to majorly reduce transmission, once we accept it and get serious about it.
But it is a really inconvenient truth for those in power...
But it is a really inconvenient truth for those in power...
https://twitter.com/jljcolorado/status/1562118493520072704
123/ My pinned tweet has a good summary of those protection measures against transmission (also in many other sources such as @CleanAirCrewOrg, or the @CDCgov web pages if you actually read them in detail):
https://twitter.com/jljcolorado/status/1463200650494316550
123/ So where does that leave us in mid-2022:
- PH institutions such as @CDCgov have given up on explaining or preventing transmission. Too inconvenient for those in power
- Scientifically, cat is out of bag. Tons of evidence of airborne, some medical & PH ppl understand it
- PH institutions such as @CDCgov have given up on explaining or preventing transmission. Too inconvenient for those in power
- Scientifically, cat is out of bag. Tons of evidence of airborne, some medical & PH ppl understand it
124/ - Measures to improve ventilation are favored (e.g. by the @WhiteHouse) since they don't face resistance from public, but they are inconsistently applied.
- CO2 meters are resisted by institutions, because they make poor ventilation obvious.
whitehouse.gov/ostp/news-upda…
- CO2 meters are resisted by institutions, because they make poor ventilation obvious.
whitehouse.gov/ostp/news-upda…

125/ Not sure how this will evolve. But as it becomes scientifically clearer, it will be harder to justify lack of action
But as we know from climate change (follow twitter.com/i/lists/105306…), the sci. evidence can be overwhelming & those in power still resist inconvenient actions
But as we know from climate change (follow twitter.com/i/lists/105306…), the sci. evidence can be overwhelming & those in power still resist inconvenient actions
126/ This is the final (hopeful) paragraph of this historical paper.
Wells lamented in 1945 the ignorance of airborne transmission in PH (jstor.org/stable/18316#m…)
Let's hope that ends with COVID-19 (& fight to make it reality - we need to be activists)
onlinelibrary.wiley.com/doi/10.1111/in…
Wells lamented in 1945 the ignorance of airborne transmission in PH (jstor.org/stable/18316#m…)
Let's hope that ends with COVID-19 (& fight to make it reality - we need to be activists)
onlinelibrary.wiley.com/doi/10.1111/in…

127/ I didn't do this alone. I got involved in COVID-19 transmission research in early 2020, and was shocked and confused by the stubborn and impatient resistance we faced.
E.g. Conly's (@WHO IPC Chair) rudeness on our Apr. 2020 call w/ @WHO]
wired.com/story/the-teen…
E.g. Conly's (@WHO IPC Chair) rudeness on our Apr. 2020 call w/ @WHO]
wired.com/story/the-teen…

128/ I've been lucky to work with the Morawska/@Don_Milton group of 36 scientists & with many others
@Don_Milton made me curious about history, mentioning Chapin and his impact. I was perplexed an "ancient" researcher could influence @WHO advisors today so much. Started reading
@Don_Milton made me curious about history, mentioning Chapin and his impact. I was perplexed an "ancient" researcher could influence @WHO advisors today so much. Started reading
129/ As we investigated many aspects of transmission, I kept an eye on the history. The paper on the 5 micron error with @katierandall and @linseymarr made me learn a lot, and also see more clearly the pendulum of history: 

130/ Contributors to the paper include @linseymarr @katierandall @EThomasEwing @zeynep @trishgreenhalgh Raymond Tellier, Julian Tang, Yuguo Li, Lidia Morawska, @jmcrookston @DFisman @Orla_Hegarty Stephanie Dancer, Philo Bluyssen, Giorgio Buonanno, @Marcel_Loomans @WBahnfleth...
131/ [Authors continued] @pkubioaerosol Chandra Shekhar @WargockiPawel Arsen Kritov Melikov and @kprather88
The authors contributed majorly to the paper. If there are any remaining mistakes, they are mine.
The authors contributed majorly to the paper. If there are any remaining mistakes, they are mine.
132/ As always, if you think that something is incorrect, or if you have a paper that contradicts (or further supports) anything I am saying here or in the paper, please send it my way
133/ My apologies that I have been pretty absent from Twitter for several months. We have had a bit of travel, and had a major field study this summer and that consumed a lot of bandwidth. 

134/ Thanks to @kprather88 this history paper has an illustrious reader on Dr. Fauci.
https://twitter.com/kprather88/status/1562234936735965188?t=84swDrNJ8WQ1HHvTyhX2xA&s=19
135/ Someone asked about why we did not cover the understanding of transmission in East Asia.
We were curious about it, also in Eastern Europe during cold war, both seemed more favorable to airborne.
There is clearly material for many papers there (send me any you find)
We were curious about it, also in Eastern Europe during cold war, both seemed more favorable to airborne.
There is clearly material for many papers there (send me any you find)
136/ But in investigating the history, it seemed that the denial and resistance of #COVIDisAirborne, led by @WHO and @CDCgov, was rooted in Western science and the Chapin error. So we focused on that in this paper.
See this text on paper (Methods):
onlinelibrary.wiley.com/doi/10.1111/in…
See this text on paper (Methods):
onlinelibrary.wiley.com/doi/10.1111/in…

137/ There is an important typo on tweet #122.
The @WhiteHouse document came out in Mar-2022, NOT 2020 as the slide erroneously showed (things could have been very different in that case! ALthough @CDCgov has just ignored this @WhiteHouse doc)
Thxto Lin & @kprather88 for catch
The @WhiteHouse document came out in Mar-2022, NOT 2020 as the slide erroneously showed (things could have been very different in that case! ALthough @CDCgov has just ignored this @WhiteHouse doc)
Thxto Lin & @kprather88 for catch

138/ When the American Thoracic Society is re-tweeting our work, I have hope that change may come
Change on airborne trans. will NOT happen (or REALLY slow) unless medicine / public health pushes
Thanks @atscommunity! [& Understood RT is NOT endorsement]
Change on airborne trans. will NOT happen (or REALLY slow) unless medicine / public health pushes
Thanks @atscommunity! [& Understood RT is NOT endorsement]
https://twitter.com/atscommunity/status/1562877617065574401
139/ BTW I forgot to thank @numeroteca for lots of help with the key figure on the paper (below)
And other Twitter users that helped me polish it online on this thread:
And other Twitter users that helped me polish it online on this thread:
https://twitter.com/jljcolorado/status/1485686803336085507(& another I can't find)

140/ I wrote SHORTER thread explaining larger picture of REASONS FOR RESISTANCE AND DENIAL OF #COVIDisAirborne by @WHO @CDCgov @sanidadgob & PH, governments, & corporations in general
TDLR: history set us up, but key: AIRBORNE IS INCONVENIENT TO POWER
TDLR: history set us up, but key: AIRBORNE IS INCONVENIENT TO POWER
https://twitter.com/jljcolorado/status/1562504871340679169
• • •
Missing some Tweet in this thread? You can try to
force a refresh










