Ambulatory Hemodialysis Unit Rounds:
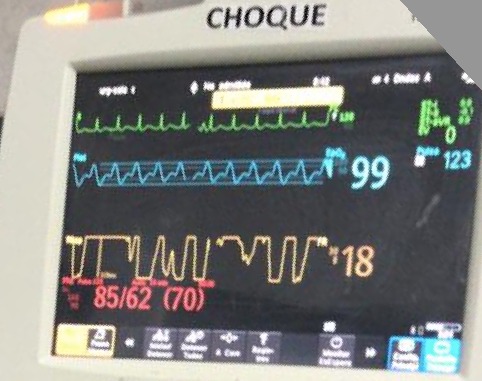
Called to see a patient with hypotension: BP 76/40,🧠 OK, CRT 5 seconds
1st step ➡️🛑Ultrafiltration + 300 ml bolus. BP 90/60
Pt is a middle aged ♂️ w ESRD and T2DM
1/9 🧵
Called to see a patient with hypotension: BP 76/40,🧠 OK, CRT 5 seconds
1st step ➡️🛑Ultrafiltration + 300 ml bolus. BP 90/60
Pt is a middle aged ♂️ w ESRD and T2DM
1/9 🧵

Now 3 kg above Dry Weight.
UF Volume so far: Only 600 ml
🔎📁 Previos HD sessions with no hypotensive episodes
1 week with URI symptoms, 2 days with dyspnea on exertion
On exam: No leg edema, Clear 🫁, JVP hard to assess (hx of multiple CVCs and central vein stenosis)
2/9
UF Volume so far: Only 600 ml
🔎📁 Previos HD sessions with no hypotensive episodes
1 week with URI symptoms, 2 days with dyspnea on exertion
On exam: No leg edema, Clear 🫁, JVP hard to assess (hx of multiple CVCs and central vein stenosis)
2/9
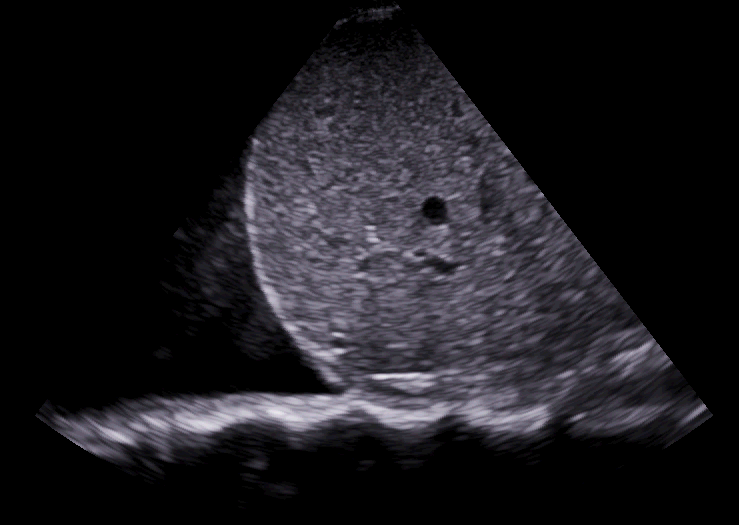
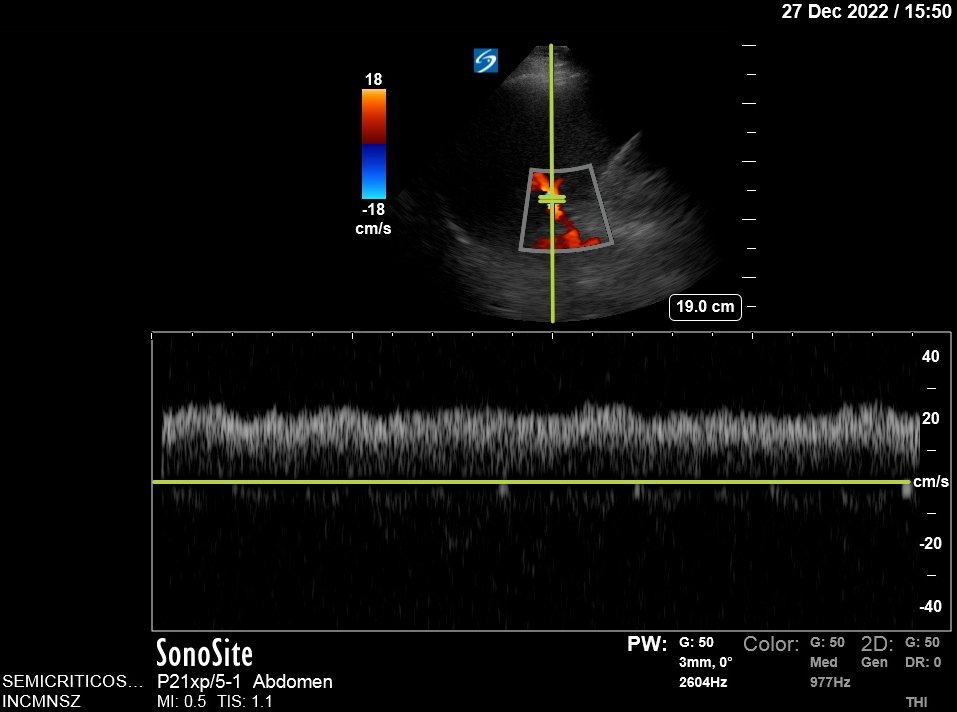
#POCUS:
Pericardial Effusion, Normal LV function, looks like there is some RV colapse
Plethoric IVC, Portal Pulsatility 39%.
A-Pattern on LUS, Small bilateral pleural effusions
🚨⬇️BP + Collapsing RV + Venous Congestion (IVC + Portal Pulsatility) suggests Tamponade!
3/9
Pericardial Effusion, Normal LV function, looks like there is some RV colapse
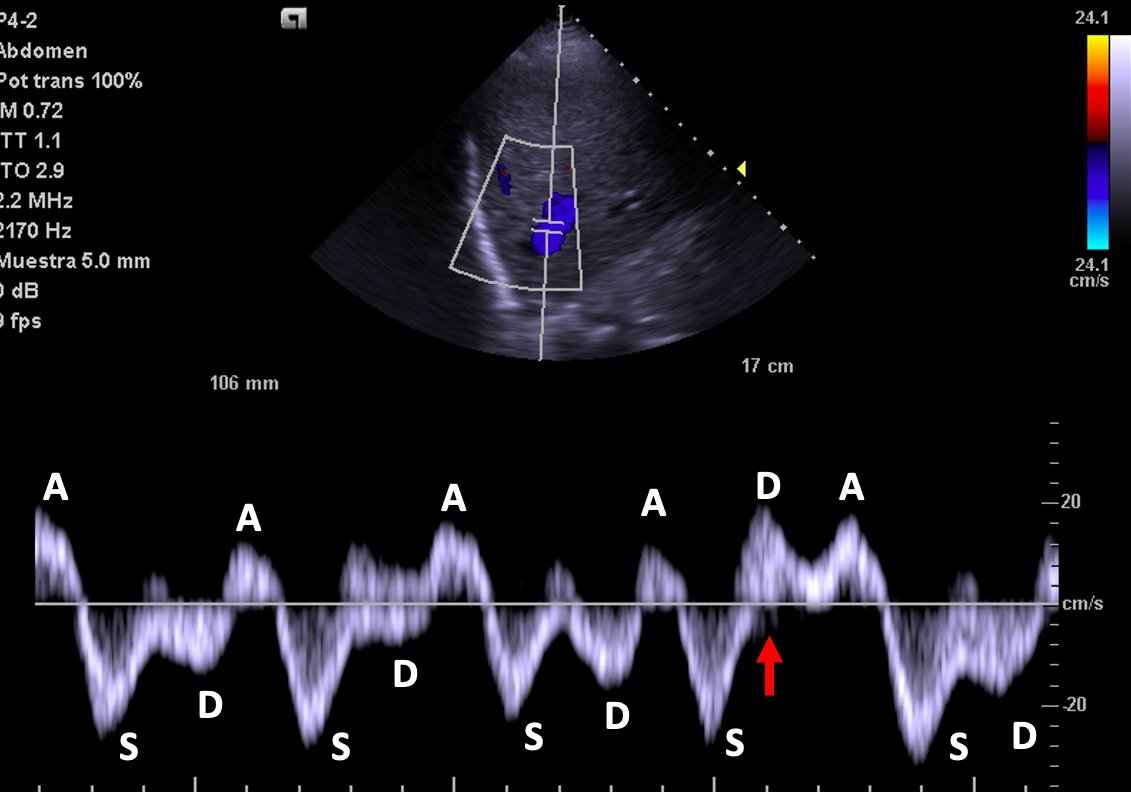
Plethoric IVC, Portal Pulsatility 39%.
A-Pattern on LUS, Small bilateral pleural effusions
🚨⬇️BP + Collapsing RV + Venous Congestion (IVC + Portal Pulsatility) suggests Tamponade!
3/9
Hepatic Vein Doppler shows characteristic D wave reversal!
Again: This is strongly suggestive of Tamponade!!🚨
4/9
Again: This is strongly suggestive of Tamponade!!🚨
4/9
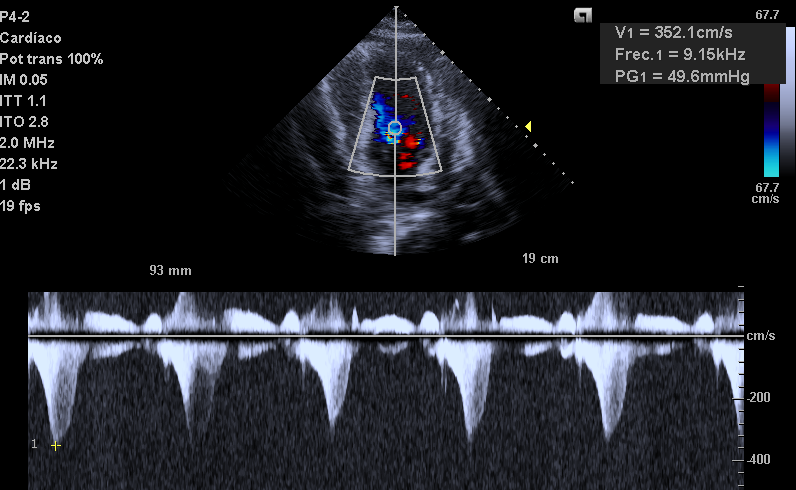
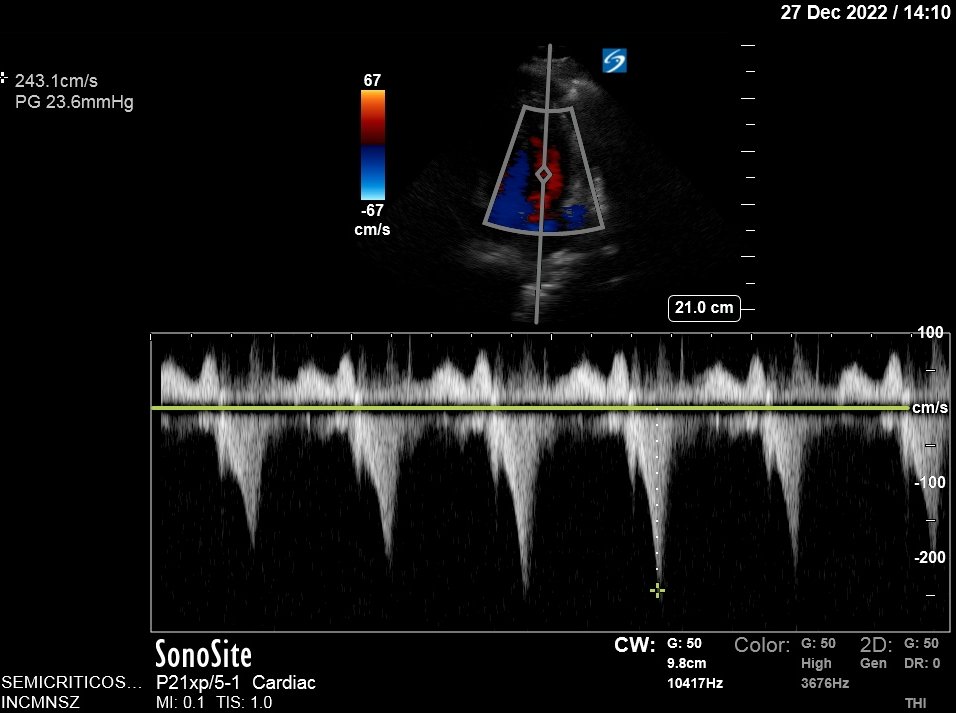
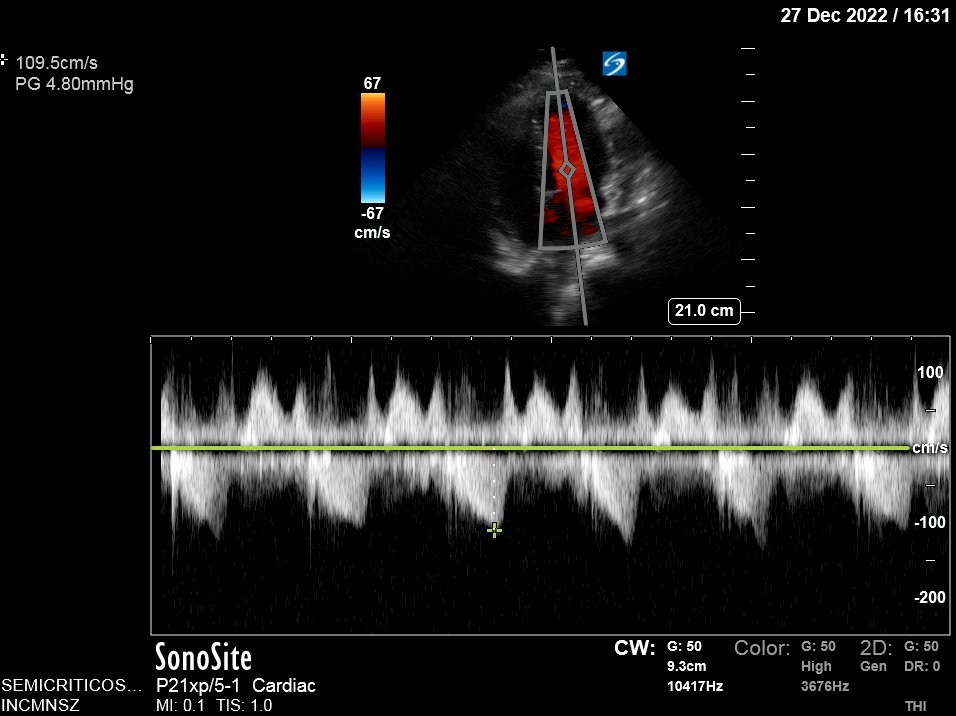
Also..LV looks very empty. LV walls can get too close together and obstruct the flow of blood!
Obstruction causes blood to speed up! (think of thumb on a hose).
Velocity is 3.5 m/s (very fast) with a gradient of 50 mmHg! This is Hemodynamically significant obstruction!
5/9

Obstruction causes blood to speed up! (think of thumb on a hose).
Velocity is 3.5 m/s (very fast) with a gradient of 50 mmHg! This is Hemodynamically significant obstruction!
5/9

In order to improve obstruction, we need to increase preload of the LV! Pericardiocentesis will achieve this (by relieving RV collapse)
In the meantime, a fluid bolus can be a temporizing measure.
More on the physiology of LV obstruction here:
6/9
In the meantime, a fluid bolus can be a temporizing measure.
More on the physiology of LV obstruction here:
https://twitter.com/ArgaizR/status/1580777299531558912?s=20&t=tN8gm3kveKRwK1gq6BXvEg
6/9
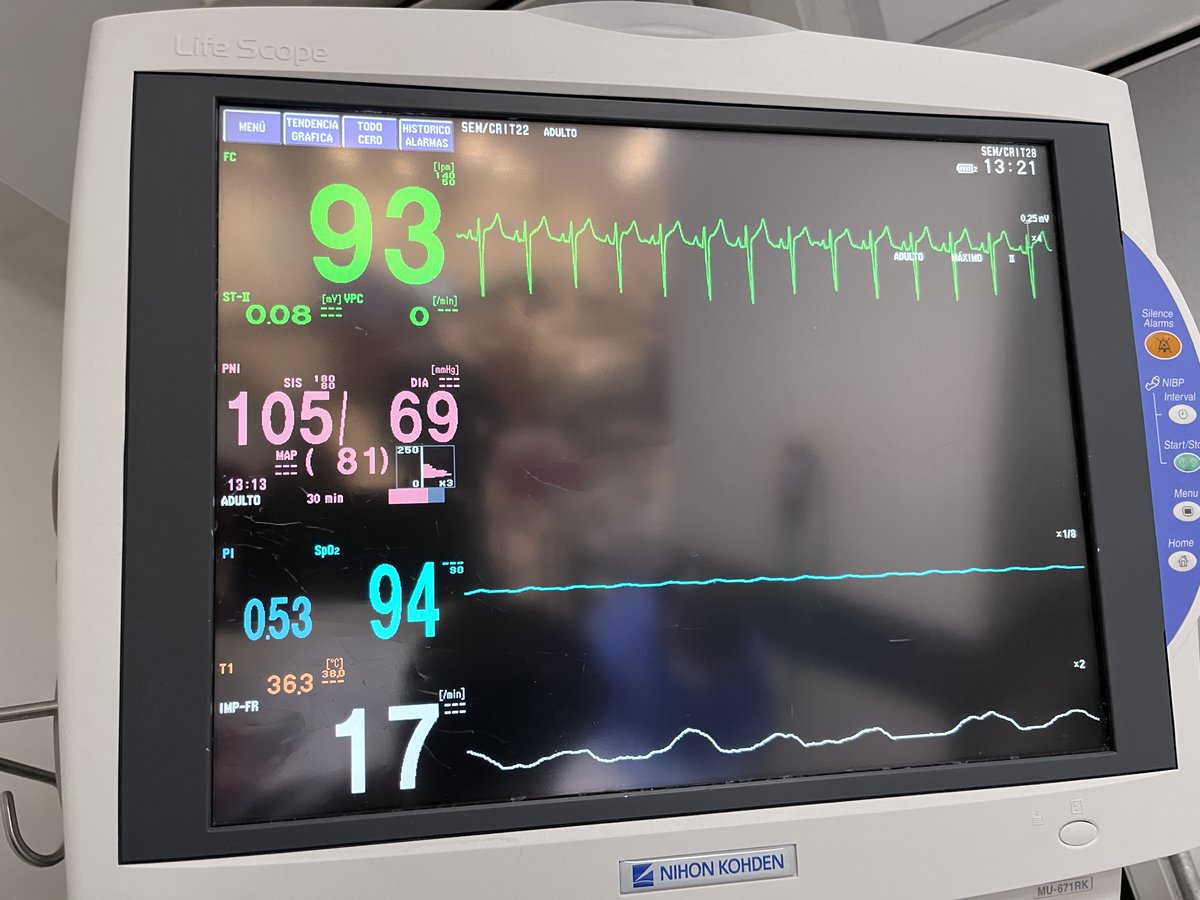
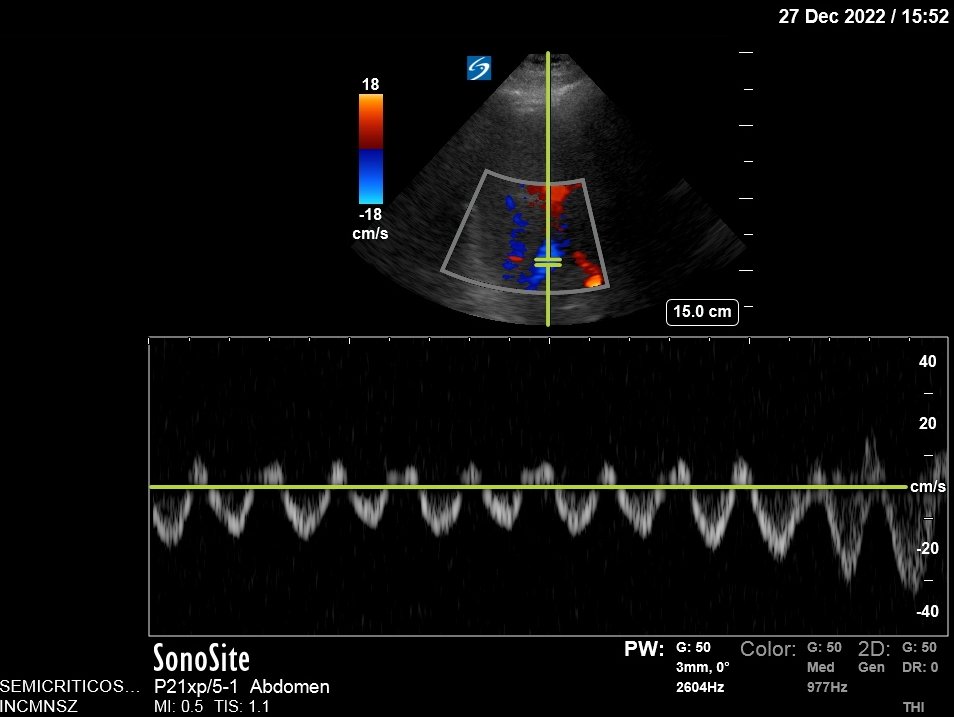
Gave an extra 300 ml fluid and arranged ICU admission!
Fluid did help: BP now 105/69, gradient improved from 50 to 24 mmHg!
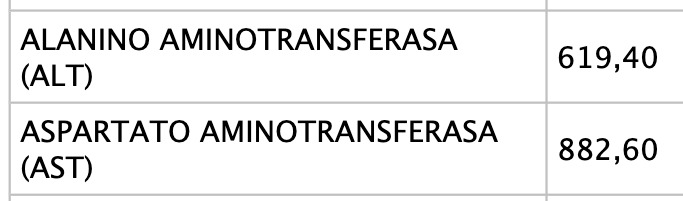
However, liver congestion got worse: Portal Vein Pulsatility now 62%. This is not good, especially since LFTs came back ⬆️⬆️⬆️
7/9



Fluid did help: BP now 105/69, gradient improved from 50 to 24 mmHg!
However, liver congestion got worse: Portal Vein Pulsatility now 62%. This is not good, especially since LFTs came back ⬆️⬆️⬆️
7/9

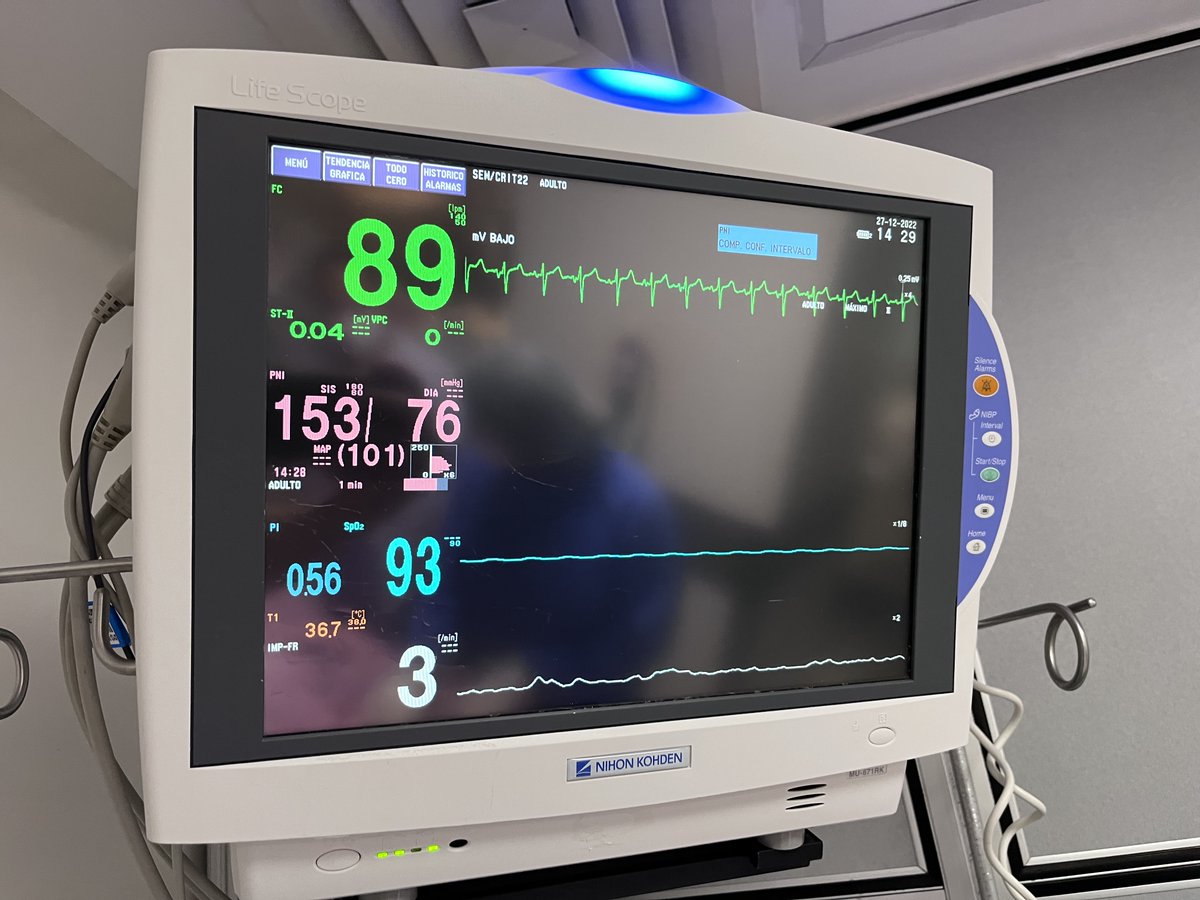
Pericardiocentesis was performed, this fixed everything!
BP now 153/76.
Portal Vein is no longer pulsatile
Hepatic vein shows no D wave reversal
Gradient is now 4.8 mmHg (Not hemodynamically significant!)
8/9



BP now 153/76.
Portal Vein is no longer pulsatile
Hepatic vein shows no D wave reversal
Gradient is now 4.8 mmHg (Not hemodynamically significant!)
8/9
Learning Points:
🔷#POCUS can help in the evaluation of intradialytic hypotension
🔷Venous congestion ≠ Volume Overload
🔷Tamponade ➡️ Low LV preload ➡️ Obstruction (if predisposing conditions)
🔷Fluids worsen congestion, but can be an adequate temporizing measure
/END
🔷#POCUS can help in the evaluation of intradialytic hypotension
🔷Venous congestion ≠ Volume Overload
🔷Tamponade ➡️ Low LV preload ➡️ Obstruction (if predisposing conditions)
🔷Fluids worsen congestion, but can be an adequate temporizing measure
/END
• • •
Missing some Tweet in this thread? You can try to
force a refresh