
#ContinuumCase!
A 71 year old has had 18 months of frequent falls
While eating, he leaves food on the closest part of the plate
His exam shows slow saccades, limb dyspraxia, and axial rigidity
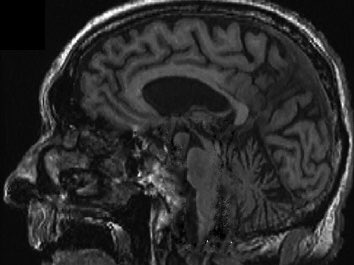
Sagittal T1 MR below. What’s going on here, #neurotwitter? 🧵
A 71 year old has had 18 months of frequent falls
While eating, he leaves food on the closest part of the plate
His exam shows slow saccades, limb dyspraxia, and axial rigidity
Sagittal T1 MR below. What’s going on here, #neurotwitter? 🧵
What’s the most likely diagnosis in this patient?
The combination of
➡️ Falls
➡️ Slowed saccades (especially vertical)
➡️ Axial rigidity
➡️ Midbrain atrophy
All suggest the diagnosis of progressive supranuclear palsy (PSP)
➡️ Falls
➡️ Slowed saccades (especially vertical)
➡️ Axial rigidity
➡️ Midbrain atrophy
All suggest the diagnosis of progressive supranuclear palsy (PSP)
PSP is a rare 4-repeat tauopathy with an increasingly diverse array of phenotypes:
➡️ Parkinsonism
➡️ Vertical gaze paresis
➡️ Gait freezing (⬆️⬆️ falls!)
➡️ Cognitive impairment
➡️ Corticobasal syndrome
➡️ Parkinsonism
➡️ Vertical gaze paresis
➡️ Gait freezing (⬆️⬆️ falls!)
➡️ Cognitive impairment
➡️ Corticobasal syndrome
Imaging of patients with PSP may demonstrate midbrain atrophy, including:
➡️ In sagittal plane, the “hummingbird” sign
➡️ In axial plane, the “Mickey Mouse” or “morning glory” sign
➡️ In sagittal plane, the “hummingbird” sign
➡️ In axial plane, the “Mickey Mouse” or “morning glory” sign

Thanks to Dr. Alex Pantelyat @HopkinsMedNews for the case and an excellent discussion of PSP and CBS, all in the latest issue of @ContinuumAAN, guest edited by Dr. Kathleen Poston @pddoc!
journals.lww.com/continuum/Full…
journals.lww.com/continuum/Full…
• • •
Missing some Tweet in this thread? You can try to
force a refresh







