NEXT session:: ARDS Ventilator Management. Domenico.
Case-based discussion. 29 F +++ BMI, PBW ~ 52kg. Dx :community acq pneumonia. pH 7.33, pO2 12 pCO2 3.8, Be - 8, on o2 reservoir mask. Legionella urinary Ag +. #LIVES2022
#ventilation #ARDS @ESICM What would you do next?
Case-based discussion. 29 F +++ BMI, PBW ~ 52kg. Dx :community acq pneumonia. pH 7.33, pO2 12 pCO2 3.8, Be - 8, on o2 reservoir mask. Legionella urinary Ag +. #LIVES2022
#ventilation #ARDS @ESICM What would you do next?
Choices : volume control with NMB , Pressure control with NMB, Assist mode ventilation, sport mode?
What was done :: cisatracurium, VC TV 280ml (5.3ml/kg), RR 36,PEEP 12, Fio2 0.8, Resp mechanics : Ppeak 39, Pplat 30, Delta P 18, Comp (RS) - 16ml/cmh20 with heated humidifier.
What is the problem with this Resp mechanics ?
What is the problem with this Resp mechanics ?
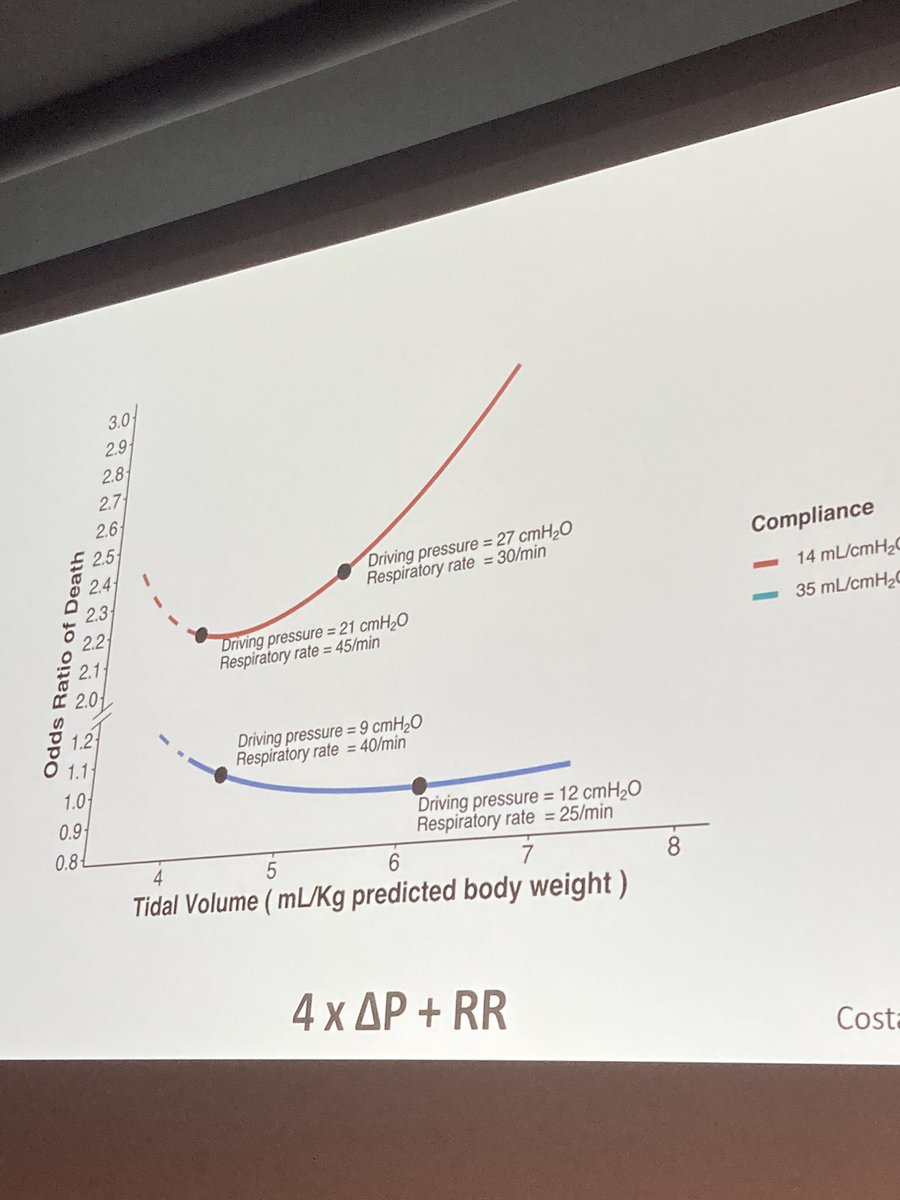
The driving pressure is too HIGH (again its not 14 is ok, 15 is not -- gradient is steeper after 15, generally lower the better). refresher : Driving Pressure as estimate of strain. pubmed.ncbi.nlm.nih.gov/25693014/
paper link for above : pubmed.ncbi.nlm.nih.gov/33784486/
Driving Pressure remains 18 despite optimisation. What would you do next? Options : A. ECMO B. Prone C. ECCO2R
Proning was done.
1. effects on oxygenation(Qs/Qt and Va/Q)
2. effects on mechanics
3. effects on VILI
4. effects on Haem-dynamics.
Proning was done.
1. effects on oxygenation(Qs/Qt and Va/Q)
2. effects on mechanics
3. effects on VILI
4. effects on Haem-dynamics.
Guerin paper : pubmed.ncbi.nlm.nih.gov/23688302/
After Proning, PEEP 10, delta P 20c,H20, VT 240ml Crs 12ml/cmh20, RR 36. (this is 6 hours after proning)
After Proning, PEEP 10, delta P 20c,H20, VT 240ml Crs 12ml/cmh20, RR 36. (this is 6 hours after proning)
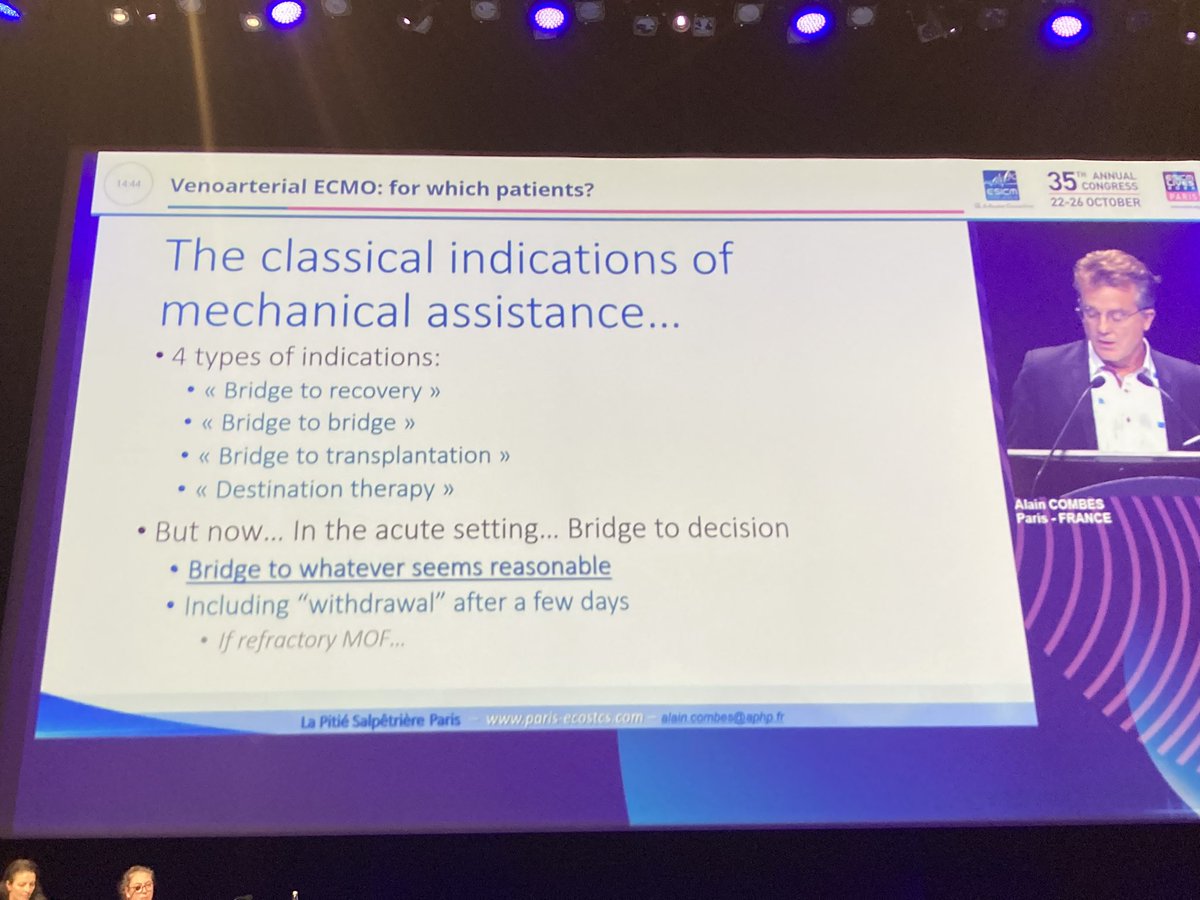
What would you do next? A. ECCO2R B. VV ECMO C. VA ECMO D. Oesophageal monitoring (I think we all know what the answer gonna be ;) )
Oesophageal monitoring. P oes-end-exp = 20cmH20, P ons end insp = 28, PEEP 20, delta P 20, Pplat 40, Delta P lung = 12. ratio of driving pressure of lung : driving pressure of respiratory system = 12/20 = 0.6.
The *TRUE* trans-pulmonary pressure. 0.6 * 40 = 24.
24 is acceptable.
The *TRUE* trans-pulmonary pressure. 0.6 * 40 = 24.
24 is acceptable.
Finally: patient weaned off 15 days after IMV.
Anecdotally, I feel like ECMO service in the UK becomes very robust post COVID, so sick ARDS patients end up in ECMO unit. What about sick ARDS patients who aren't eligible for ECMO -- how would local units manage?
Anecdotally, I feel like ECMO service in the UK becomes very robust post COVID, so sick ARDS patients end up in ECMO unit. What about sick ARDS patients who aren't eligible for ECMO -- how would local units manage?
AudienceQ : PEEP high potentially detrimental for RV function. it increases mechanically RV after load but it also recruits lung +++ & improve hyperaemia, the cumulative effect could be positive. Echo : key to assess the harmful effects @iceman_ex always Echo. :P
@iceman_ex This leads to discussion of Haem-dynamics of this patient case. Generally hypoxaemic pts are hypovolaemic - as too tired to drink & +++ ambient loss. Volume resuscitation key especially per-intubation. PPV unmasks the relative hypovolaemia. atsjournals.org/doi/10.1164/rc…
@iceman_ex which is why potentially propofol may be harmful sedative in an acute post inubation phase in this patient popn. sidetracking pubmed.ncbi.nlm.nih.gov/35536310/
• • •
Missing some Tweet in this thread? You can try to
force a refresh