Duke Cardiology, 🇺🇦+🇩🇪+🇺🇸, #HeartFailure. Views expressed are my own and do not reflect the views or opinions of my employer.
How to get URL link on X (Twitter) App




 sciencedirect.com/science/articl…
sciencedirect.com/science/articl…







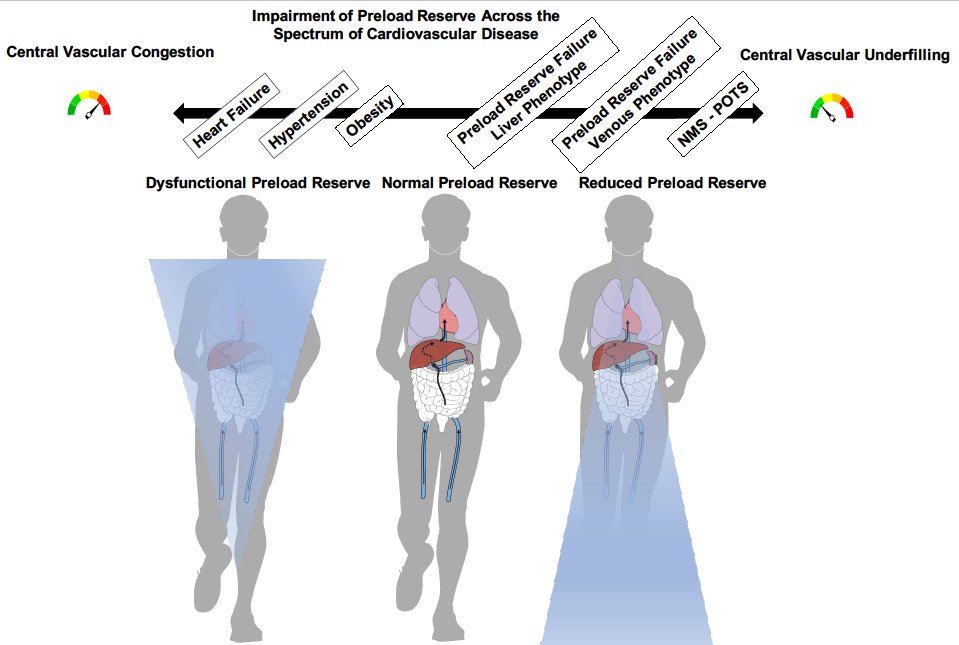
 🟦NAFLD (prevalence 25%) isn't only a hepatic disease but also a systemic & CV disease w/o effective pharmacotherapy
🟦NAFLD (prevalence 25%) isn't only a hepatic disease but also a systemic & CV disease w/o effective pharmacotherapy

https://twitter.com/AndrewCAhn2/status/1552715513859436544

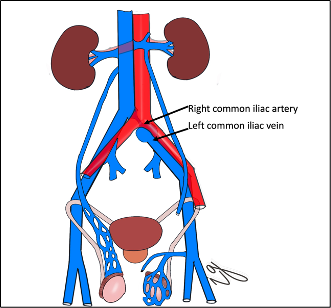 #2 The issue with venous distension in the abdomen and pelvis is that it creates venous pooling/obstruction to blood return. Its mostly in the abdomen and not legs!
#2 The issue with venous distension in the abdomen and pelvis is that it creates venous pooling/obstruction to blood return. Its mostly in the abdomen and not legs! 



 🚨As of July 4, 2022, there were about 529 million pts who recovered from COVID-19. The association between COVID-19 recovery and incident HF has not been studied in a large scale, nationally representative sample.
🚨As of July 4, 2022, there were about 529 million pts who recovered from COVID-19. The association between COVID-19 recovery and incident HF has not been studied in a large scale, nationally representative sample.

 #2
#2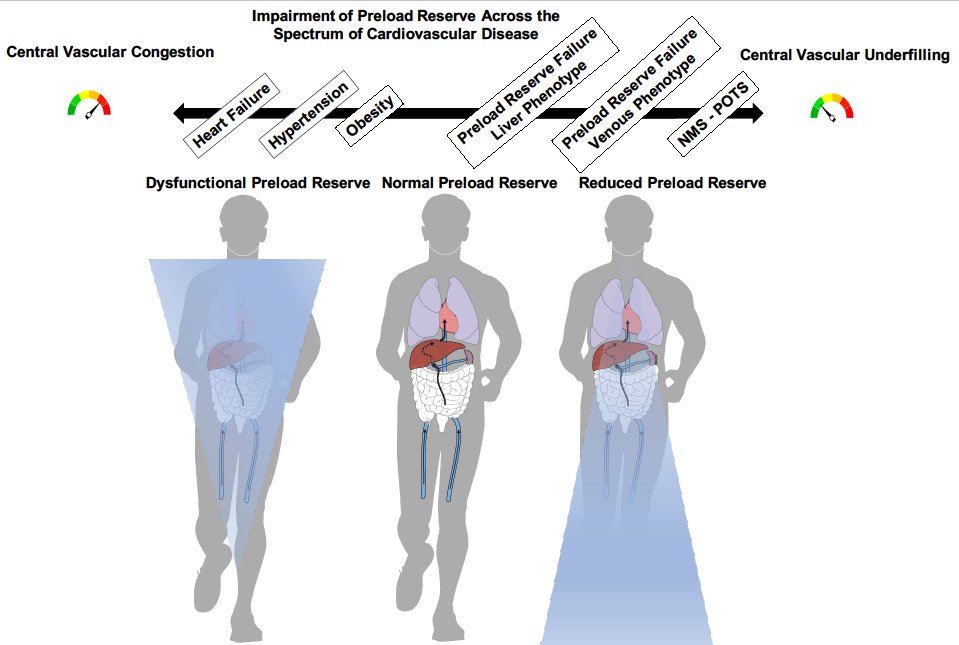
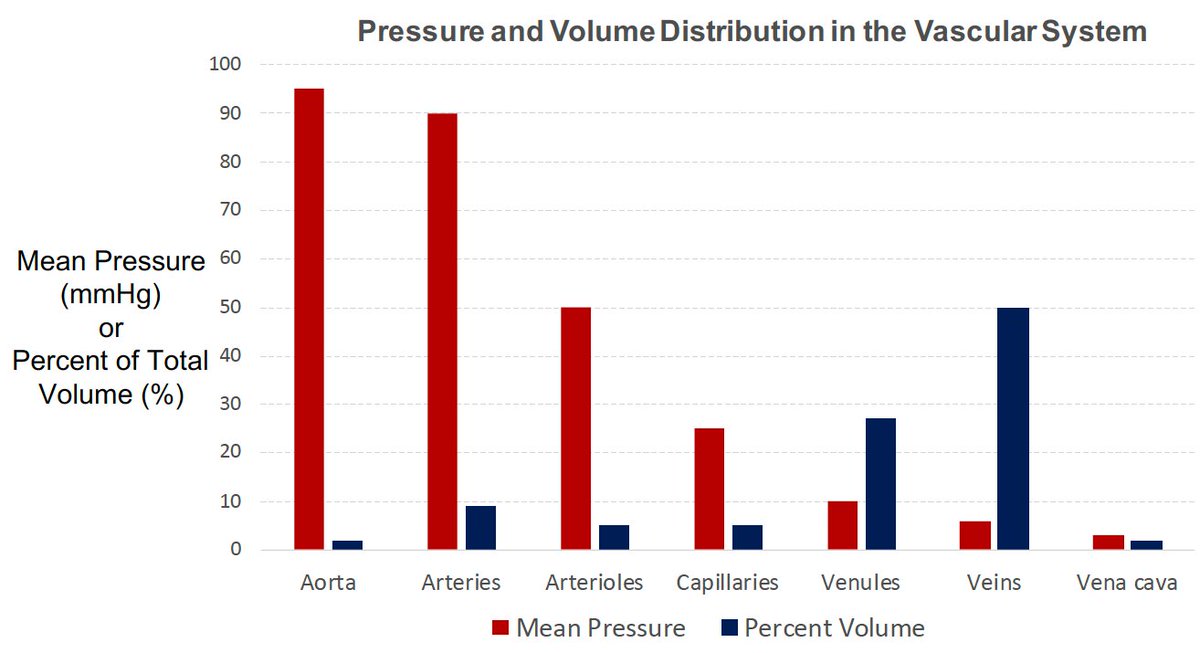
 2. Majority of intravascular blood volume is located in the venous system. Veins are highly innervated (in many instances more so than arteries). The abdomen pools the majority of the blood volume and blood can be recruited quickly in and out of the compartment.
2. Majority of intravascular blood volume is located in the venous system. Veins are highly innervated (in many instances more so than arteries). The abdomen pools the majority of the blood volume and blood can be recruited quickly in and out of the compartment.