1) I am so humbled that over 2K of you now follow me! 🥰. Still beaming from meeting so many peeps at #NCS2022. To celebrate, lets learn from another < than straightforward case #medtwitter #neurotwitter #neurorads #neurocritical
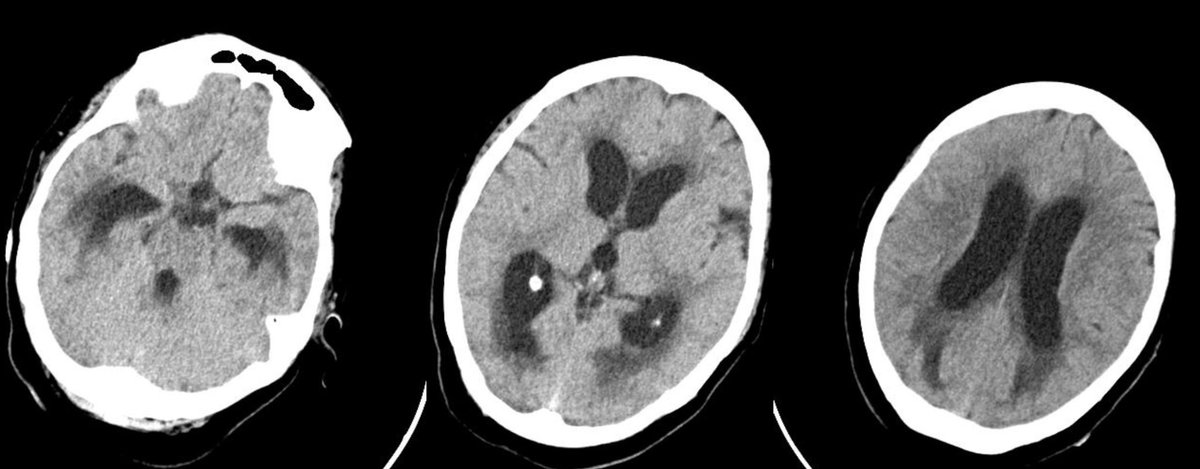
2) Middle aged person with HTN, 🚬 and THC daily use, presents w/ 3⃣days of severe HA described as “worst headache of life” ⛈️. We’ve been over this differential before but here it goes again 👇. They undergo CT head which demonstrates SAH and a right frontal IPH: 



3) They also undergo CTA which demonstrates a possible right MCA aneurysm (red arrow) as well as multiple areas of narrowing (blue arrows): 

4) What is your diagnosis
5) We'll get back to the diagnosis later. Which of the following features would place the patient at risk of developing RCVS?
6) If you picked C, 🥳🎉🍾! Marijuana is a known trigger for RCVS, but > on this later. Back to the patient. They are transferred with concern for aneurysmal rupture and undergo an angio where they are noted to have 3 🧠🎈: Right MCA, PCOM and ACA/pericallosal (red arrows): 



7) CT is as above. On exam, patient with severe headache but non focal. What are the Hunt/Hess and modified Fisher Scores?
8) Remember that Hunt and Hess is an older way of assessing mortality, and WFNS has < inter-rater variability and should be preferentially used for severity classification. Here is a breakdown of both scales: (from pbrainmd.wordpress.com/2015/03/24/hun…) 
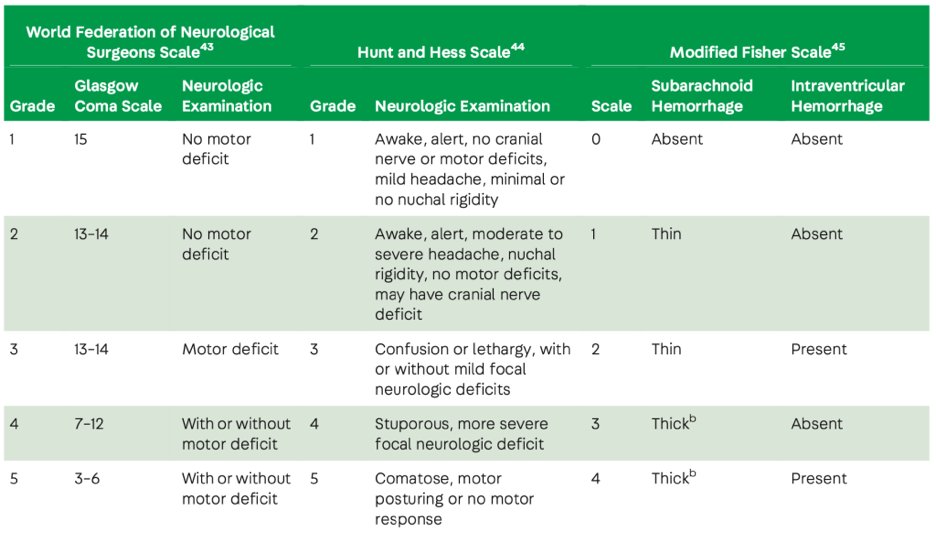
9) Fisher Score quantifies risk of vasospasm. Because the risk of vasospasm ⬇️ with increasing grade (3➡️4), the scale was revised and the modified Fisher is now more commonly used. Here is a breakdown of components: (from nursekey.com/subarachnoid-h…). This makes the pt a HH1mF3 

10) Based on SAH 🗺️, it is possible that right MCA or PCOM 🎈could have 🍾 and led to this pattern, & are treated: MCA is coiled, right PCOM is managed with a flow-diverting stent. Final run still w/ right PCOM anr filling. 

11) The patient is monitored closely over the next several days for any signs of vasospasm. Which of the following is NOT a way of monitoring for vasospasm development?
12) While all can be used to monitor for spasm, A, B and C can be used on a daily and ongoing basis, whereas D is reserved for when we need to confirm vasospasm. See more on vasospasm at:
https://twitter.com/rkchoi/status/1574117263313195011?s=46&t=X4P8MrmK8FV6k8FZfN--ow
13) The patient fortunately never develops any indication that there is vasospasm and did great. However, the question at the time of discharge is whether she had RCVS or aneurysmal SAH. What do you think?
14) The Dx = 🤷. Based on the pattern of SAH, the presence of small areas of spasm that resolved by the time they had an angio, and the 🏥 course (never had any spasm, hyponatremia & HA resolved), we felt the > likely diagnosis was RCVS. Discharge on nimodipine?
15) Because we could not rule out an aneurysmal process, we did discharge her on nimodipine. Remember nimodipine does not help with spasm but does improve outcomes: nejm.org/doi/full/10.10…
16) Let’s spend a moment talking about RCVS, which is Reversible Cerebrovascular Vasoconstriction Syndrome, aka Call-Fleming syndrome, aka Drug induced cerebral arteritis aka benign angiopathy of the CNS
17) Pathophys is incompletely understood. P/w ⛈️👏headache, CT can show strokes, ICH and/or SAH and vascular imaging will show the multifocal segmental vasoconstriction.
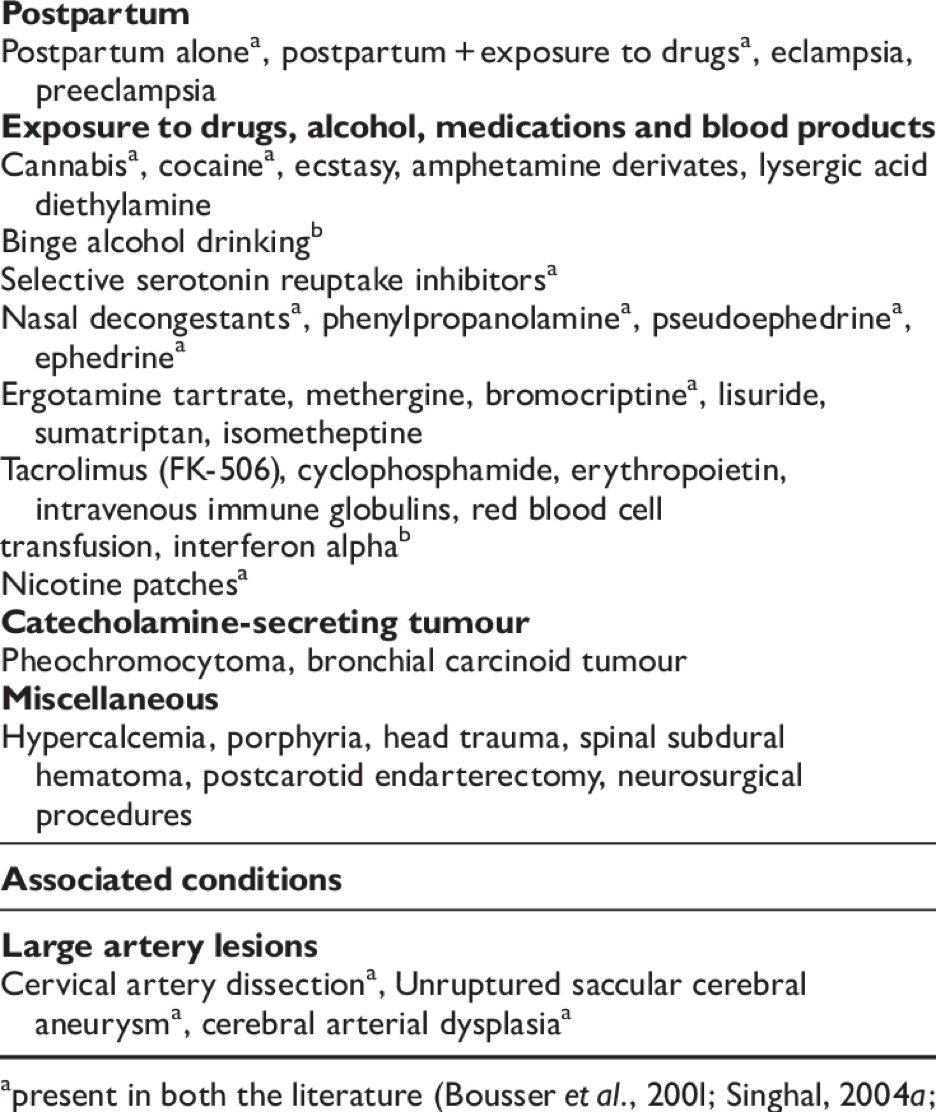
18) Common triggers = post partum, post coital, and frequently drug induced (cocaine, THC, SSRI, nasal decongestants, tacrolimus most common) (from researchgate.net/figure/Precipi…) 
19) Sometimes, meditation can also cause this…
https://twitter.com/rkchoi/status/1554246705750712320?s=46&t=X4P8MrmK8FV6k8FZfN--ow
20) Management typically involves treating the spasm with a CCB such as Verapamil, treat symptoms, BP control and sz 💊 as needed. We monitor vasospasm as if the patient had SAH. If the vasoconstriction is severe enough, it may warrant intervention via angio, but this is rare.
21) Patients with RCVS typically do well and recurrence is uncommon. However, some patients can develop massive strokes, edema and death.
End) Take 🏡 points:
✅RCVS can cause thunderclap headache and present with SAH
✅In a pt with RCVS who has aneurysms, treat the deadlier one first
✅RCVS has a fairly good prognosis
✅Monitor for spasm in both
✅Treat with CCB in both
✅RCVS can cause thunderclap headache and present with SAH
✅In a pt with RCVS who has aneurysms, treat the deadlier one first
✅RCVS has a fairly good prognosis
✅Monitor for spasm in both
✅Treat with CCB in both
Other comments, ideas, questions, approaches? @CaseyMayPharmD @caseyalbin @PulmCrit @drdangayach @RamaniBalu1 @EricLawson90 @JimmySuhMD @JayKinariwala @a_charidimou @ShadiYaghi2 @namorrismd @aartisarwal @SMuehlschMD
Correction, severe headache makes the pt HH2 not 1 👆
• • •
Missing some Tweet in this thread? You can try to
force a refresh