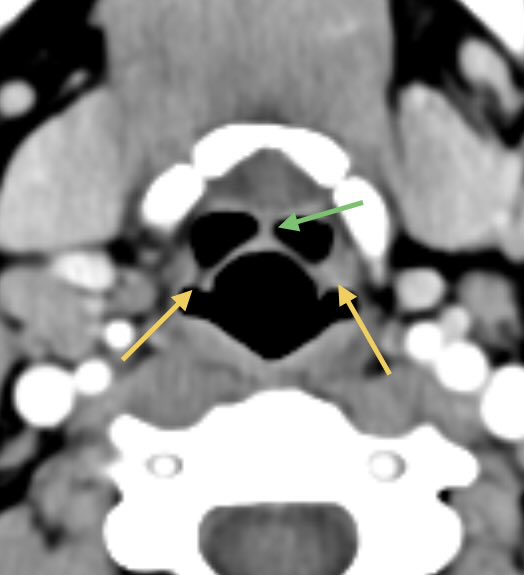
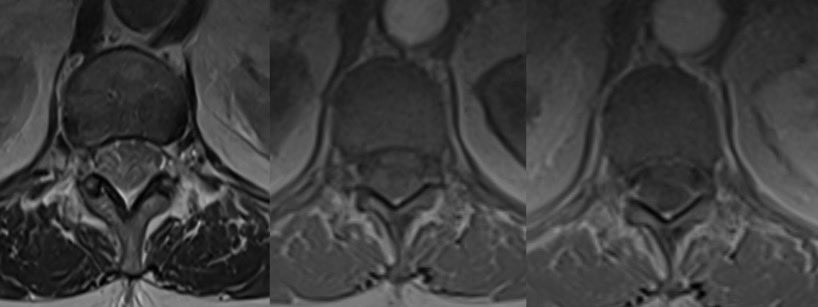
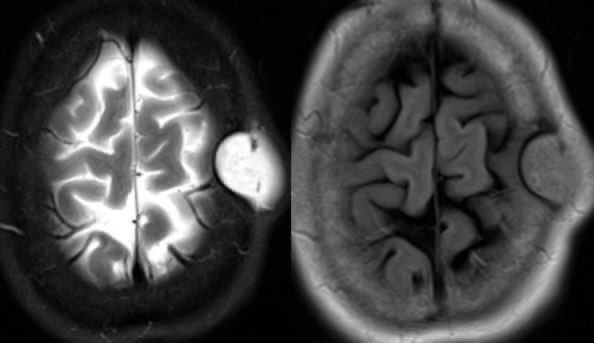
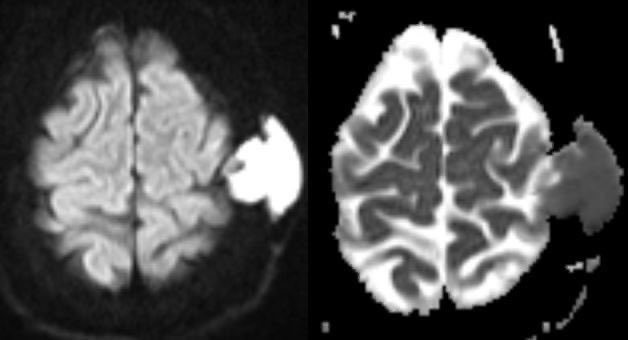
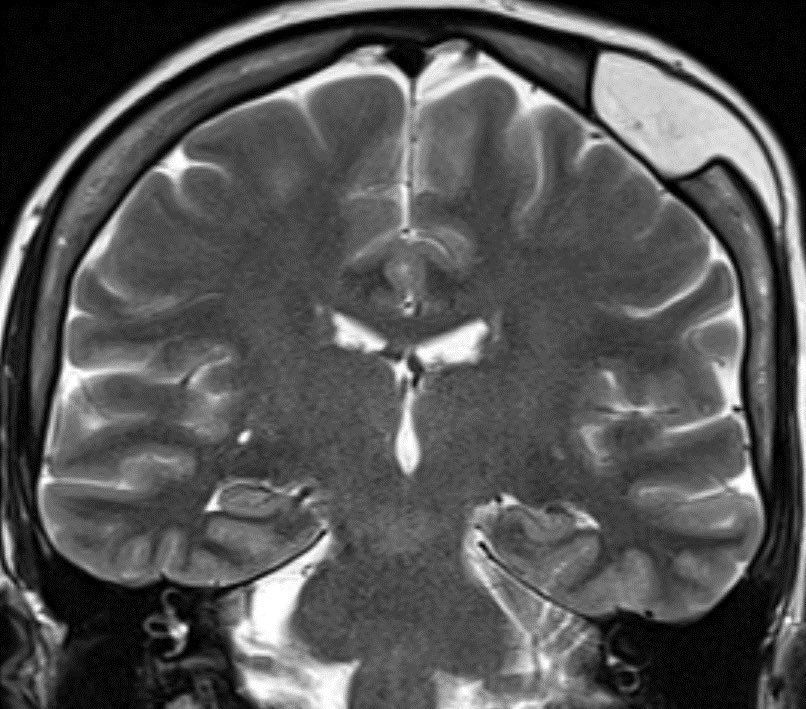
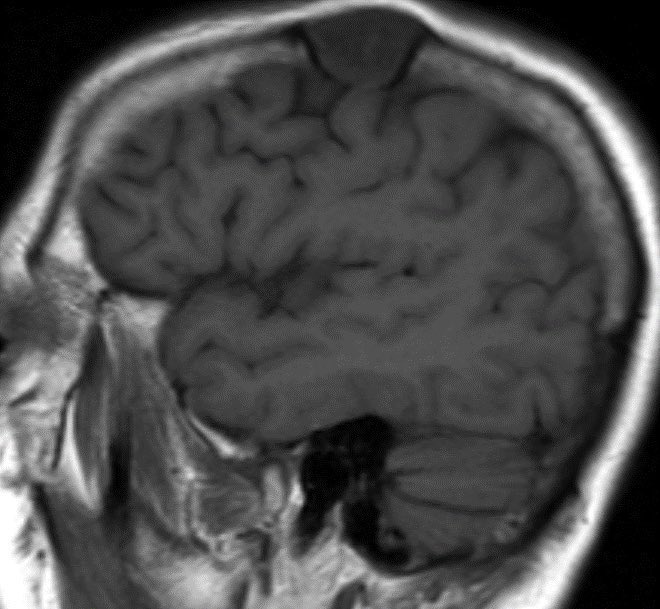
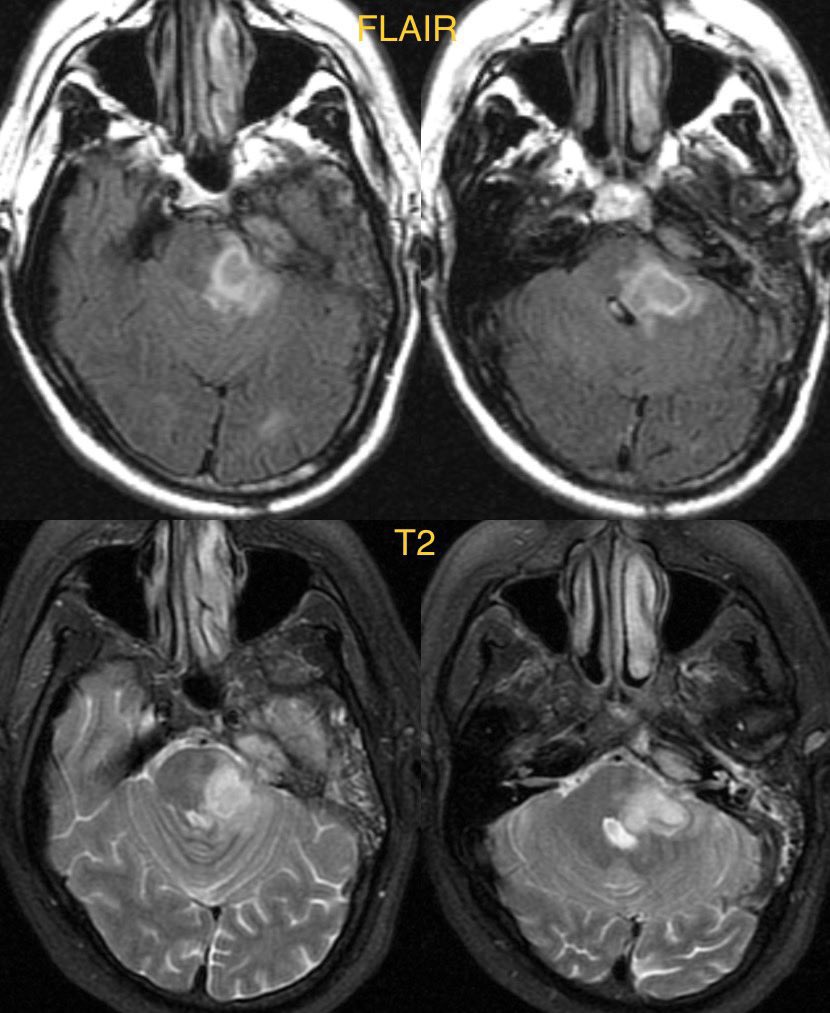
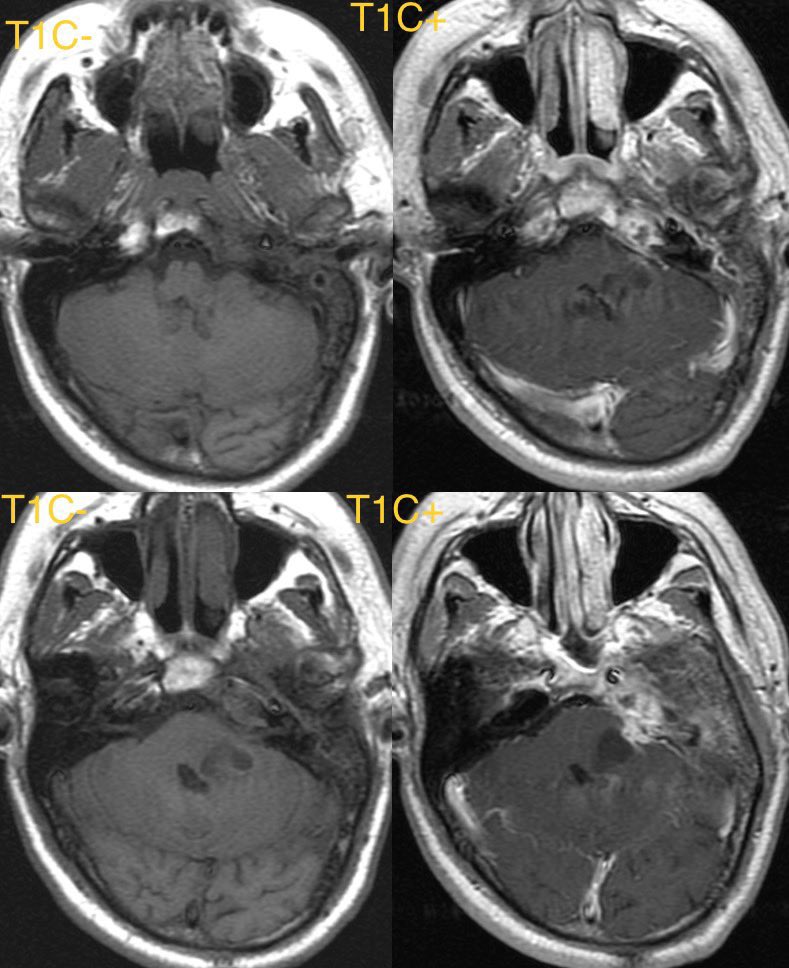
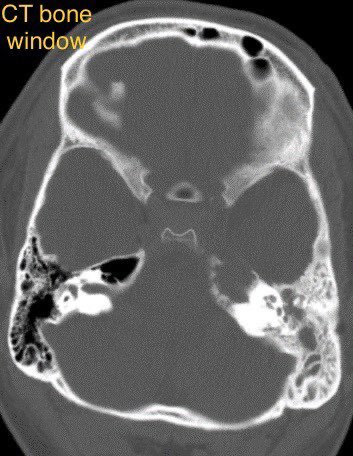
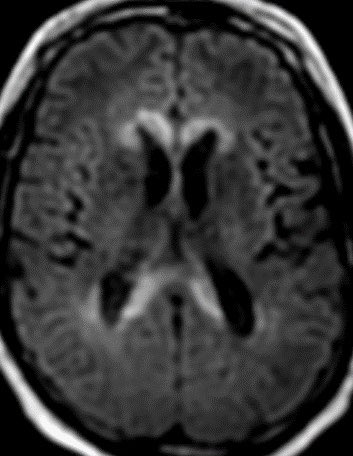
62 y/o M presents with signs of raised intracranial pressure. CT shows a hyper dense mass crossing the corpus callosum. On MR, the mass is hypointense on T2WI, restricting diffusion, and homogenously enhancing along the periventricular surface.
#radtwitter #radres #neurotwitter



#radtwitter #radres #neurotwitter



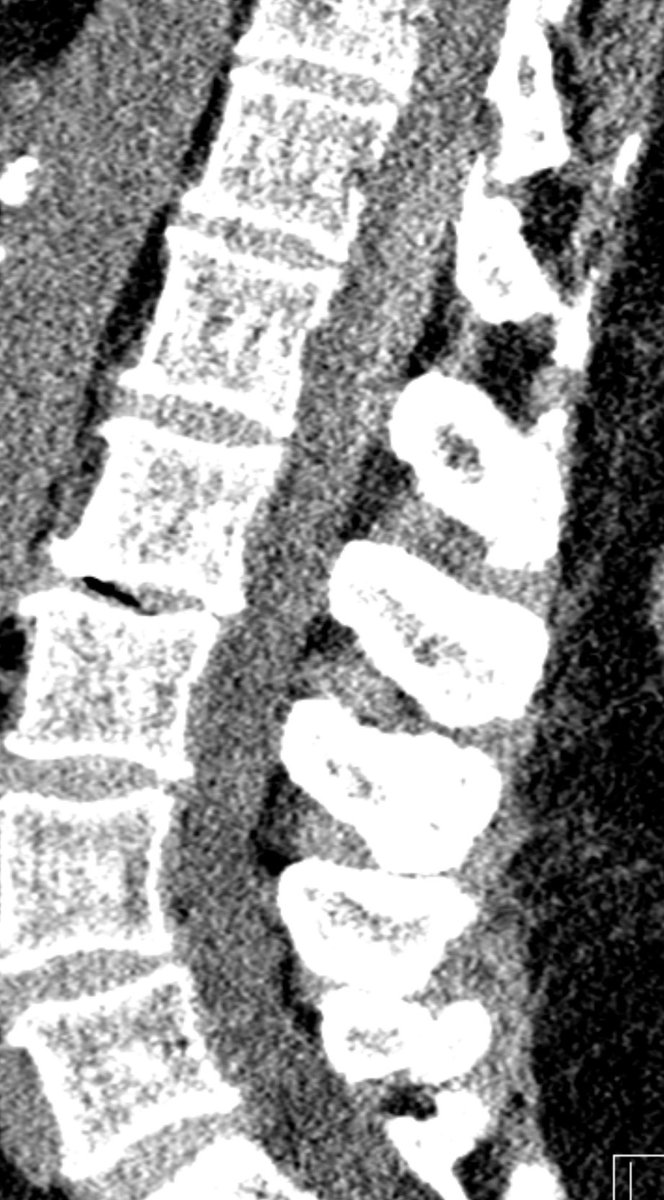
The corpus callosum is composed of very dense white matter tracks. Only aggressive tumors or lesions that effect the white matter cross the midline through the CC.
Diff Diagnosis for CC masses
High grade astrocytoma/Glioblastoma
Primary CNS lymphoma
Tumefactive Demyelination
Diff Diagnosis for CC masses
High grade astrocytoma/Glioblastoma
Primary CNS lymphoma
Tumefactive Demyelination
Dx: Primary CNS lymphoma
PCNSL has a highly variable imaging appearance. Classically, it presents as a hyperdense mass with restricted diffusion and relatively hypointensity on T2WI due to hypercellularity. The mass enhances homogeneously and may cross the CC. #Neurosurgery
PCNSL has a highly variable imaging appearance. Classically, it presents as a hyperdense mass with restricted diffusion and relatively hypointensity on T2WI due to hypercellularity. The mass enhances homogeneously and may cross the CC. #Neurosurgery
High grade astrocytoma and/or glioblastoma have more necrosis with heterogenous rather than homogenous enhancement.
Tumefactive demyelination has less mass effect relative to the size of the lesion, peripheral incomplete ring enhancement and marginal restricted diffusion. @RSNA
Tumefactive demyelination has less mass effect relative to the size of the lesion, peripheral incomplete ring enhancement and marginal restricted diffusion. @RSNA
• • •
Missing some Tweet in this thread? You can try to
force a refresh