It's a PFO! A few words about this powerful echo window: The bicaval view 🧵 (1/8)
#POCUS #Medtwitter #echofirst #PCCMTwitter #ICUtwitter
#POCUS #Medtwitter #echofirst #PCCMTwitter #ICUtwitter
https://twitter.com/JonahRubinMD/status/1577058889454886912
This window is attainable only via a transESOPHAGEAL echo (TEE).
Point-of-care TEE is used widely in SICUs worldwide, and MICUs outside the US. You can expect to see them increasingly in US MICUs over the next decade. (2/8)
Point-of-care TEE is used widely in SICUs worldwide, and MICUs outside the US. You can expect to see them increasingly in US MICUs over the next decade. (2/8)
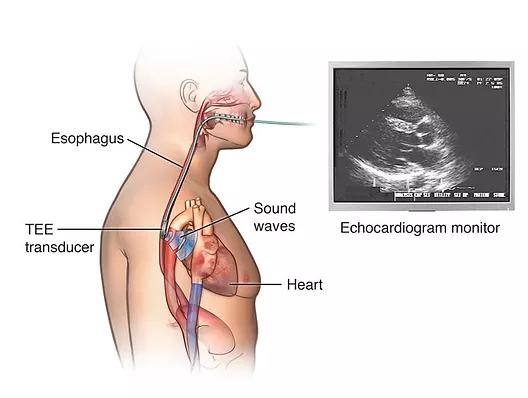
By viewing the heart via the esophagus, windows are often much crisper than when fighting with rib shadows, edematous lungs, and often bandages/wounds (esp. in surgical patients) on the chest. (3/8)
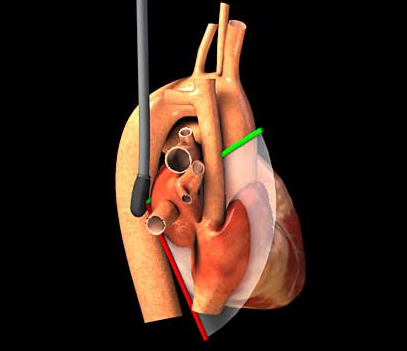
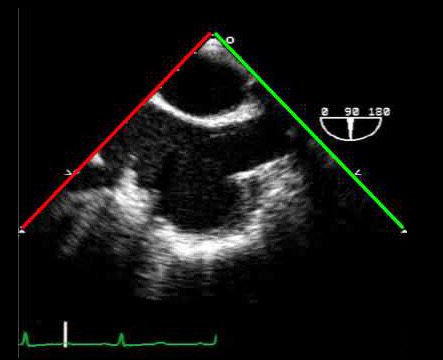
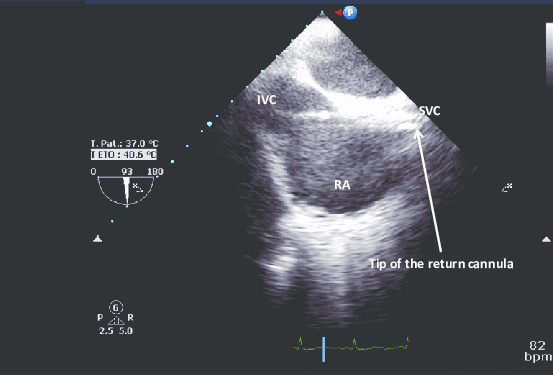
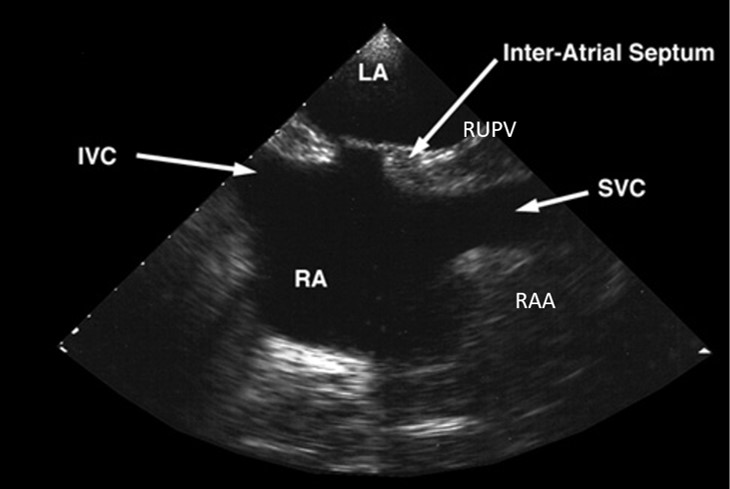
As its name suggests, the bicaval view allows you to see both vena cava - IVC and SVC - in one shot. It's obtained by placing the probe into the mid-esophagus, and rotating the omniplane angle to 90 degrees. Incredible simulator here: pie.med.utoronto.ca/tee/TEE_conten… (4/8) 


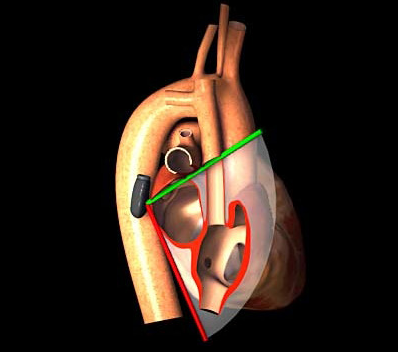
This view is extremely helpful when placing guidewires/catheters with little room for error - like ECMO cannulas. You can ensure the guidewire is venous, not going into the RV, and for dual lumen ECMO cannulas, confirm placement in both IVC and SVC. (5/8) 

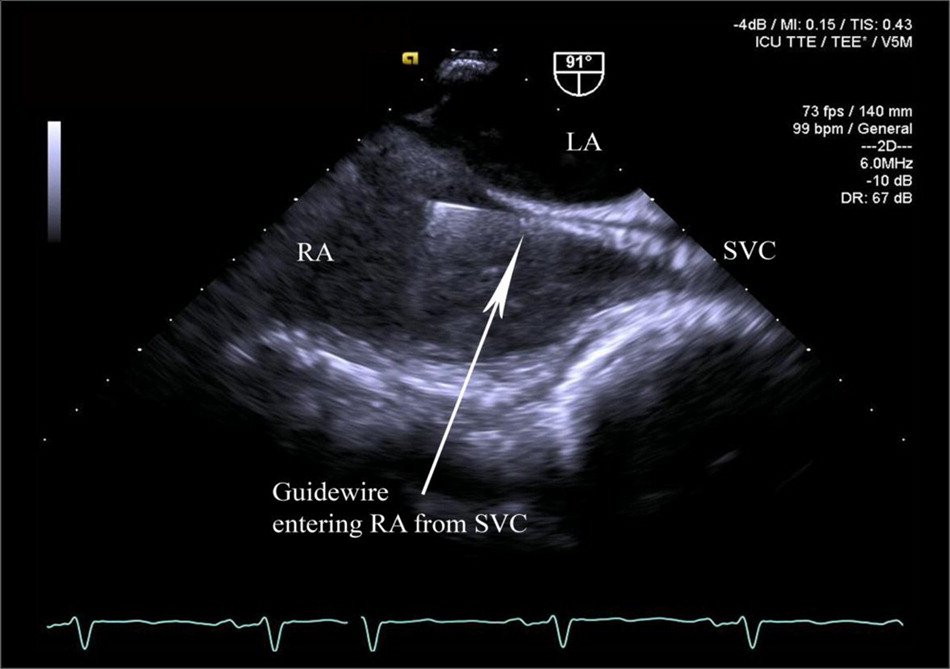
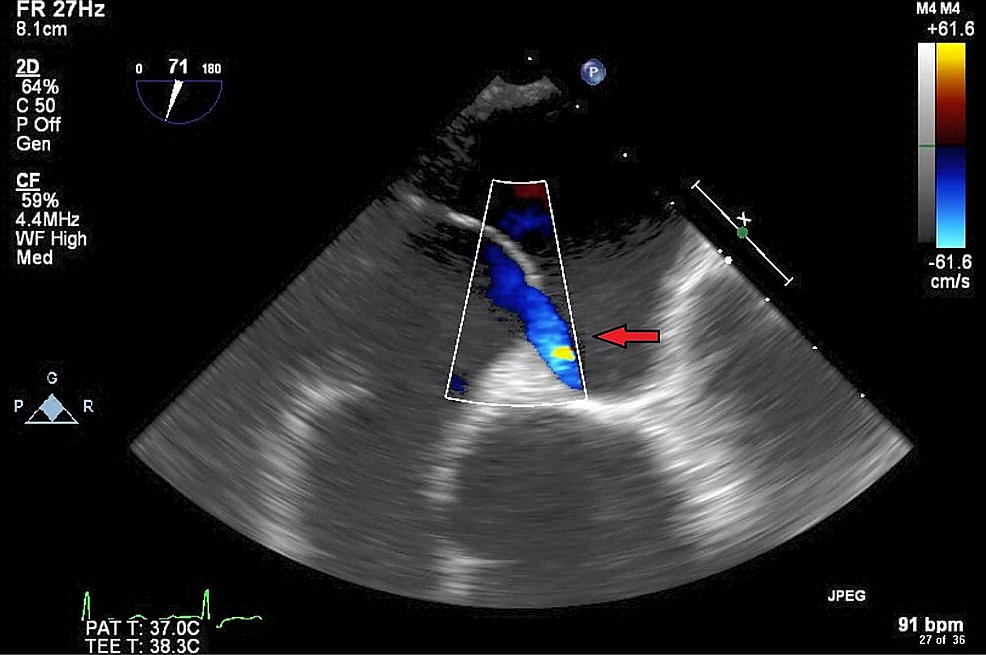
But it can also be seen as a bi*atrial* view because it allows you to see the RA and LA in one shot as well - including, of course, the interatrial septum. Note that the septum has two "beefy" ends, with a thin filament-appearing layer connecting them - the septum primum. (6/8) 
Normally, at birth, this adheres to the thicker septum secundum. Sometimes it doesn't truly seal, but the higher pressure of the LA (above the RA) keeps it flush against the septum secundum and closed. But when RA pressure rises above LA pressure, the flap can open ➡️PFO (7/8) 
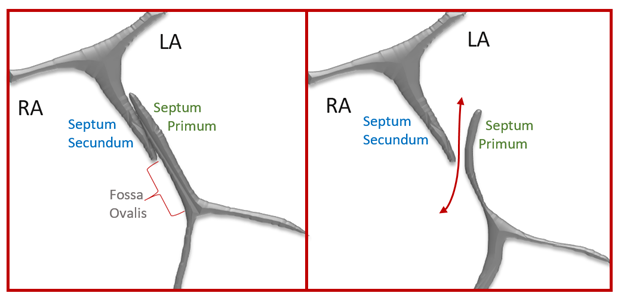
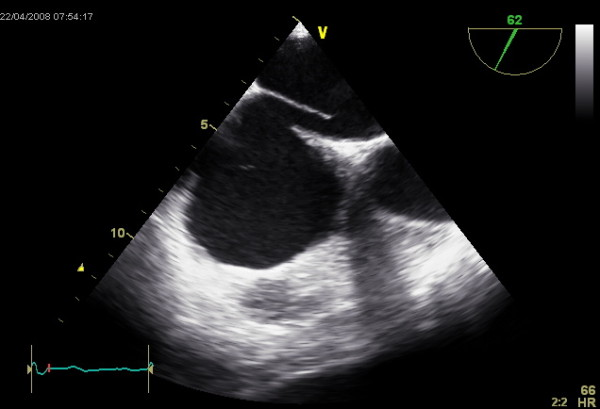
Note - this is not technically an ASD (atrial septal defect) - because the septa are all intact. In an ASD, part of the septum is missing or perforated. Note in this image, and our clip, the flow sneaks underneath the curtain, through the unsealed, patent, foramen ovale! (8/8) 

Thanks for reading! As always, thoughts, comments, rebuttals, and additional input always welcome!
• • •
Missing some Tweet in this thread? You can try to
force a refresh