Critical care echo lecture #4 @HarvardPulm @MGH_PCCM @PCCSM_BIDMC:
JUST THE RIGHT PRESSURE (i.e. assessing RVSP😀).
Key slides ⤵️ and brief pearls/takeaways 🧵... (1/8)
#Medtwitter #echofirst #PCCMTwitter



JUST THE RIGHT PRESSURE (i.e. assessing RVSP😀).
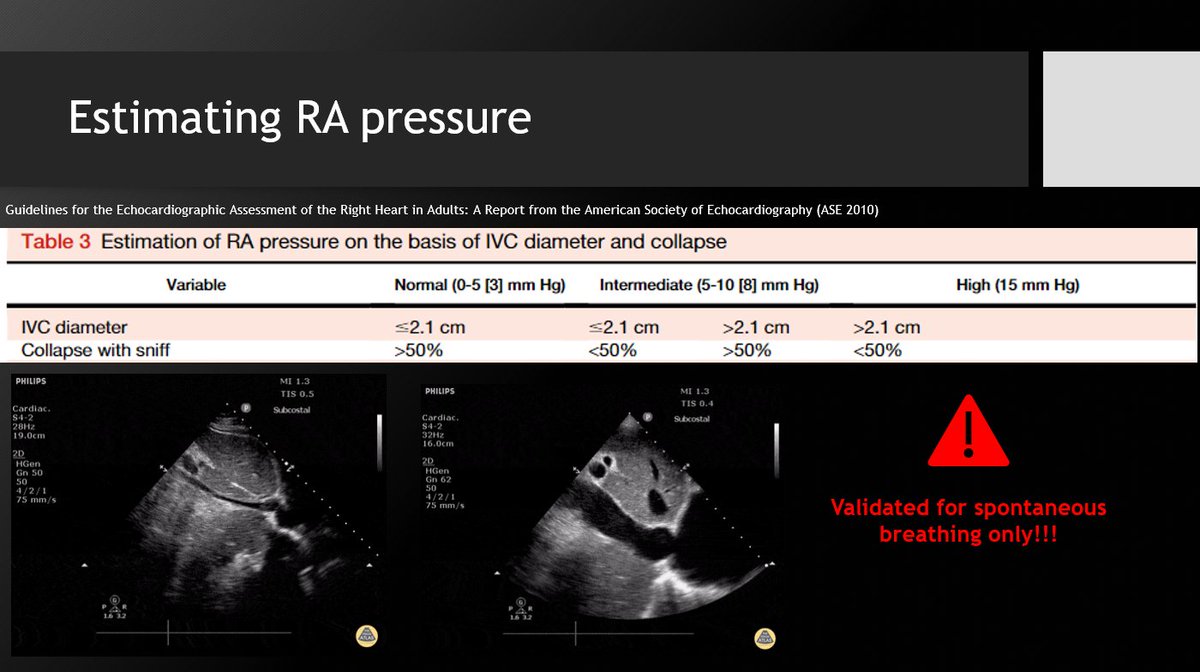
Key slides ⤵️ and brief pearls/takeaways 🧵... (1/8)
#Medtwitter #echofirst #PCCMTwitter
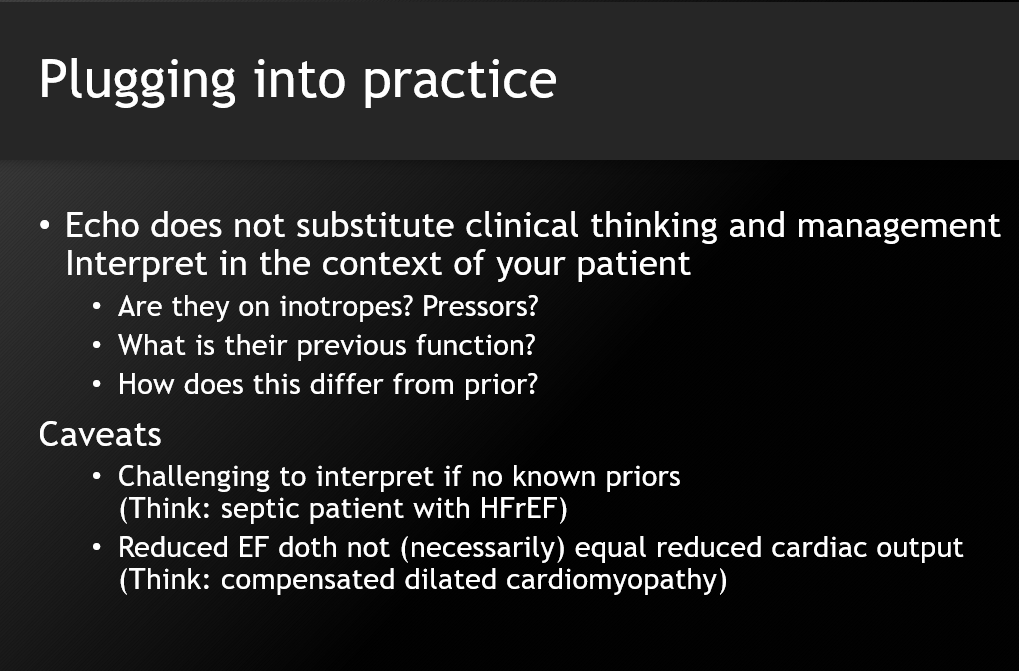
1⃣ Speak to your PH specialists about RVSP role and utility in PH diagnosis and management. That is not its role for the intensivist.
2⃣ Acutely, RVSP can help determine if there is a chronic component to elevated PA pressures (>60 usually not acute!), but does not rule out acute on chronic, nor pseudonormalization in severe RV failure
3⃣ More importantly: in the ICU, when without a Swann-Ganz catheter, RVSP can *help* (like all ICU data, not unilaterally) guide decisions about hemodynamic management such as inotrope/pressor choice, mechanical circulatory support, fluid management, etc.
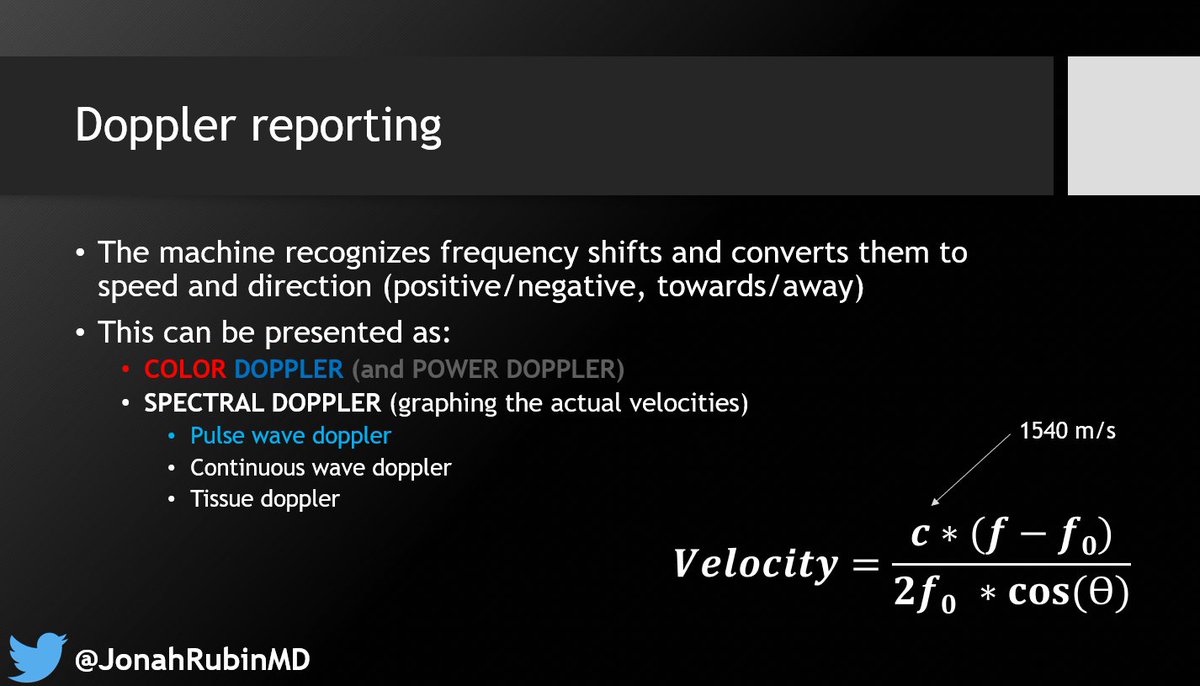
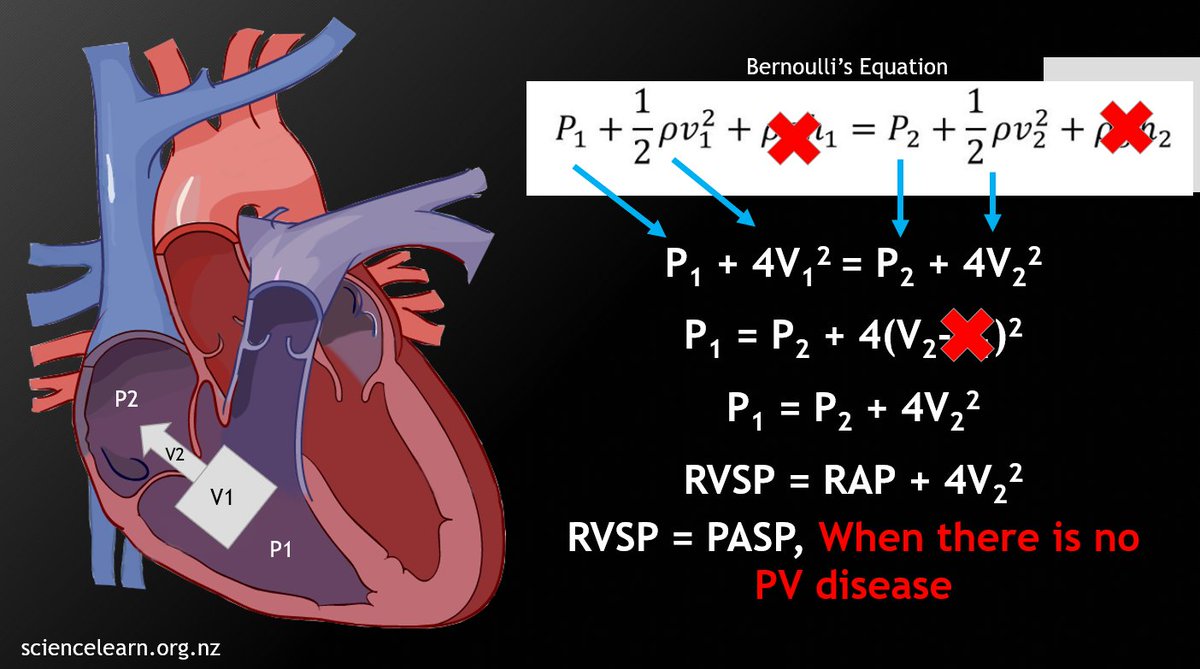
4⃣ Understand Bernoulli's equation and its modifications to know when it cannot be applied (laminar flow, massive/torrential TR, elevated proximal pressure)
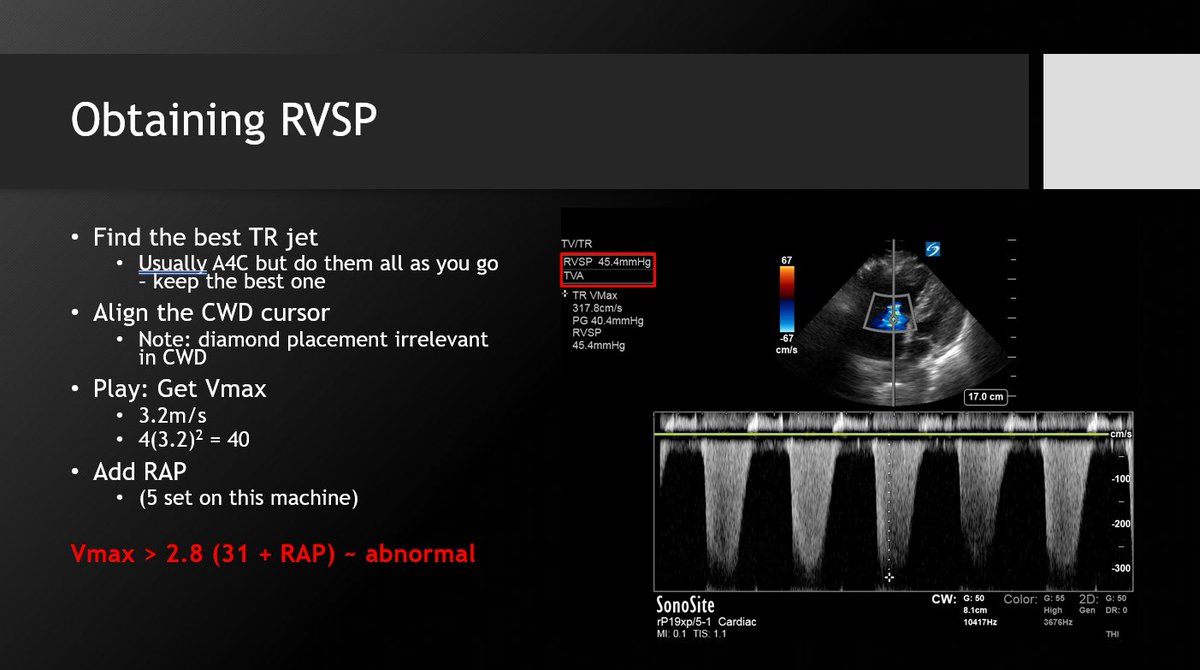
5⃣ RAP can dramatically alter the RVSP calculation; accurate assessment is crucial. The 2.1cm/50% collapse criteria are for spontaneous breathing patients only! Can use CVP if available. 
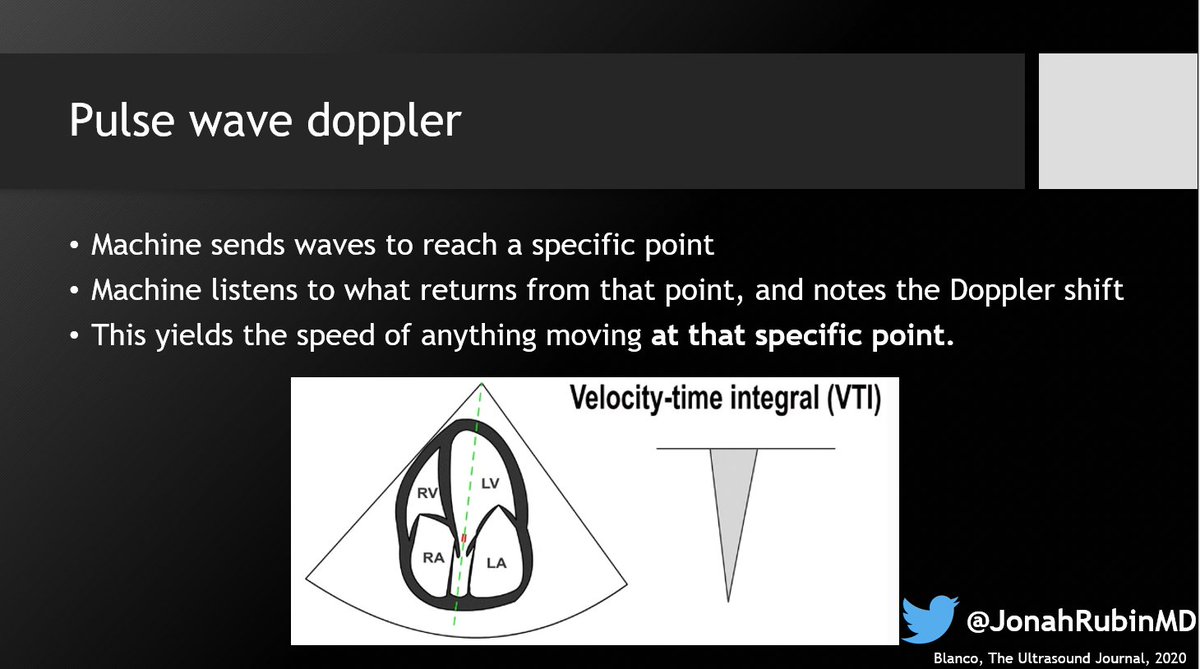
6⃣ Your best/most aligned TR jet can be in any of several views: RV inflow, PSAX-av level, A4C, even subcostal. Check them all. Keep the one with the best envelope and highest pressure. Doppler will only underestimate.
7⃣ To reiterate: Patients don't read textbooks. Application of critical care echo requires understanding the principles behind the numbers/echos to determine how to appropriately apply findings to a specific patient at a specific time.
📢 What would you add/correct/change?
• • •
Missing some Tweet in this thread? You can try to
force a refresh