
1/11 A few years ago, I took care of two young women (some details changed) with similar scans… a brief thread about how MRI can shape a Ddx… but first a poll: Which lesions can restrict diffusion?
2/ Yes… all of these lesions can restrict diffusion. For more info on restricted diffusion see tweets 9-18 in this wonderful tweetorial from @teachplaygrub:
https://twitter.com/teachplaygrub/status/1541432382112145409?s=20&t=MHrVVyJilAaLVM9mqb3s5g
3/So some brief history about the 2 pts. First patient presented to another hospital months ago with R-sided hemiparesis and dysarthria. CSF showed elevated protein but no pleocytosis. Treated several times with steroids with transient improvement but has clinically progressed. 

4/Second patient developed L hemiparesis over two days. CSF showed neutrophilic pleocytosis with very high protein and normal glucose. Progessed to coma despite high dose steroids (and abx) 
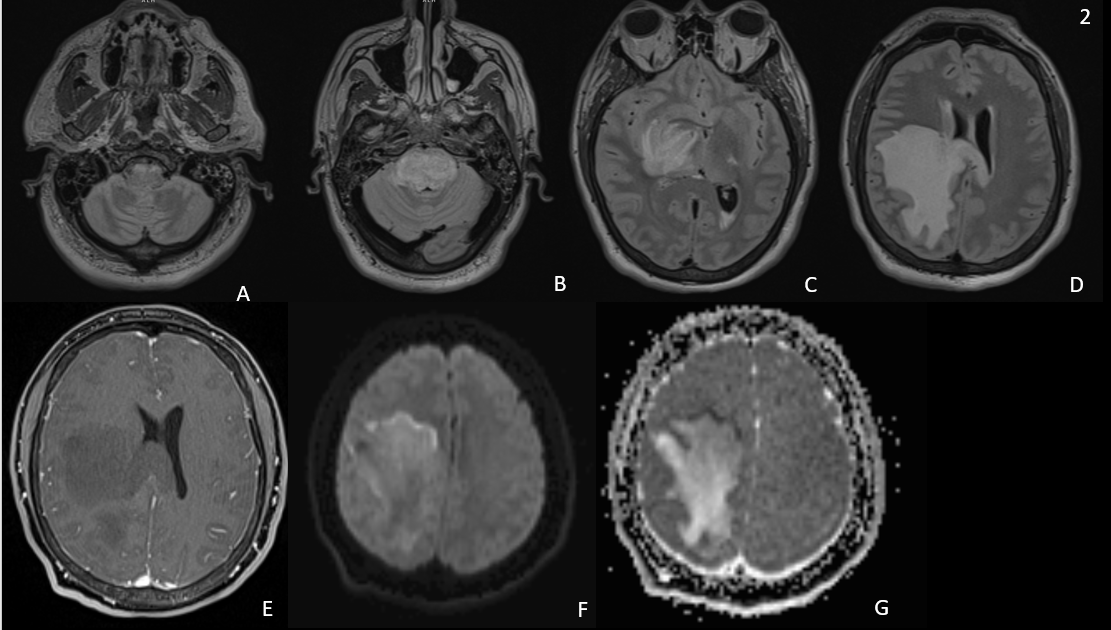
5/ MRIs at first glance very similar. Both with expansile T2 hyperintensity from medulla through basal ganglia. But pt 1’s lesion has gad enhancement (arrows) while pt’s 2 does not. 

6/Both have areas of restricted diffusion but with very different patterns. Pt 1’s lesion restricts diffusion in the center of the avidly enhancing basal ganglia portion of the lesion. Pt. 2’s restricts diffusion peripherally at the leading edge in the subcortical white matter. 



7/This is very helpful. Central restricted diffusion is more concerning for highly cellular tumors or abscess. Leading edge restricted diffusion is more concerning for demyelinating lesions (even without enhancement!). n.neurology.org/content/78/21/… 

8/Pt 2’s biopsy showed an extensive macrophage population with extensive myelin loss with many myelin fragments present within macrophages c/w inflammatory demyelinating lesions, in this case ADEM.
9/ Pt 1’s imaging which we noted could be c/w highly cellular tumor could represent GBM or Primary CNS Lymphoma (PCNSL). PCNSL is more often both supra- and infratentorial and more often had patchy or “stripy” appearance as we see in the cerebellum. rdcu.be/cWrAP 

10/Pt 1’s biopsy did indeed show Primary CNS Diffuse Large B-cell Lymphoma (DLBCL)
11/11 To summarize, central restricted diffusion in T2 hyperintense lesions more common in highly cellular tumors. Peripheral, or leading edge, restricted diffusion in a T2 hyperintense lesion more common in demyelinating disease. So look carefully!
#MedEd #neurology #neuroradiology #FOAMed #FOAMrad #neurotwitter @caseyalbin @EricLawson90 @MDNeurocritcare @mdneurorads @aszelikovich @AaronLBerkowitz @RiadRmdn @drdangayach @aartisarwal @DrGunjanParikh @AANmember @CPSolvers @DxRxEdu @MedTweetorials #Neurosurgery
@UMDNeurosurgery @a_charidimou @rkchoi @drltorres @ShadiYaghi2 @ContinuumAAN @JimmySuhMD @JimSiegler @sigman_md @MDNeurocritcare @Tracey1milligan @zach_london
• • •
Missing some Tweet in this thread? You can try to
force a refresh







