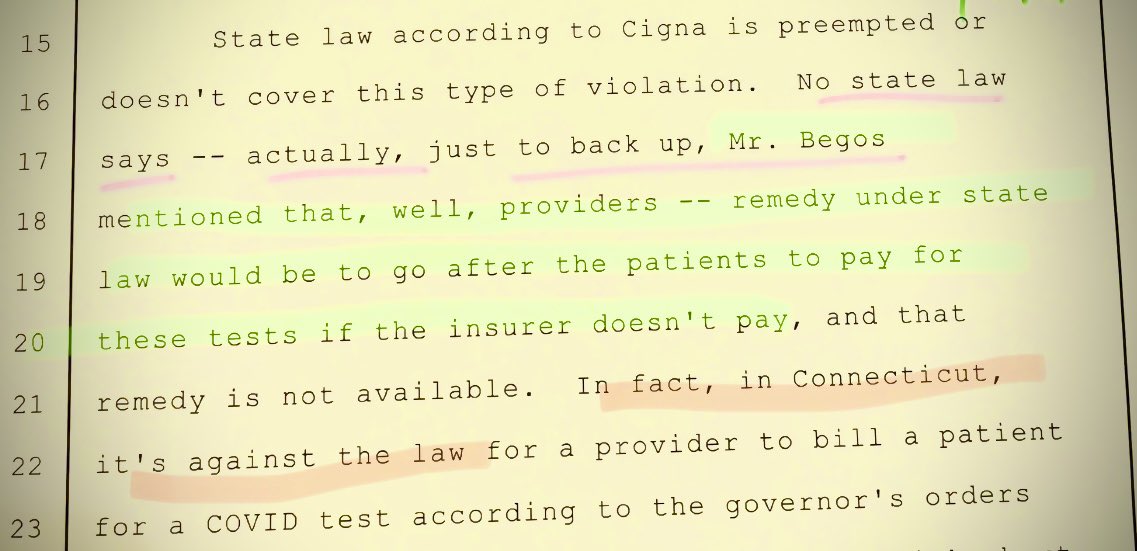
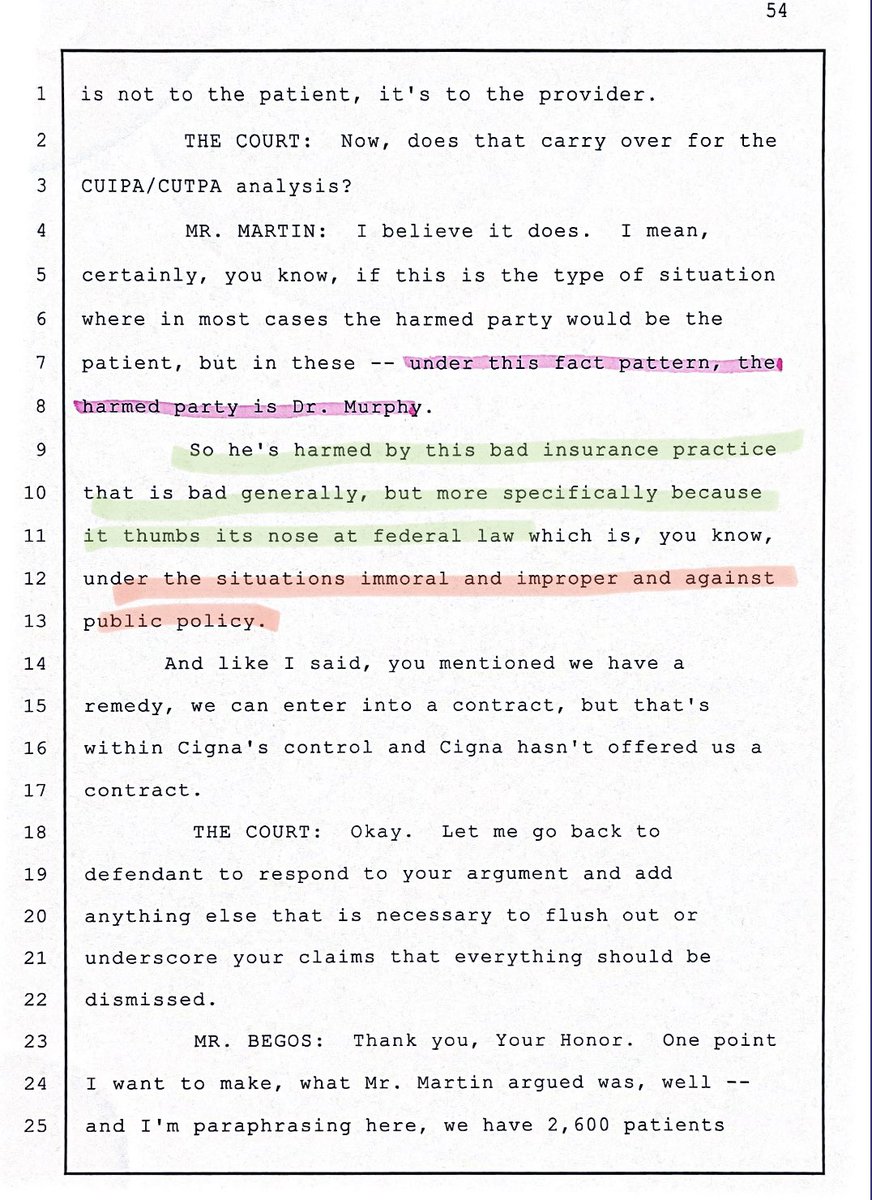
CDC: You must rule out other viruses including #influenza #RSV during pandemic when testing #COVID19 OIG: if you do that, U should be investigated for fraud and abuse. 😵💫😵💫😵💫 @BioFireDX & @QIAGEN are the best #covidtests for patients who feel sick. FULL STOP. Despite JDs advice 




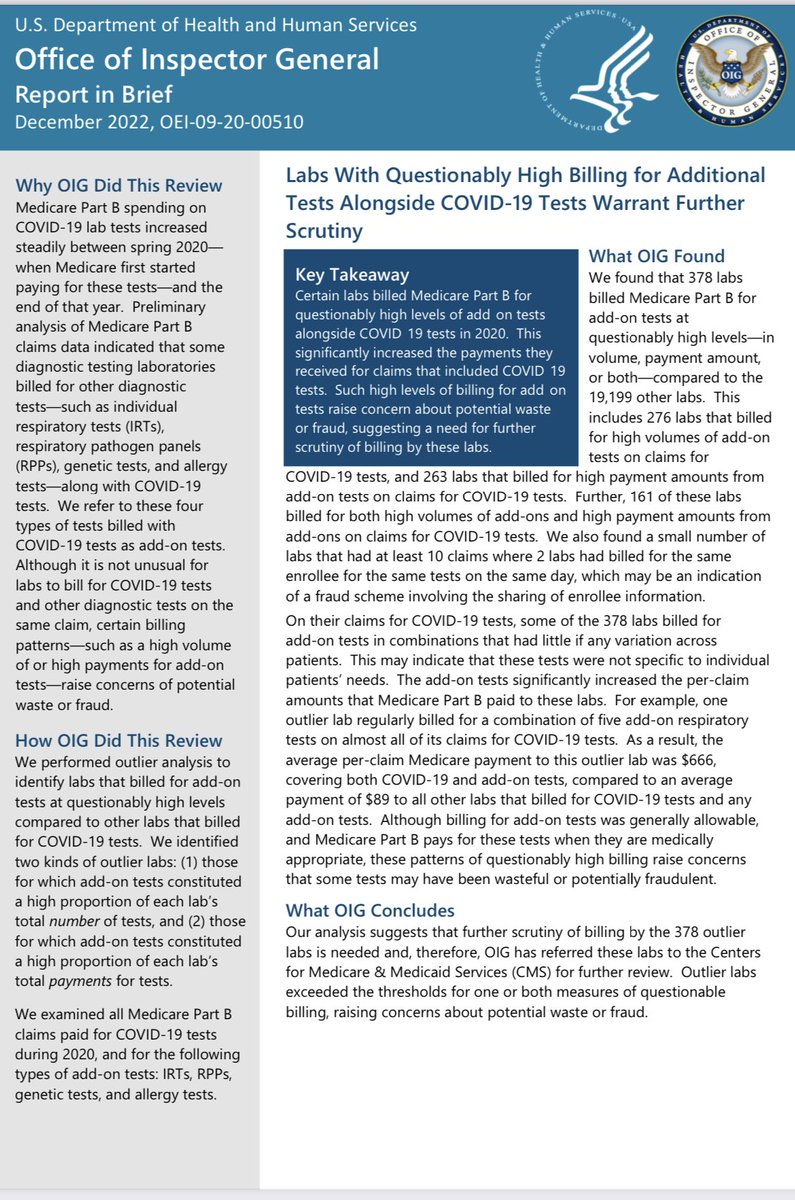
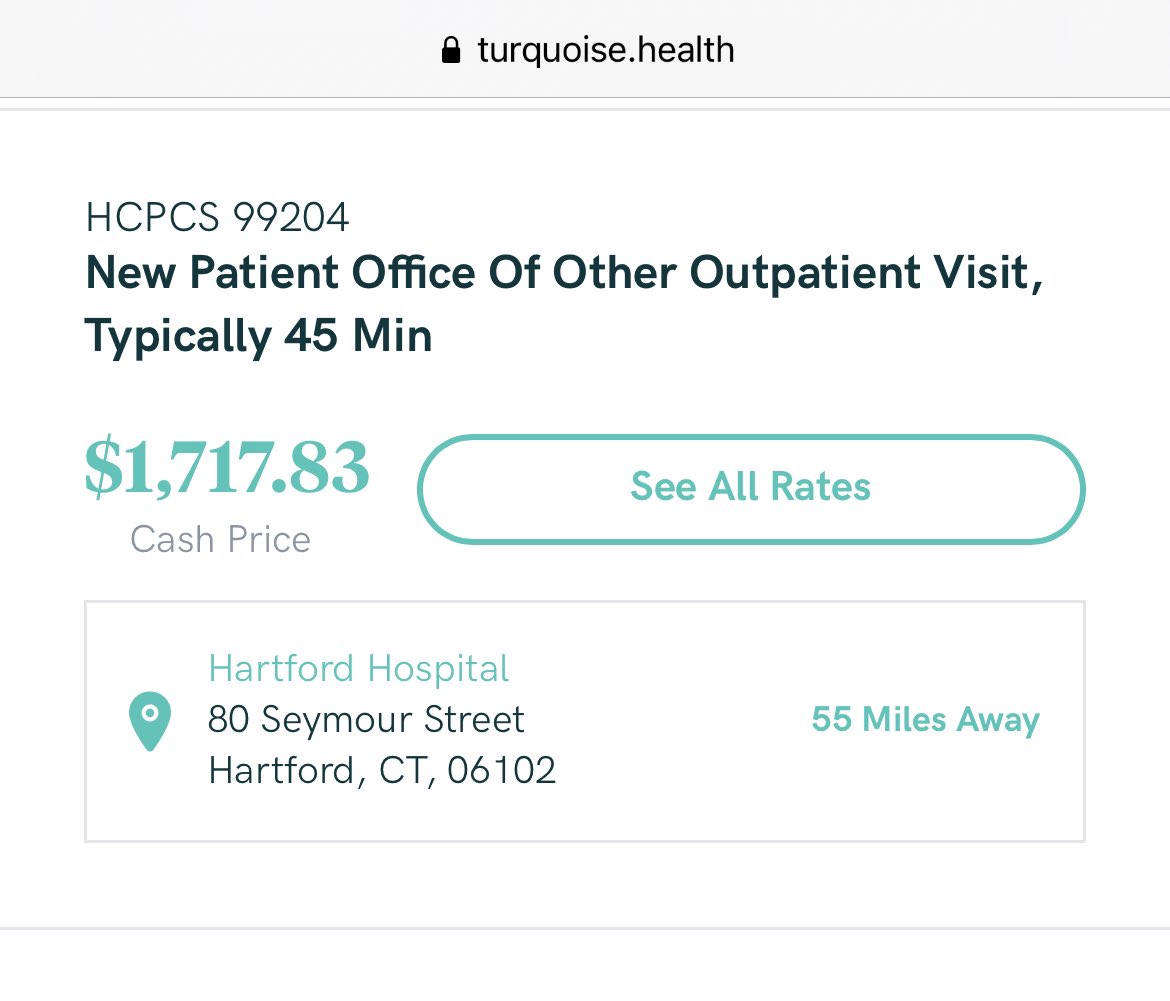
cdc.gov/flu/profession… GEEZ WHY CAN’T WE FIND COVID TESTING ANYWHERE??? Despite best medical practice, OIG wants to investigate you for doing what’s right for the patient, then the lawyers will decide. Who will offer tests with that Damocletian risk.
To be clear there is zero need to do allergy skin testing OR PGX pharmacogenomic tests when evaluating for COVID testing. Lumping the first FDA approved #COVID19 test with these shows how bad lawyers are at understanding medical care. Yet all too willing to attack good docs/labs 





HT to the readers who noticed @OIGatHHS CLASSIFIED @BioFireDX and @QIAGEN QIASTAT CORRECTLY AS COVID19 tests. WHICH THEY ARE! The limitation in their analysis is that PRIOR TO late May 87633 was the preferred code for @BioFireDX and the reps said to use this code NOT THE PLA code 



So by investigating 87633 this analysis potentially investigates millions of approved #covid19 tests. Hurting labs everywhere. We have @BioFireDX correspondence where they suggest “using whatever code pays more” 😵💫😵💫My advice, talk to labs & docs prior to any investigation.
But I still agree with them. PGX testing has no business being involved in COVID Tests. Maybe downstream when writing for Paxlovid. But not during the testing encounter. Besides, results wouldn’t be back in a timely manner.
An aside, OIG acknowledges what CDC says, nothing has changed, but they lawyerly magically wave over the fact CMS is violating FFCRA by now NOT PAYING FOR @BioFireDX OR @QIAGEN despite acknowledging it IS A COVID TEST! But who cares about CMS violating federal law when labs are! 





Don’t believe us? Read FFCRA or listen to my @tiktok_us tiktok.com/t/ZTR4gPAeX/ IF FDA APPROVED OR EUA IT MUST BE PAID. 0202U Is the first fully approved #COVIDtest yet CMS refuses to pay for it. 

After I have read through this OIG report again and again, it appears that the Lawyers again don’t understand lab medicine. THINGS ARE NOT ADD ON if they CANNOT BE SEPARATED AS A TEST. Example, if I want a Sodium level on a patient I MUST ORDER A BASIC METABOLIC PANEL.
Buckle up because I am going to drop science for OIG JDs. That Panel has a single code. 80048 it covers SODIUM, the test we want AND GLUCOSE, BUN, Creatinine, Potassium, Chloride, CO2, Calcium. Even if I ONLY WANT THE SODIUM, I MUST ORDER ALL OF THESE, why?
IT IS ONLY MANUFACTURED AS A KIT this way or as a bigger KIT. You cannot JUST GET A SODIUM. With the FDA @BioFireDX COVID19 test it is EXACTLY THE SAME! You cannot just get COVID19 alone with it. It runs as a kit. Like the BMP. But the OIG conveniently confuses add ons when.. 

They likely are not add ons @OIGatHHS because @BioFireDX in its marketing material in 2017 encouraged doctors to SPLIT THE CODES. Let me explain using the SODIUM example. But first let me explain what Ms Maxwell “found” out.
“IRTs were the most common add-on tests billed on claims for
COVID-19 tests. The average payment for an IRT was $66” these ADD ONS ARENT ADD ONS AT ALL. They are split codes. @BioFireDX in 2017 advocated using BOTH BACTERIAL CODES AND 87632 these RPP tests are key for
COVID-19 tests. The average payment for an IRT was $66” these ADD ONS ARENT ADD ONS AT ALL. They are split codes. @BioFireDX in 2017 advocated using BOTH BACTERIAL CODES AND 87632 these RPP tests are key for

#ANTIBIOTICSTEWARDSHIP and their use prior to covid pandemic is was useful to AVOID overprescribing antibiotics! And also detecting flu and RSV. But they cost money. MONEY insurers & Medicare don’t want to pay! So many insurers had medical management guidelines PREVENTING 87633
So many labs simply billed for LESS pathogens than @BioFireDX RAN AND “ADDED” the codes for the bacterial pathogens INDIVIDUALLY. Imaging IF insurers wouldn’t pay for the Chloride with the Sodium. It’s stupid, but hey, insurers man. To obtain payment, the labs would then
• • •
Missing some Tweet in this thread? You can try to
force a refresh