Great article on neurocritical care of the pregnant patient by Dr. Malaiyandi: ncbi.nlm.nih.gov/pmc/articles/P…
Some pearls:
👉 🔑 tenet is prioritize outcome of mother while minimizing harm to fetus #reproductiverightsarehumanrights
👉PA<AP radiation
👉Use preservative free heparin
Some pearls:
👉 🔑 tenet is prioritize outcome of mother while minimizing harm to fetus #reproductiverightsarehumanrights
👉PA<AP radiation
👉Use preservative free heparin
👉 NCCT head <0.001mGy exposure👉 Avoid use of lead over abdomen for CT - may actually increase radiation exposure
👉POCUS can raise temp from absorption of sound waves. B-mode best, Doppler worst. Minimize time
👉CT contrast = cat B, use when urgently needed vs MRA when not
👉POCUS can raise temp from absorption of sound waves. B-mode best, Doppler worst. Minimize time
👉CT contrast = cat B, use when urgently needed vs MRA when not
👉avoid Gadolinium, however, but ok to breastfeed post
👉tPA/tNK do not cross placenta, but ⬆️ risk uterine bleeding - per @StrokeAHA_ASA give when benefit>risk
👉Lovenox best for AC. DOACs ⬆️ risk of miscarriage
👉#PCC/FFP/protamine cat. C. #andexanet = cat. N
👉tPA/tNK do not cross placenta, but ⬆️ risk uterine bleeding - per @StrokeAHA_ASA give when benefit>risk
👉Lovenox best for AC. DOACs ⬆️ risk of miscarriage
👉#PCC/FFP/protamine cat. C. #andexanet = cat. N
BP wise:
👉1st line=labetalol, nifedipine. Can use labetalol💧
👉2nd line=hydralazine, clonidine, thiazide. Can use nicardipine or esmolol 💧
👉AVOID ACEI/ARBs
👉1st line=labetalol, nifedipine. Can use labetalol💧
👉2nd line=hydralazine, clonidine, thiazide. Can use nicardipine or esmolol 💧
👉AVOID ACEI/ARBs
Antiseizure 💊:
👉LEV and LTG (low dose) likely best
👉PHB, VPA, PHT worst
MG
👉#IVIG/#PLEX ok
👉oral pyridostig ok, but 🚫 IV
👉LEV and LTG (low dose) likely best
👉PHB, VPA, PHT worst
MG
👉#IVIG/#PLEX ok
👉oral pyridostig ok, but 🚫 IV
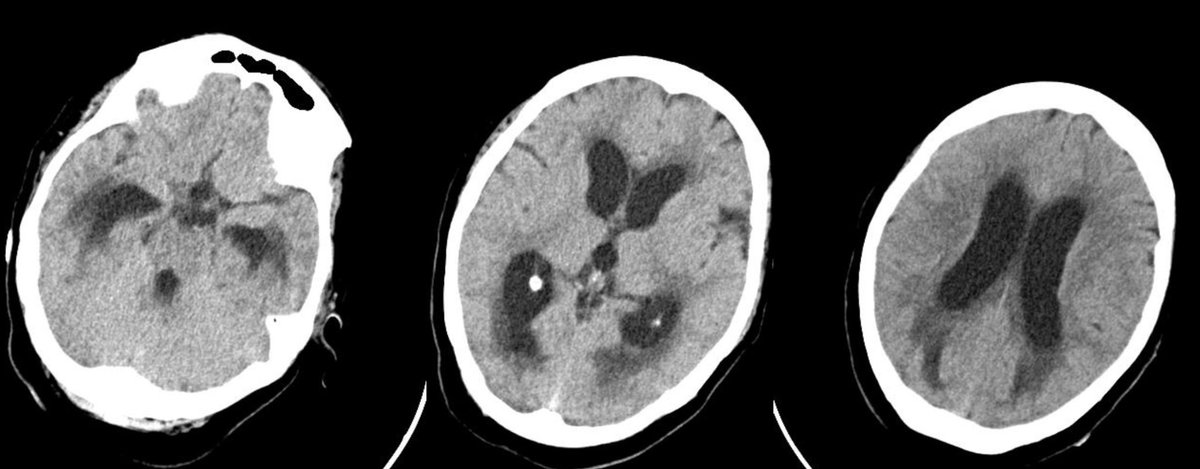
ICP crisis:
👉avoid hypertonic🧂 or mannitol 🍬 as able
👉decompressive hemicrani sooner than you otherwise would
👆and more from the paper! 🙏 Dr. Malaiyandi et al!
👉avoid hypertonic🧂 or mannitol 🍬 as able
👉decompressive hemicrani sooner than you otherwise would
👆and more from the paper! 🙏 Dr. Malaiyandi et al!
Other pearls? @caseyalbin @EricLawson90 @a_charidimou @Capt_Ammonia @CajalButterfly @oneDRwoman1 @DSandsmarkMDPhD @RamaniBalu1 @DrAtulRamesh1 @TJUHNeuroCrit
• • •
Missing some Tweet in this thread? You can try to
force a refresh