There are a lot of jargon words in #neurology. As a student, I felt particularly confused by the words clonus, myoclonus, and asterixis, so I made this #tweetorial for learners who feel like I did.
#MedTwitter #MedEd #medicalschool #neurotwitter
#MedTwitter #MedEd #medicalschool #neurotwitter
Clonus is RHYTHMIC involuntary muscle contractions. It's caused by lesions to the pyramidal tract (ie UMN). It's likely due to exquisitely hyperreflexic muscle stretch reflexes - basically the muscle contraction triggers itself to keep firing in a feedback loop. 
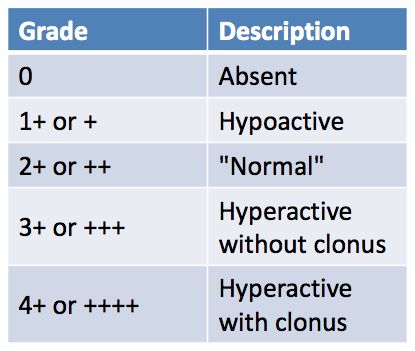
An easy way to check for clonus is by rapidly plantarflexing the foot, but you can sometimes see clonus just by checking muscle stretch reflexes.
Sustained clonus is defined as > 10 consecutive beats, but both sustained and unsustained clonus are generally pathologic in adults.
Sustained clonus is defined as > 10 consecutive beats, but both sustained and unsustained clonus are generally pathologic in adults.
Myoclonus, on the other hand, is NONRHYTHMIC, involuntary, brief muscle contractions.
Myoclonus can be primary (e.g. hereditary essential myoclonus) or secondary to medications/epilepsy, etc. The etiology is unfortunately pretty complex and outside the scope of this lesson.
Myoclonus can be primary (e.g. hereditary essential myoclonus) or secondary to medications/epilepsy, etc. The etiology is unfortunately pretty complex and outside the scope of this lesson.
Interestingly, myoclonus can be completely normal.
Ever do that sudden jerk right when you're falling asleep? Myoclonus.
Even hiccups are just a kind of myoclonus.
Ever do that sudden jerk right when you're falling asleep? Myoclonus.
Even hiccups are just a kind of myoclonus.
Asterixis is that hand-flapping thing cirrhotics get, right?
Well, yeah, but it's actually much simpler than that: asterixis is just negative myoclonus.
Well, yeah, but it's actually much simpler than that: asterixis is just negative myoclonus.
It tends to occur with global metabolic issues such as cirrhosis (hyperammonemia) and renal failure (hyperuremia). Muscle tone is lost due to what's basically a transient "dropped call" from the brain.
Look for asterixis in movements that require sustained flexion or extension: firmly gripping your hand, walking, or holding the wrists in extension.
As you can see, while the three terms are related, they are very different in terms of their presentation and meaning:
* Clonus: rhythmic. Super-hyperreflexia. UMN lesion.
* Myoclonus: irregular rapid jerks. Wide ddx.
* Asterixis: negative myoclonus. Metabolic derangements.
* Clonus: rhythmic. Super-hyperreflexia. UMN lesion.
* Myoclonus: irregular rapid jerks. Wide ddx.
* Asterixis: negative myoclonus. Metabolic derangements.
• • •
Missing some Tweet in this thread? You can try to
force a refresh








