
Jew.
CardioPulmonary Critical Care 🔥🫁🫀🔥 @harvardpulm @MGH_PCCM @MGHHeartHealth @MGHHCICU @HMSbioethics ecmo | echo | ethics | education | My tweets
How to get URL link on X (Twitter) App


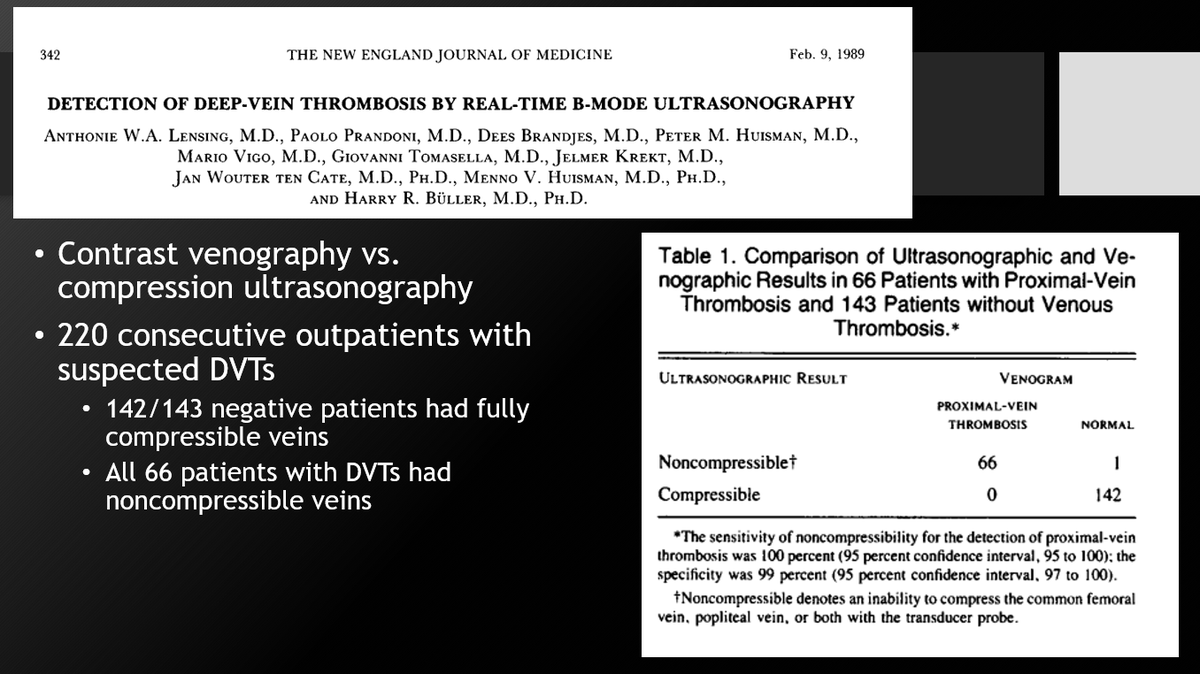
 Why do you care?
Why do you care? 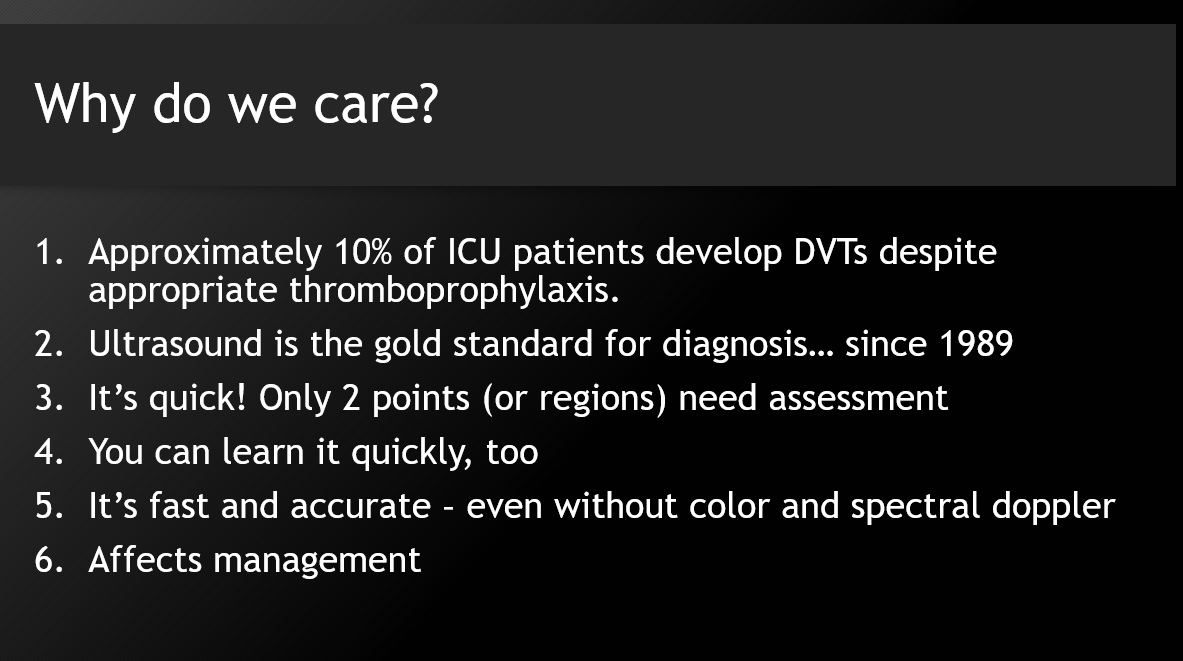

 1⃣ Be sure to optimize for the RV-focused view when making size assessments
1⃣ Be sure to optimize for the RV-focused view when making size assessments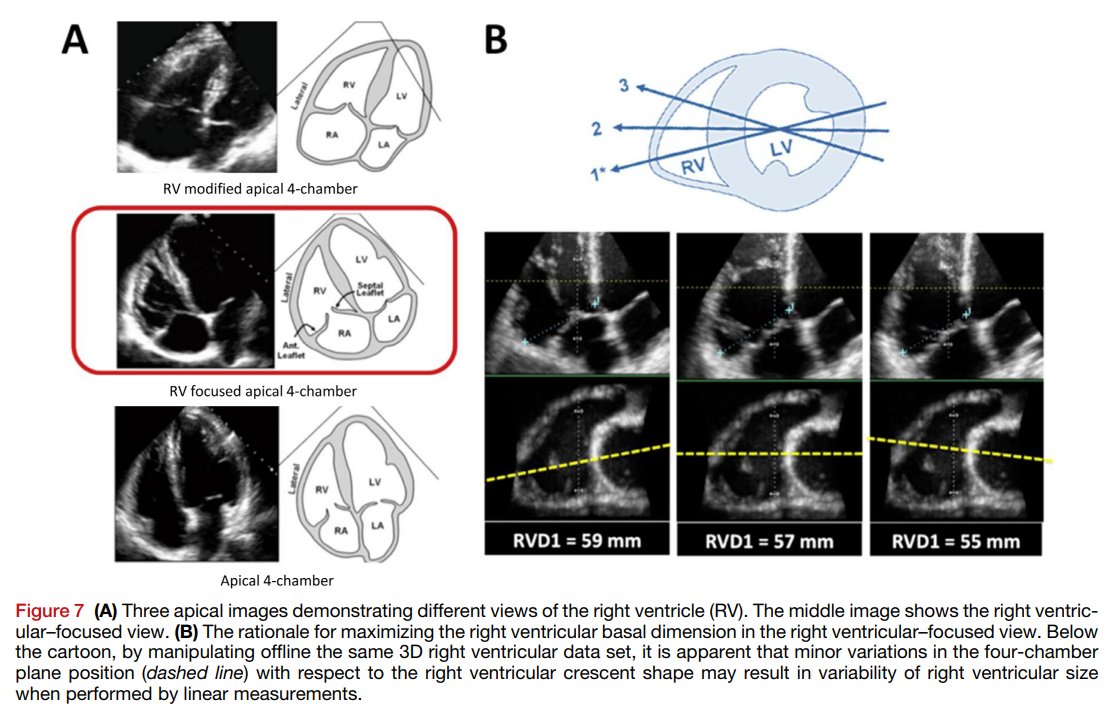
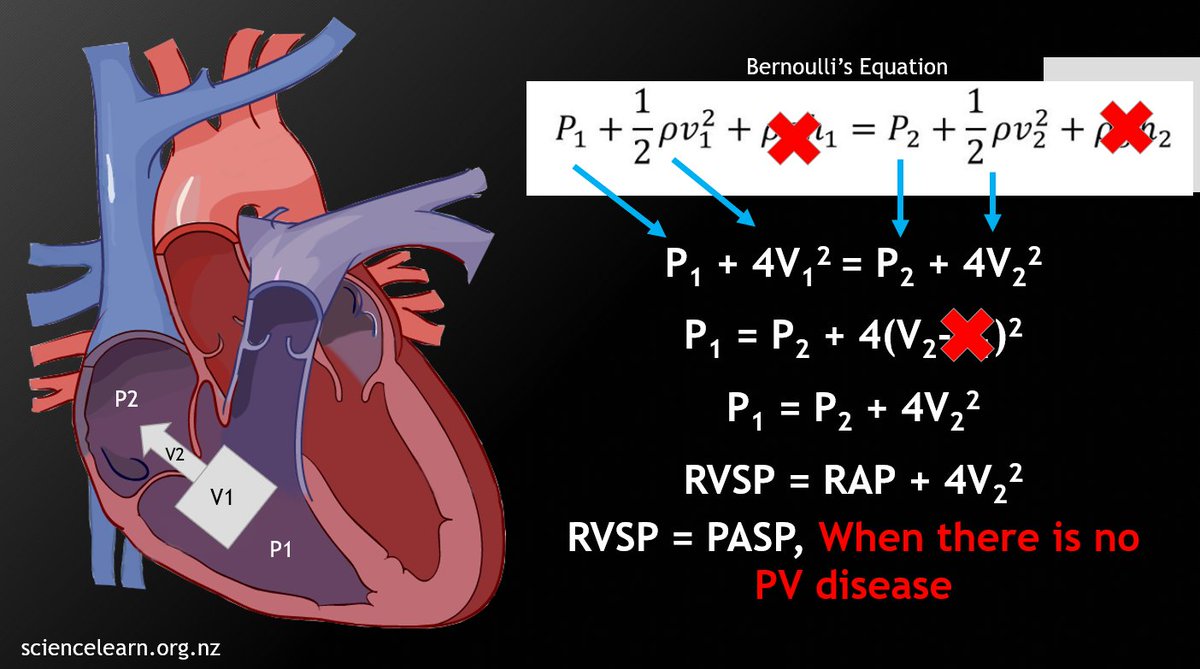
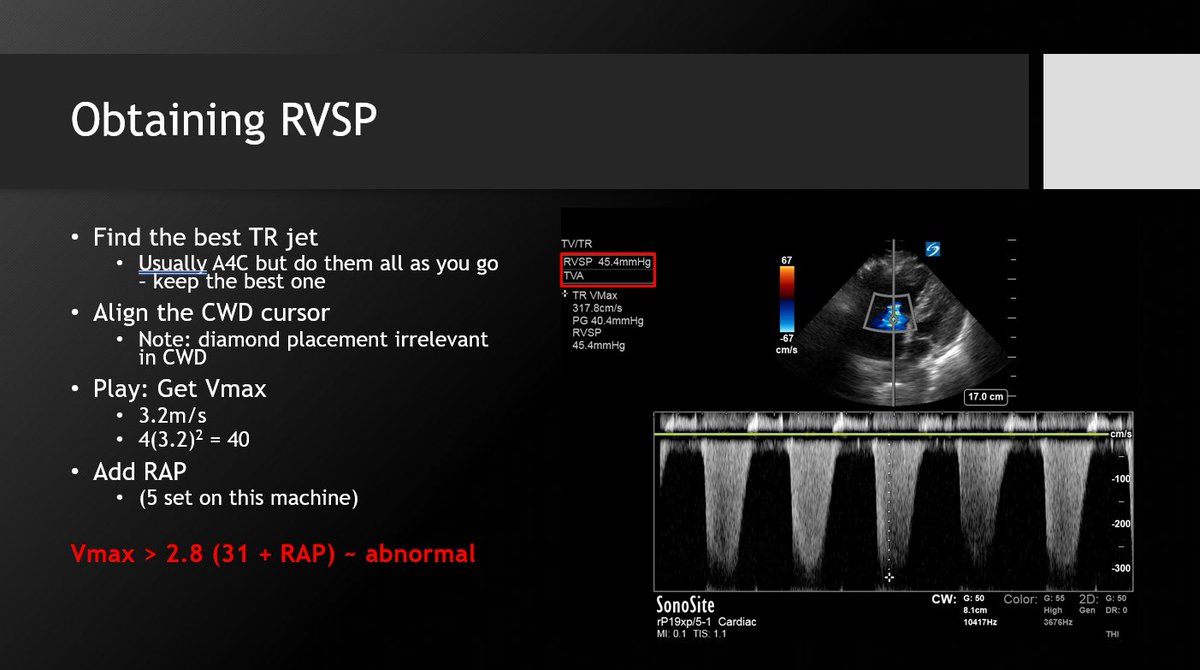
 1⃣ Speak to your PH specialists about RVSP role and utility in PH diagnosis and management. That is not its role for the intensivist.
1⃣ Speak to your PH specialists about RVSP role and utility in PH diagnosis and management. That is not its role for the intensivist.



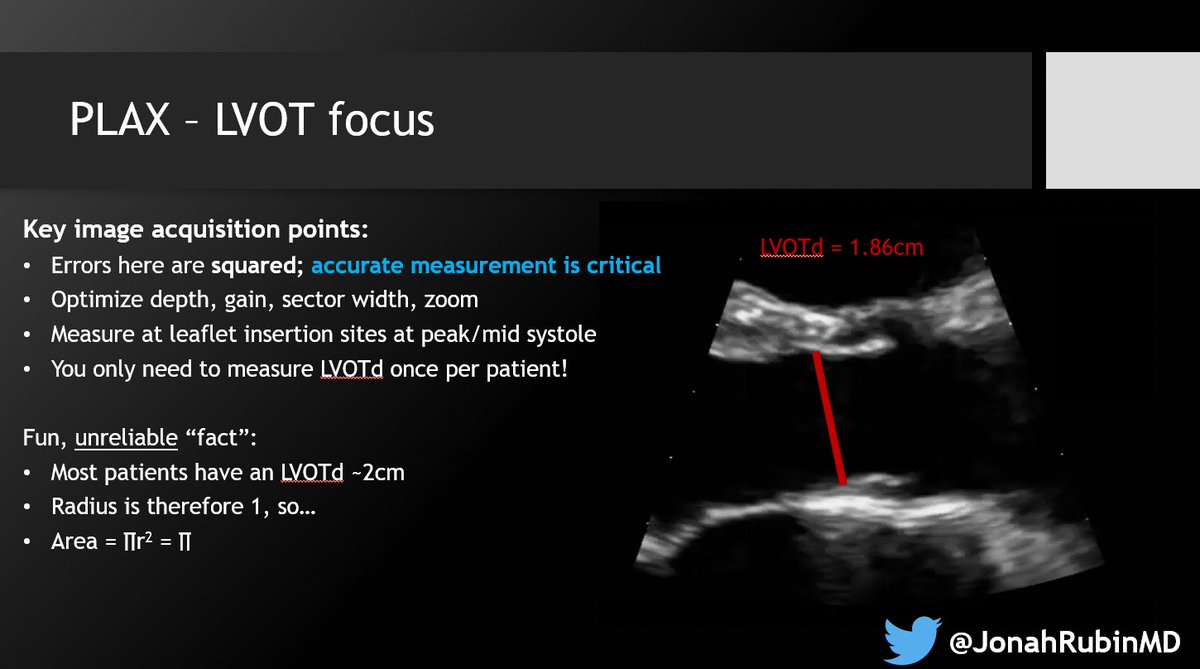
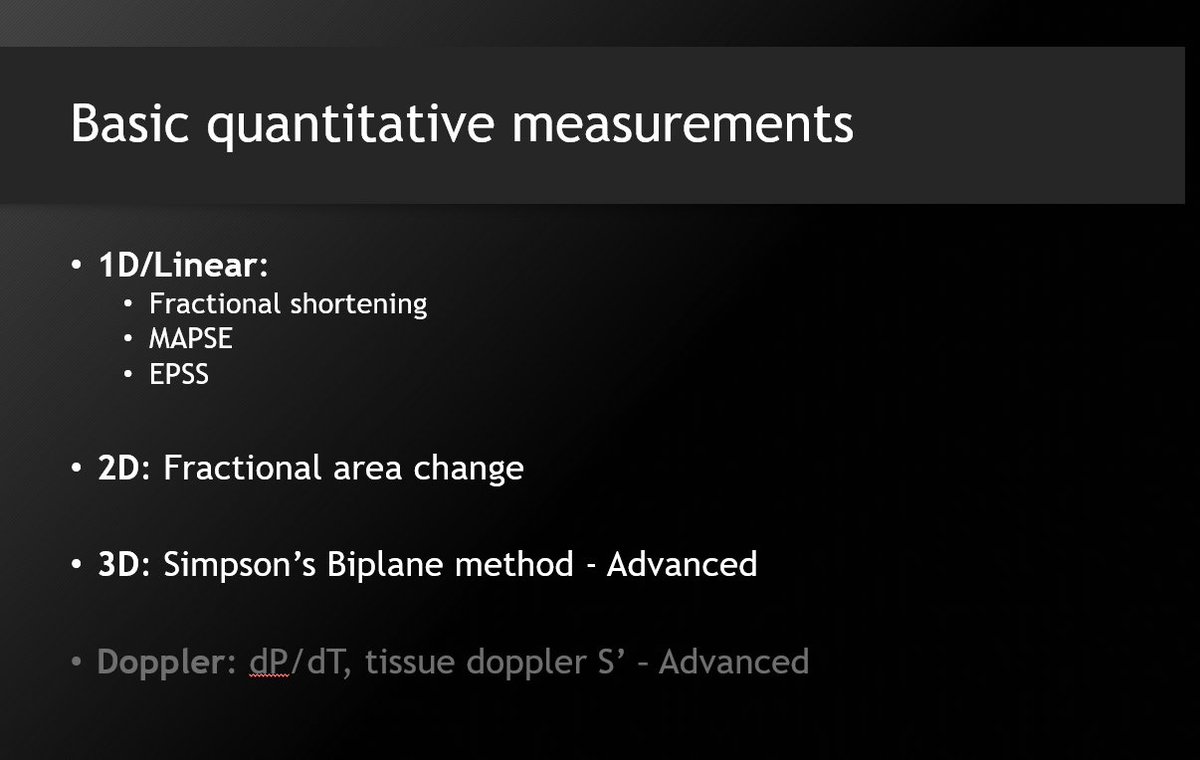
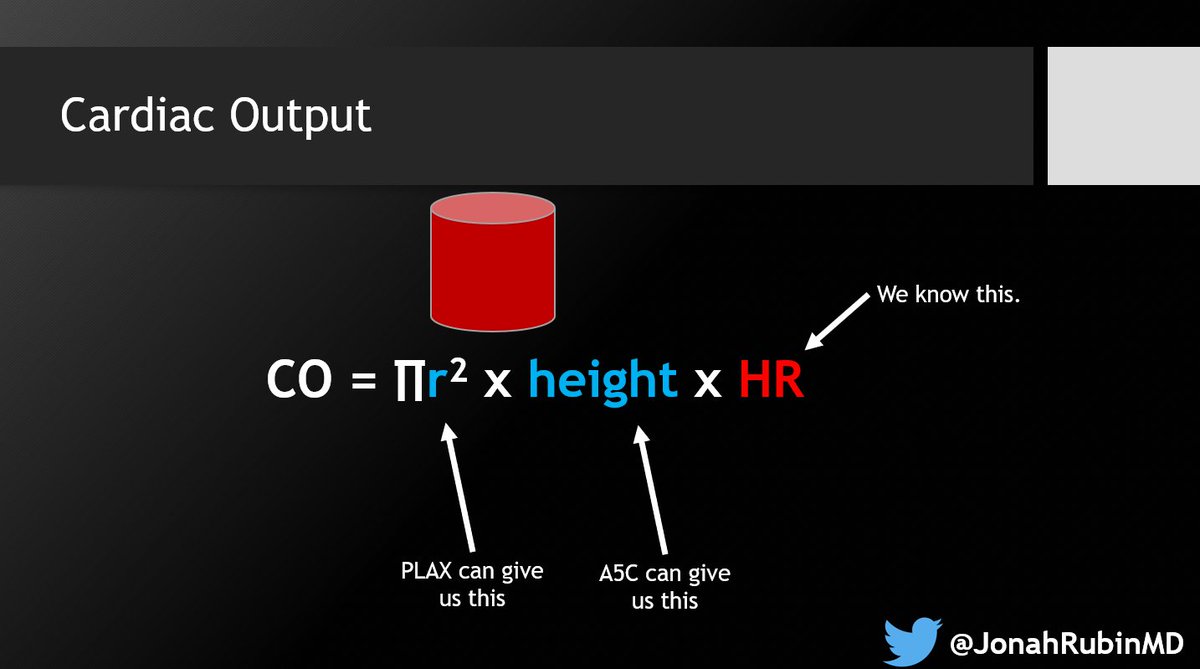 2⃣ Optimize the PLAX for the LVOTd. Sometimes I find that too much "optimization" actually makes it harder. Just know your options and do what works with your patient.
2⃣ Optimize the PLAX for the LVOTd. Sometimes I find that too much "optimization" actually makes it harder. Just know your options and do what works with your patient. 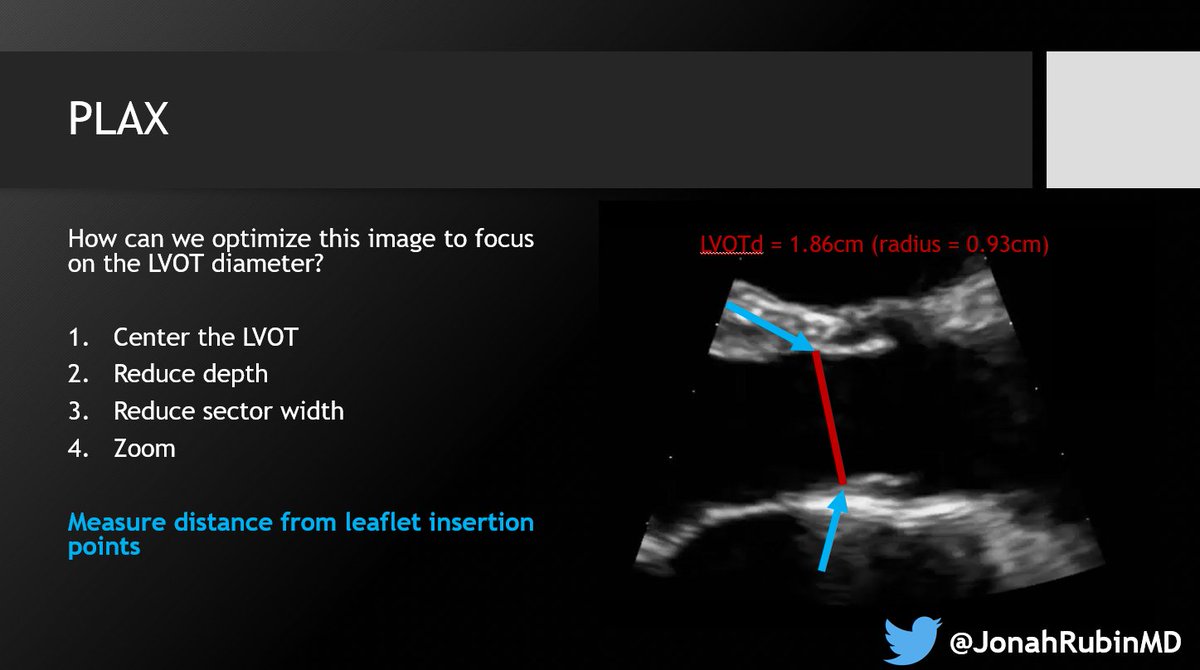
https://twitter.com/JonahRubinMD/status/1577058889454886912This window is attainable only via a transESOPHAGEAL echo (TEE).
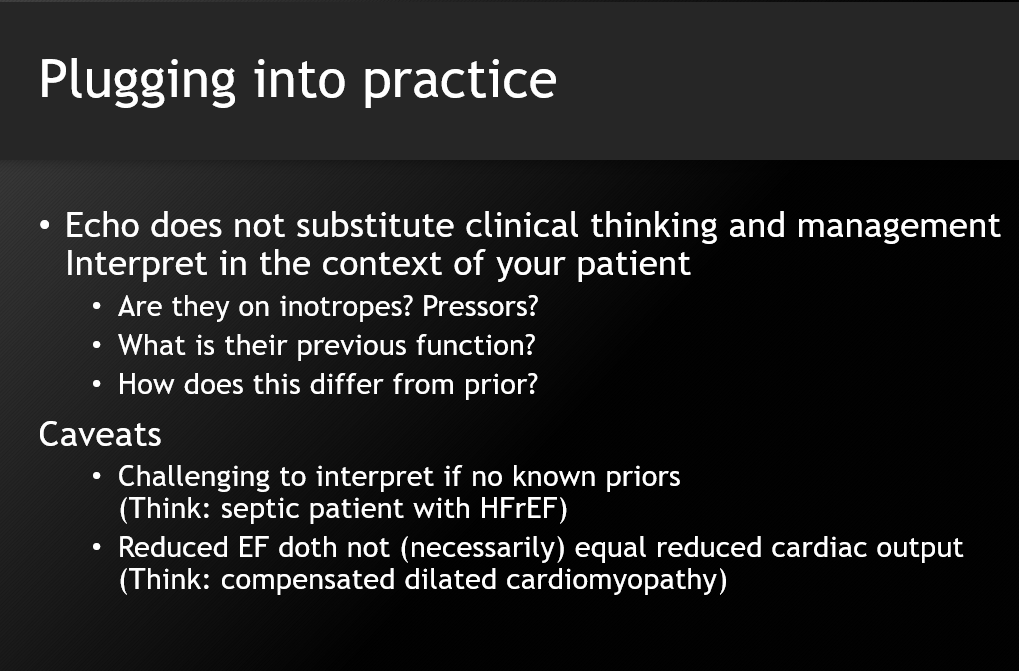 👀The oft-invoked 'eyeball' method is a deceptive oversimplification. You can't suddenly accurately assess LV function just because you're told to!
👀The oft-invoked 'eyeball' method is a deceptive oversimplification. You can't suddenly accurately assess LV function just because you're told to! 
https://twitter.com/JonahRubinMD/status/1490720088089104390It's a tale and disease perhaps ultimately worthy of discussion in the medical historical annals of @AvrahamCooperMD @tony_breu @AdamRodmanMD.
https://twitter.com/JeffreyGoldberg/status/1490376990054133770This piece reads as play-by-play a reenactment of the stories I learned about my grandparents and friend's families in the Holocaust. Acceptance of a progressively more racist and genocidal state. "It's not that bad", "it can't get worse", "our whole life is here".
 Session 1: Systematic Approach to Interpreting CT Chest led by Dr. Suhail Raoof!
Session 1: Systematic Approach to Interpreting CT Chest led by Dr. Suhail Raoof!
https://twitter.com/HarvardPulm/status/1369789019190665217
https://twitter.com/JonahRubinMD/status/1319307267389476865First, to address the elephant and 44% who correctly say this is generally impossible: Normally, you *cannot* increase O2 sats by adding Hg, bc sats refer to the saturation of Hg. Adding Hg doesn’t enable the lungs to saturate the new Hg any more than all the Hg it had before.