Very happy that this work is finally out in a peer reviewed journal: @NatureComms
“Household transmission of the SARS-CoV-2 Omicron variant in Denmark”
Read it here: nature.com/articles/s4146…
A short thread with the new/updated results.
1/
“Household transmission of the SARS-CoV-2 Omicron variant in Denmark”
Read it here: nature.com/articles/s4146…
A short thread with the new/updated results.
1/

We investigate the secondary attack rate (SAR) in households infected with #SARSCoV2 #Omicron vs #Delta in Demark, 9-22 December 2021.
2/
2/

Conclude:
Omicron has a higher SAR than Delta. While vaccination and booster vaccination does confer protection against Omicron, we conclude that the rapid spread of Omicron is likely due to immune evasiveness and to a lower extent an increase in the basic transmissibility.
3/
Omicron has a higher SAR than Delta. While vaccination and booster vaccination does confer protection against Omicron, we conclude that the rapid spread of Omicron is likely due to immune evasiveness and to a lower extent an increase in the basic transmissibility.
3/
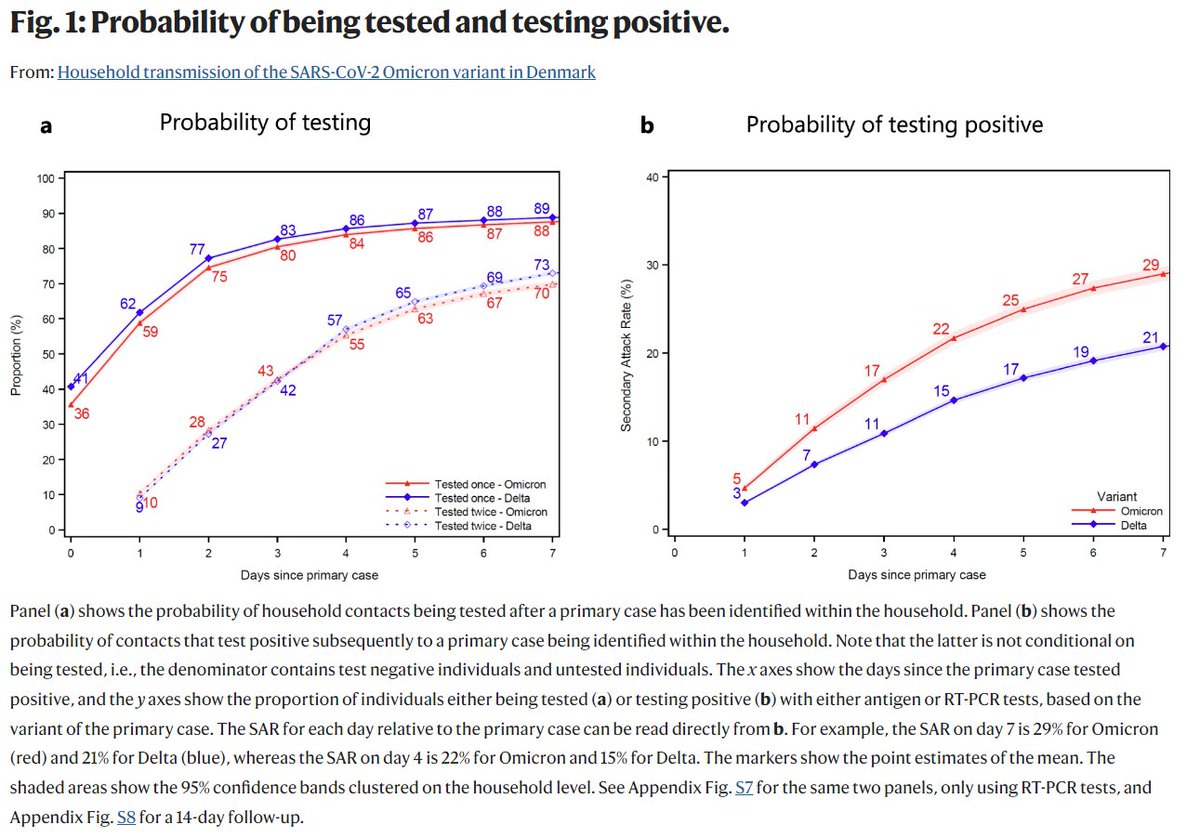
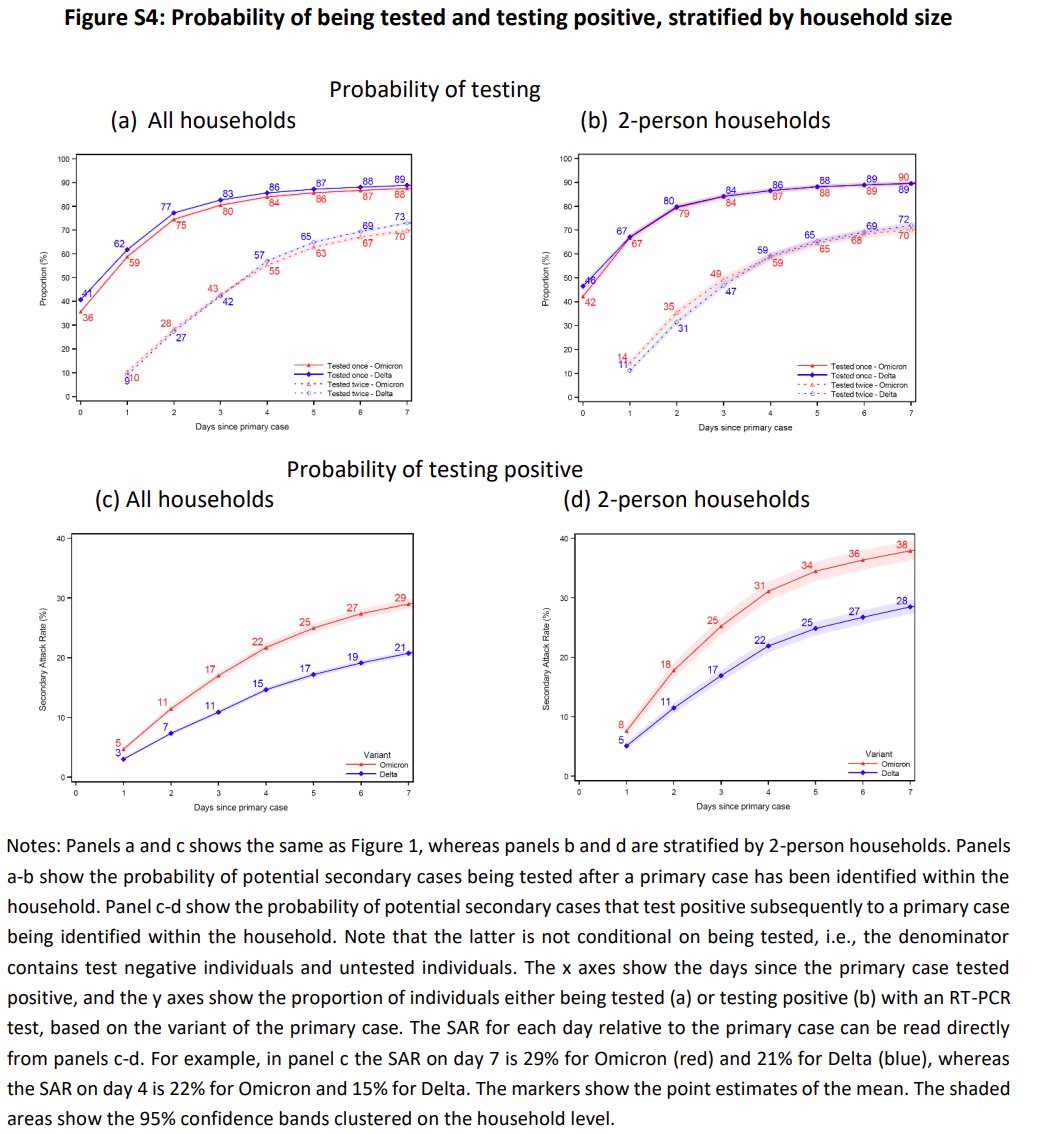
We found an overall secondary attack rate (SAR) of 31% in households infected with Omicron and 21% in households infected with Delta (Figure 1,b).
4/
4/
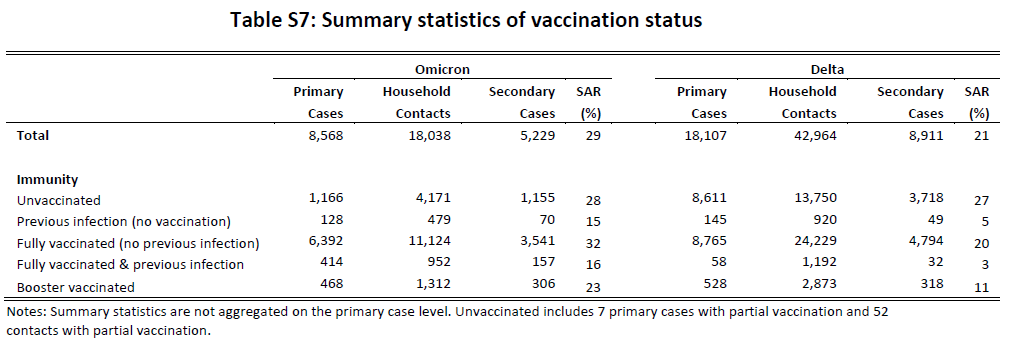
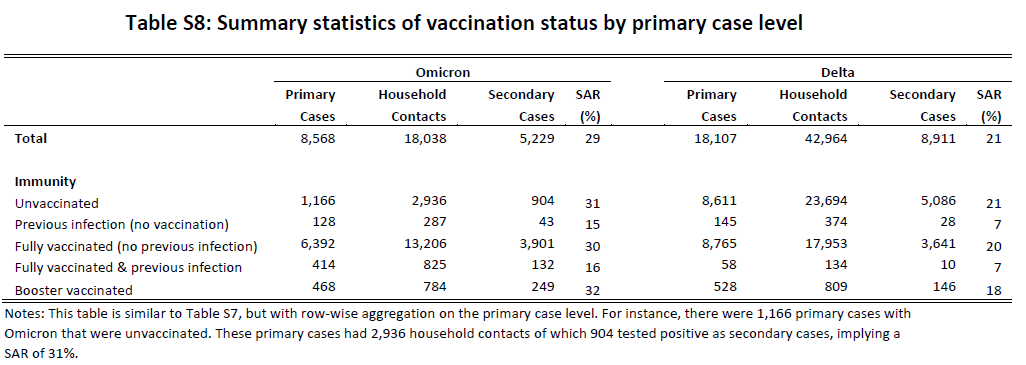
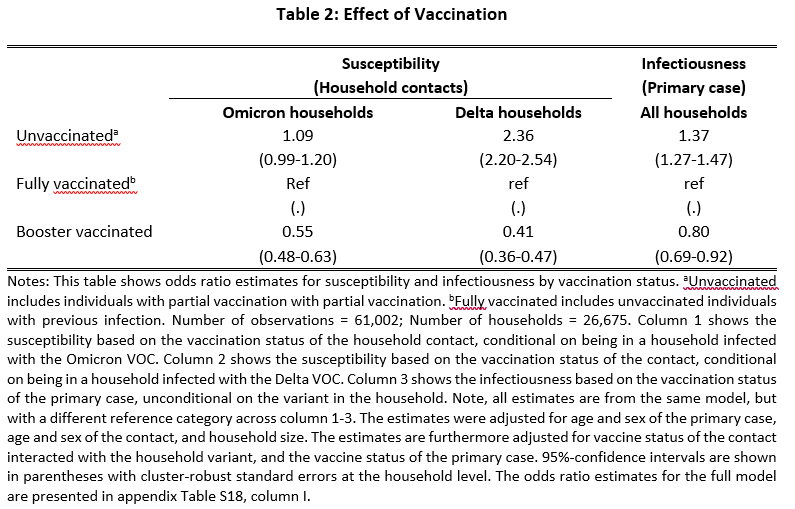
Unvaccinated individuals are more susceptible and more infectious, while booster-vacc. are less susceptible and less infectious, compared to fully vacc. individuals.
This demonstrates a baseline association between vacc. status and both susceptibility and infectiousness.
5/
This demonstrates a baseline association between vacc. status and both susceptibility and infectiousness.
5/
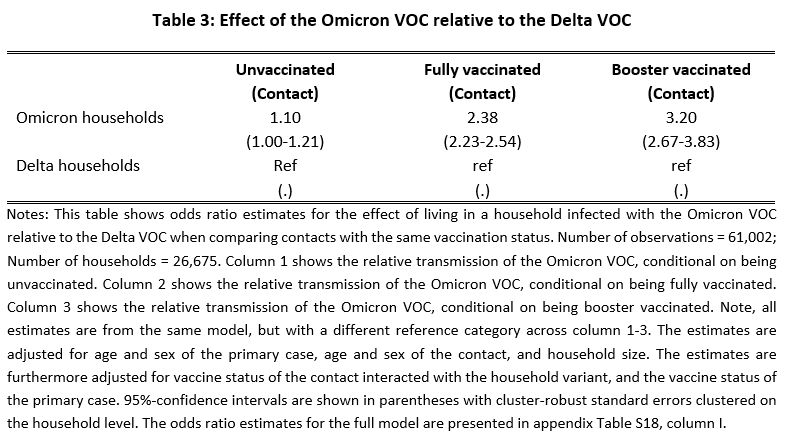
Next, we compare the relative SAR of household contacts with the same vaccination status across households infected with Omicron and Delta.
This indicates that Omicron has a higher immune evasiveness compared to Delta.
6/
This indicates that Omicron has a higher immune evasiveness compared to Delta.
6/
We have included a series of additional summary statistics and and robustness checks in the supplementary Information (appendix): static-content.springer.com/esm/art%3A10.1…
7/
7/
One of the main potential weaknesses of our approach is the assumption that primary and secondary cases are classified correctly, i.e., that the presumed within-household transmission did in fact occur from primary to secondary household cases.
8/
8/
There are three overall concerns with misclassifications:
1) Tertiary cases could be misclassified as secondary cases
2) Misclassification of primary cases
3) Secondary cases are identified as being infected in the household, but are in fact infected by the outside community
9/
1) Tertiary cases could be misclassified as secondary cases
2) Misclassification of primary cases
3) Secondary cases are identified as being infected in the household, but are in fact infected by the outside community
9/
1)Misclassification of tertiary cases as secondary cases
Tertiary cases could in theory be misclassified as secondary cases. If one variant has a shorter serial interval time, this could lead to a difference in the misclassification that is correlated with the variant.
10/
Tertiary cases could in theory be misclassified as secondary cases. If one variant has a shorter serial interval time, this could lead to a difference in the misclassification that is correlated with the variant.
10/
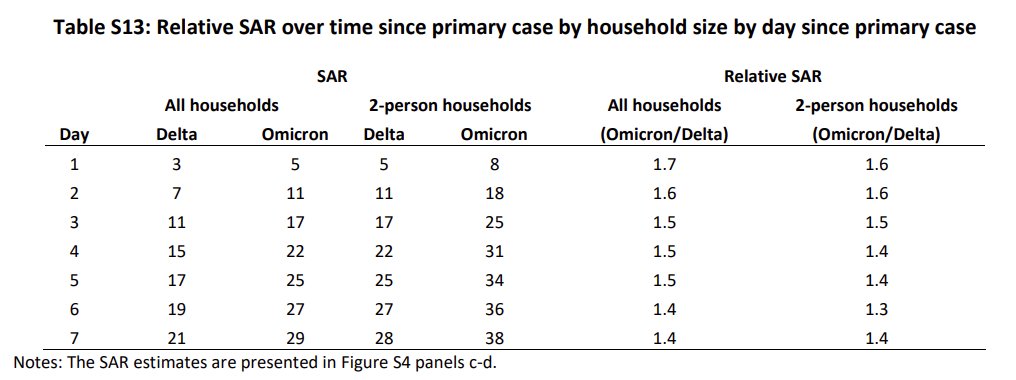
To address this, we compare the relative SAR in 2-person vs. multi-person households.
If the increased serial interval for Omicron implied more tertiary cases, we should see an increased difference in the relative SAR over time for households with more than two members.
11/
If the increased serial interval for Omicron implied more tertiary cases, we should see an increased difference in the relative SAR over time for households with more than two members.
11/
2)Misclassification of primary cases
Correct identification of primary cases within the household is important for this study as this determines whether the household is counted as an Omicron or Delta household when assessing the effect of the VOC on transmission.
13/
Correct identification of primary cases within the household is important for this study as this determines whether the household is counted as an Omicron or Delta household when assessing the effect of the VOC on transmission.
13/
In theory the first identified case, i.e., the index case, may not be the primary case of a household transmission chain.
14/
14/
In our setting, we use the timing of tests and test results to classify cases. This could be an issue, if for example vaccination status and/or symptoms are correlated with the likelihood of being tested.
15/
15/
Overall, we can classify the relevant household contacts into five types by their observed tests and test results from two tests within 7 days of exposure:
16/
16/
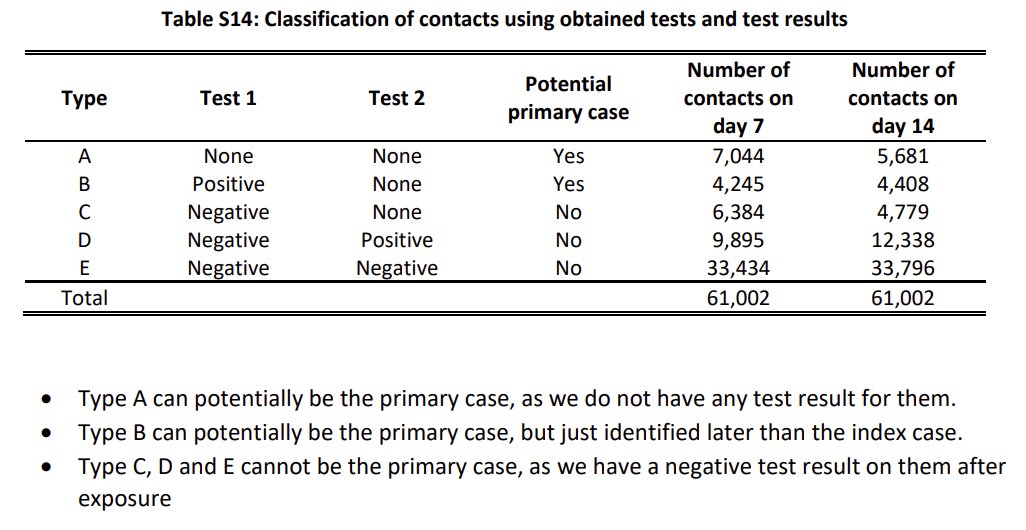
This leaves us with a subsample of 72% of all households and 68% of all contacts.
Using this sub-sample, we estimate our full regression model again. The estimates are relatively robust to this sub-sampling.
17/
Using this sub-sample, we estimate our full regression model again. The estimates are relatively robust to this sub-sampling.
17/
3)Misclassification of community cases as secondary household cases
Secondary cases could in theory be infected by the outside community and not the household and therefore be misclassified as secondary household cases.
18/
Secondary cases could in theory be infected by the outside community and not the household and therefore be misclassified as secondary household cases.
18/
To address this potential concern of misclassification, we first investigate the probability that secondary cases are infected with the same variant as the primary case.
Overall, 97.5% of secondary cases were infected with the same variant as the primary case.
19/
Overall, 97.5% of secondary cases were infected with the same variant as the primary case.
19/
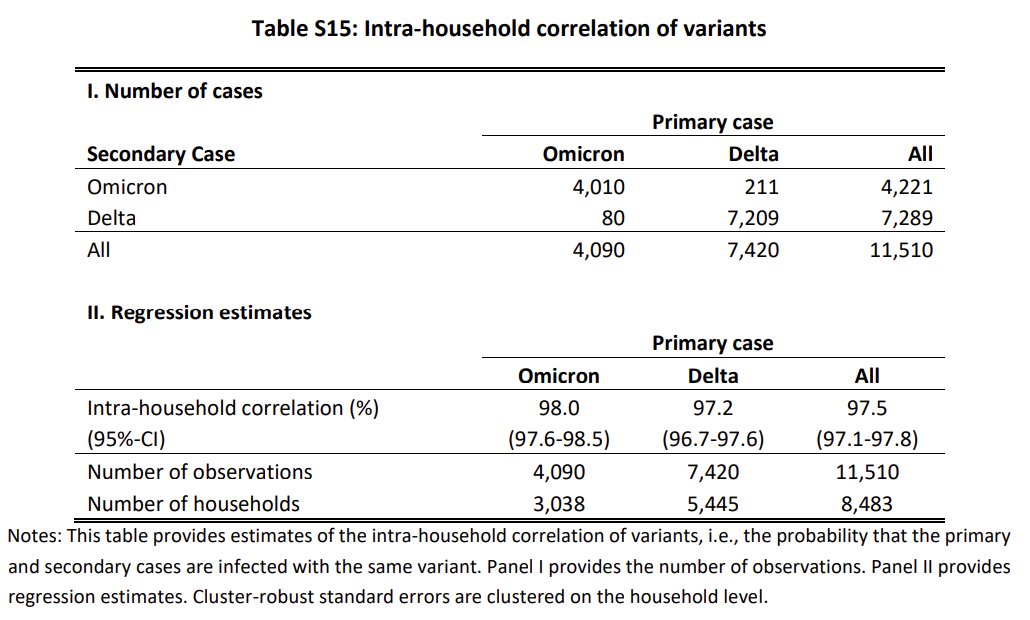
This measure is, however, a necessary—but not sufficient—condition.
20/
20/
If the local geographic neighborhood is primarily infected with one variant and that is the same as within the household, we would not be able to separate secondary cases infected in the household from those infected in the local community based on the variant.
21/
21/
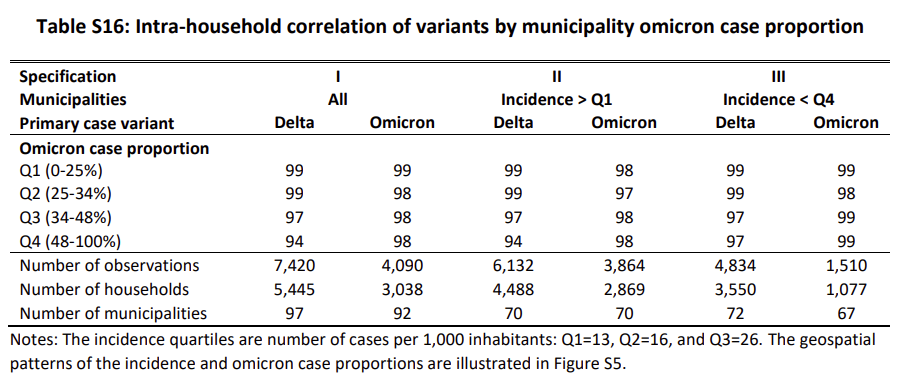
However, for households infected with a different variant from that which is dominant in the neighborhood, we can in fact gauge the role of misclassified community infections.
22/
22/
We can follow households infected with Omicron that are surrounded by a neighborhood with Delta.
Here, we would expect the secondary cases to be infected with Omicron, if they were infected in the household, and infected with Delta, if they were infected in the community.
23/
Here, we would expect the secondary cases to be infected with Omicron, if they were infected in the household, and infected with Delta, if they were infected in the community.
23/
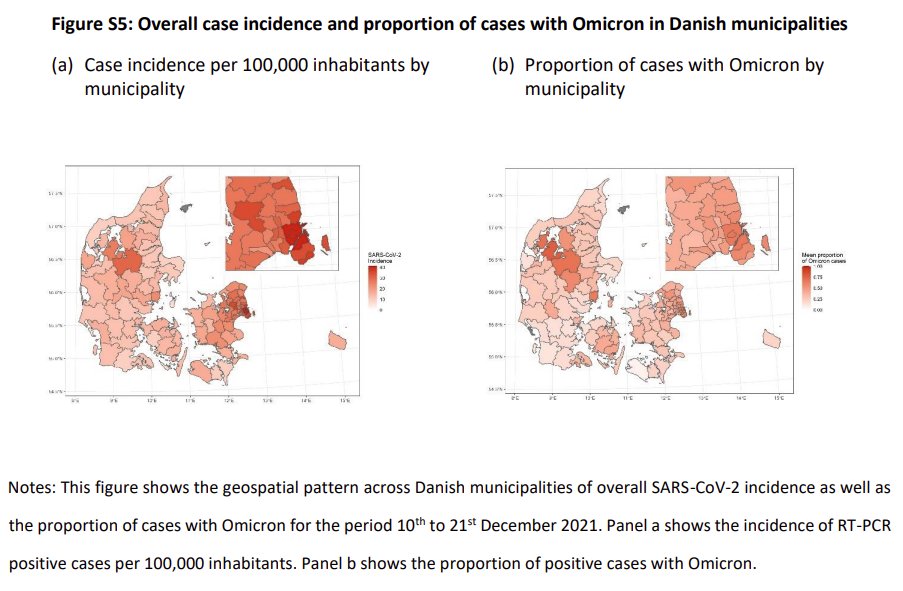
The spatial distribution of Omicron and Delta shows that we have support across almost all municipalities in Denmark.
24/
24/
The highest misclassification was due to community infection for households infected with the Delta VOC that were located in municipalities with a high Omicron incidence, where we found that 94% of secondary cases were infected with the same variant as the primary case.
25/
25/
In conclusion: We found limited evidence of misclassification of primary and secondary cases distorting our results.
26/
26/
Thanks to great co-authors and a bunch of anonymous reviewers.
@CarstenKirkeby @udansk @KareMolbak @TyraGroveKrause @mobdjek @MarcStegger @RskSkov
@Economics_UCPH @CEBI_UCPH @SSI_dk @UCPH_health
@CarstenKirkeby @udansk @KareMolbak @TyraGroveKrause @mobdjek @MarcStegger @RskSkov
@Economics_UCPH @CEBI_UCPH @SSI_dk @UCPH_health
Link to original thread with results from our preprint:
https://twitter.com/LyngseF/status/1476223591138140167?fbclid=IwAR01KKC-cyvfnm9Be9SIqFTOTKNVakOkBzMumJag3JTKUs2i9v04_Rjkfzc
A short appendix note on pooling of groups.
-We pool previously infected with fully vaccinated.
-We pool partially vaccinated with unvaccinated.
This is, e.g., described in the Methods section and in Tables 1+2 in the main article.
A1/
-We pool previously infected with fully vaccinated.
-We pool partially vaccinated with unvaccinated.
This is, e.g., described in the Methods section and in Tables 1+2 in the main article.
A1/
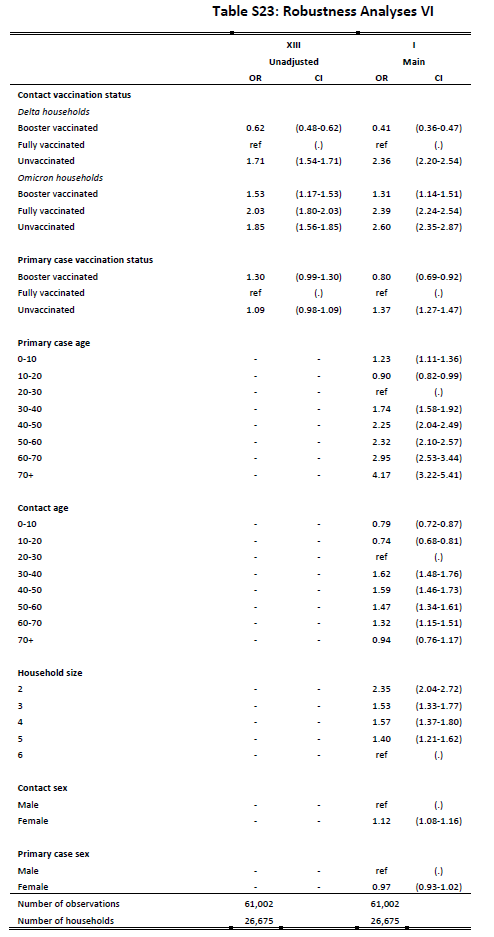
Appendix Table S23 (model I, Main) provides our main estimates (same as in Table 2+3).
Appendix Table S23 (model XIII) provides unadjusted estimates.
This shows that vaccination status is confounded with age, as expected.
A3/
Appendix Table S23 (model XIII) provides unadjusted estimates.
This shows that vaccination status is confounded with age, as expected.
A3/
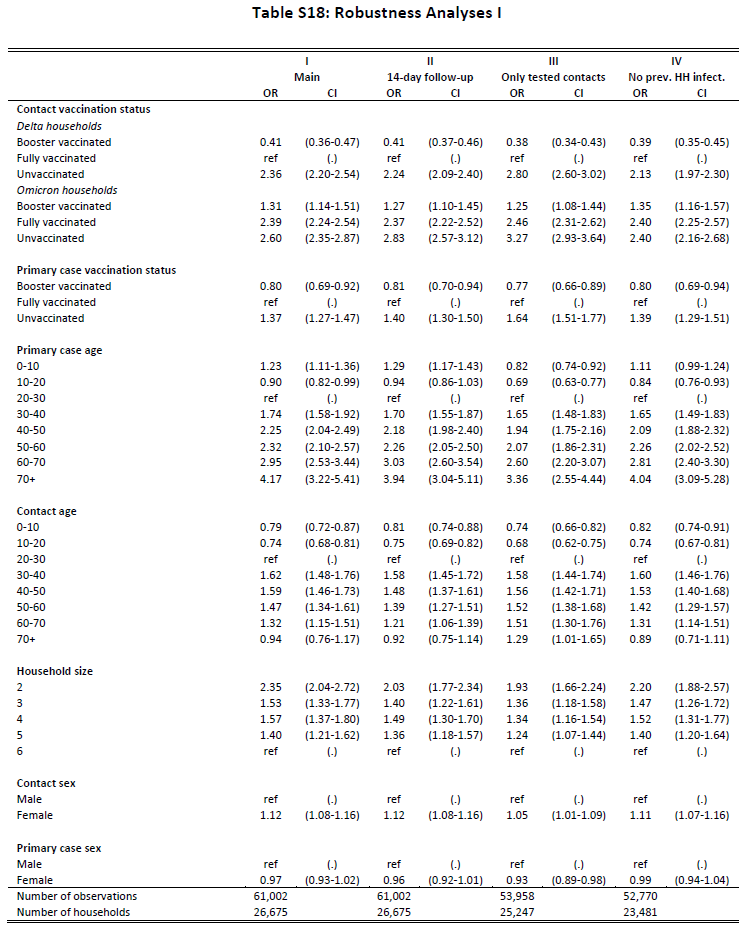
Appendix Table S18 (model IV) excludes all households with a previous infection.
Our estimates are robust to this restriction.
A4/
Our estimates are robust to this restriction.
A4/
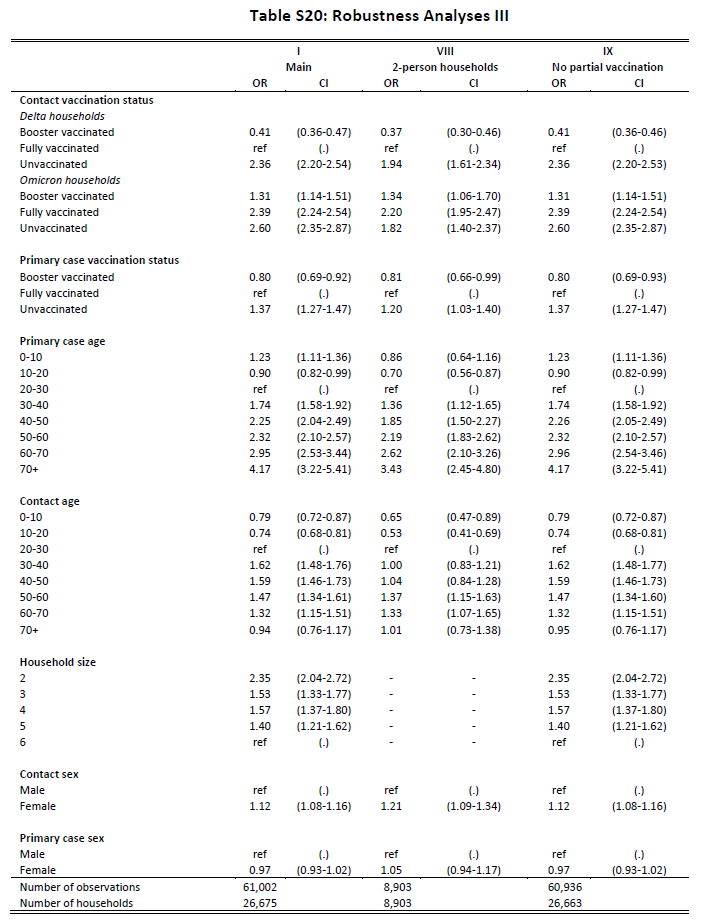
Appendix Table S20 (model IX) excludes all with partial vaccination.
Our estimates are robust to this restriction.
A5/
Our estimates are robust to this restriction.
A5/
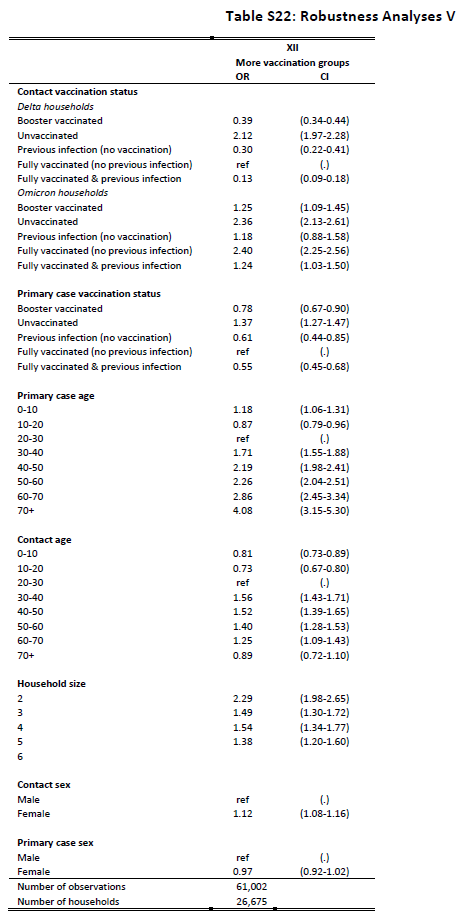
Appendix Table S22 (model XII) provides estimates with more vaccination groups, i.e., splitting previous infection from vaccination.
The estimates for these subgroups have less precision.
Our estimates are qualitatively similar with this specification.
A7/
The estimates for these subgroups have less precision.
Our estimates are qualitatively similar with this specification.
A7/
• • •
Missing some Tweet in this thread? You can try to
force a refresh