🚨🚨🚨New @EuroRespSoc @escardio #PulmonaryHypertension guidelines 2022
There is a lot of new guidance, this is just a short thread to begin with the most notable changes...
Let's go! 🧵 👇👇👇 (1/10)
There is a lot of new guidance, this is just a short thread to begin with the most notable changes...
Let's go! 🧵 👇👇👇 (1/10)
1⃣New definition:
📌Same mPAP threshold as Nice 2018 (mPAP> 20 mmHg)
📌Lower PVR threshold (PVR >2 WU)! 👈
📌No more DPG to differentiate Ipc & Cpc
📌Re-introduction of #ExercisePH in definition!👈
(2/10)
📌Same mPAP threshold as Nice 2018 (mPAP> 20 mmHg)
📌Lower PVR threshold (PVR >2 WU)! 👈
📌No more DPG to differentiate Ipc & Cpc
📌Re-introduction of #ExercisePH in definition!👈
(2/10)

2⃣Diagnostic algorithm:
📌Fast track for referral to a #PH centre at any point of warning signs or #PAH or #CTEPH suspected
📌Individualised route for suspected #LungDisease but rapid cross-referral if necessary
📌If eventually PAH/CTEPH suspected, follow to tables 😵💫
(3/10)


📌Fast track for referral to a #PH centre at any point of warning signs or #PAH or #CTEPH suspected
📌Individualised route for suspected #LungDisease but rapid cross-referral if necessary
📌If eventually PAH/CTEPH suspected, follow to tables 😵💫
(3/10)



3⃣Risk stratification:
📌3-strata: fundamentally similar to previous ➡️to be used at initial evaluation
📌4-strata: identifies intermediate-low & intermediate-high categories ➡️to be used at follow-up
(4/10)

📌3-strata: fundamentally similar to previous ➡️to be used at initial evaluation
📌4-strata: identifies intermediate-low & intermediate-high categories ➡️to be used at follow-up
(4/10)


4⃣New #treatment algorithm (1/2):
📌3-strata risk assessment for initial evaluation, but 4-strata risk for follow up 🤔
👉At initial evaluation:
📌Only patients with 🫀or🫁comorbidities (any risk) ➡️initial monotherapy
📌Low-interm risk w/out comorb ➡️PDE5i + ERAs
(5/10)
📌3-strata risk assessment for initial evaluation, but 4-strata risk for follow up 🤔
👉At initial evaluation:
📌Only patients with 🫀or🫁comorbidities (any risk) ➡️initial monotherapy
📌Low-interm risk w/out comorb ➡️PDE5i + ERAs
(5/10)

4⃣New #treatment algorithm (2/2):
👉At follow-up:
📌Low risk: continue
📌Intermediate-low (4-strata!): add prostacyclin-R antagonists or switch PDE5-i ➡️sGCS
📌Intermediate-high or high: add parenteral prostacyclin &/or #LungTransplant referral
(6/10)
👉At follow-up:
📌Low risk: continue
📌Intermediate-low (4-strata!): add prostacyclin-R antagonists or switch PDE5-i ➡️sGCS
📌Intermediate-high or high: add parenteral prostacyclin &/or #LungTransplant referral
(6/10)

5⃣Definition of a PH centre:
📌Skills & facilities required in a PH specialist centre
📌Definition of the processes involved for the care of #PH patients
📌Recommendation to connect w #PatientAssociation!
🎯Focus on the structure of care ensures appropriate management👈
(7/10)

📌Skills & facilities required in a PH specialist centre
📌Definition of the processes involved for the care of #PH patients
📌Recommendation to connect w #PatientAssociation!
🎯Focus on the structure of care ensures appropriate management👈
(7/10)


6⃣Many other new changes in specific settings:
📌CTEPH treatment w BPA mostly after medical therapy in inoperable pts
📌New classification of hemodynamic severity in Group 3 PH: PVR>5 WU! 👈
📌More detailed recommendations for the management of vasodilator tests & CCB+ pts
(8/10)


📌CTEPH treatment w BPA mostly after medical therapy in inoperable pts
📌New classification of hemodynamic severity in Group 3 PH: PVR>5 WU! 👈
📌More detailed recommendations for the management of vasodilator tests & CCB+ pts
(8/10)



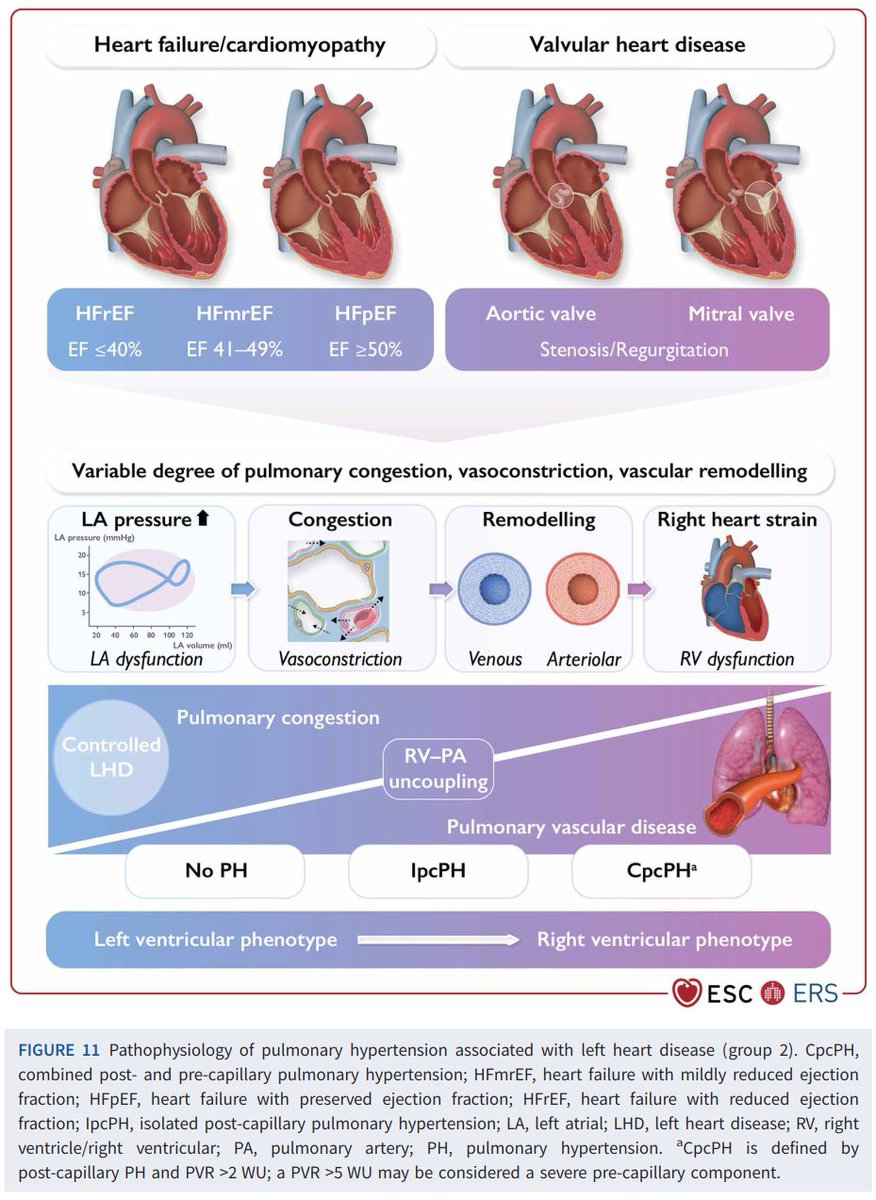
7⃣In general, the new guidelines are a trove of useful insights into physiopathology, guidance in >> detail than previous documents, tables & fantastic images, which obviously took a lot of work!
It will take a while to digest all this 😅
The visual style greatly helps!
(9/10)



It will take a while to digest all this 😅
The visual style greatly helps!
(9/10)



With all this new ideas in the air, see you at #ERS2022!
@SandeepSahayMD @AlbertaPHdoc @VituloP @LichtblauMD @Sheilaramjug @RRVdpool @PenateGregorio @AlbertoGaOrtega @PVRI @EuroRespSoc @atscommunity @ATS_PC @SeparCPulmonar
(10/FIN)
@SandeepSahayMD @AlbertaPHdoc @VituloP @LichtblauMD @Sheilaramjug @RRVdpool @PenateGregorio @AlbertoGaOrtega @PVRI @EuroRespSoc @atscommunity @ATS_PC @SeparCPulmonar
(10/FIN)

• • •
Missing some Tweet in this thread? You can try to
force a refresh








