I am a cardiologist, and my work place is above the diaphragm?! Why should I care about the #liver and #NAFLD (non-alcoholic fatty liver disease)?
⚡️Our therapies in many cases reach well beyond the heart
⚡️In order to improve outcomes we have to tackle comorbidities
A🧵
⚡️Our therapies in many cases reach well beyond the heart
⚡️In order to improve outcomes we have to tackle comorbidities
A🧵

🟦NAFLD (prevalence 25%) isn't only a hepatic disease but also a systemic & CV disease w/o effective pharmacotherapy
🟦We discuss the promising role of SGLT2i in NAFLD, propose mechanisms, & suggest future directions.
sciencedirect.com/science/articl…
🟦We discuss the promising role of SGLT2i in NAFLD, propose mechanisms, & suggest future directions.
sciencedirect.com/science/articl…

The pathogenesis of NAFLD is multifactorial w/ parallel processes that involve insulin resistance, hepatic fat accumulation, increased lipotoxicity, mitochondrial dysfunction, oxidative stress, ER stress, abnormal autophagy, altered gut flora, & apoptosis. 

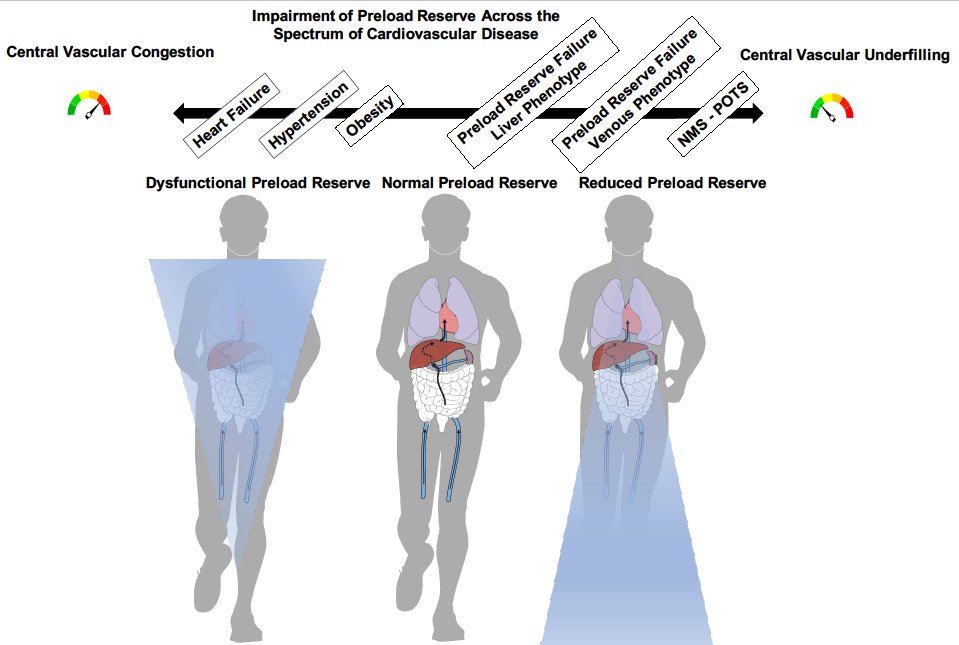
There's an association between NAFLD▶️atherosclerotic CVD + a newly recognized association between NAFLD and incident HF. NAFLD and HF (specifically HFpEF) share several pathophysiological mechanisms (inflammation, endothelial dysfunction, excess epicardial adipose tissue) 

Given robust evidence of CV benefits for SGLT2i in diseases that share similar pathophysiological mechanisms as NAFLD, a growing interest in investigating the role of SGLT2i in NAFLD has been undertaken w/ promising signals in (pre)clinical studies. sciencedirect.com/science/articl… 

How can SGLT2i potentially be beneficial in NAFLD? We discuss pathways by which SGLT2i can achieve the endpoints of increasing insulin sensitivity; decreasing fat accumulation in the liver, liptotixicty, oxidative stress, & ER stress; improving autophagy; & inhibiting apoptosis.
Dedicated large randomized clinical trails are needed to establish the efficacy of SGLT2i in patients w/ NAFLD
• • •
Missing some Tweet in this thread? You can try to
force a refresh