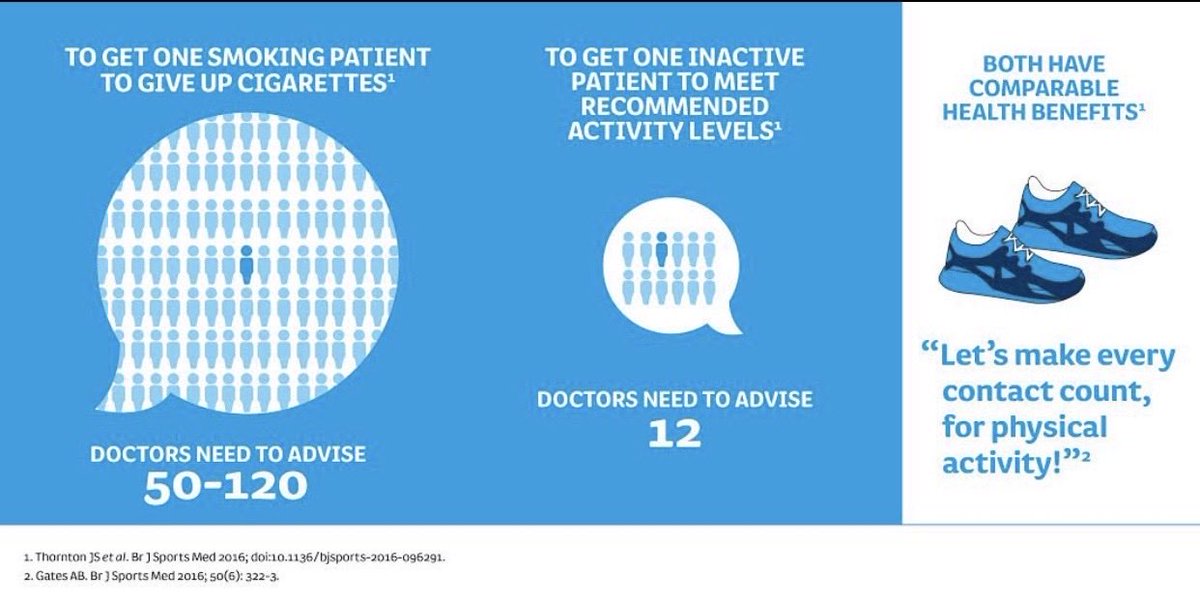
PA affects life span as much as smoking
21) A new model of practice where we guide people towards positive health. It’s not a transactional relationship - focused on episodic pain relief - it’s a long-term collaboration where we provide ongoing support for self-management to enhance health, health span & performance. 

27) with NCDs, disabling OA, falls & frailty looming improving health span & focusing on bio markers of biological age is essential. The goal is to blow out the # of candles at your next birthday for your biological not your chronological age @davidasinclair 
28) "Chronological age isn't how old we really are. It's a superficial number," said professor David Sinclair, co-director of the Paul F. Glenn Center for the Biology of Aging at Harvard Medical School.
29) "We all age biologically at different rates according to our genes, what we eat, how much we exercise and what environmental toxins we are exposed to. Biological age is what determines our health and ultimately our lifespan.
30) Biological age is number of candles we really should be blowing out. In the future, with advances in our ability to control biological age, we may have even fewer candles on our cake than the previous one."
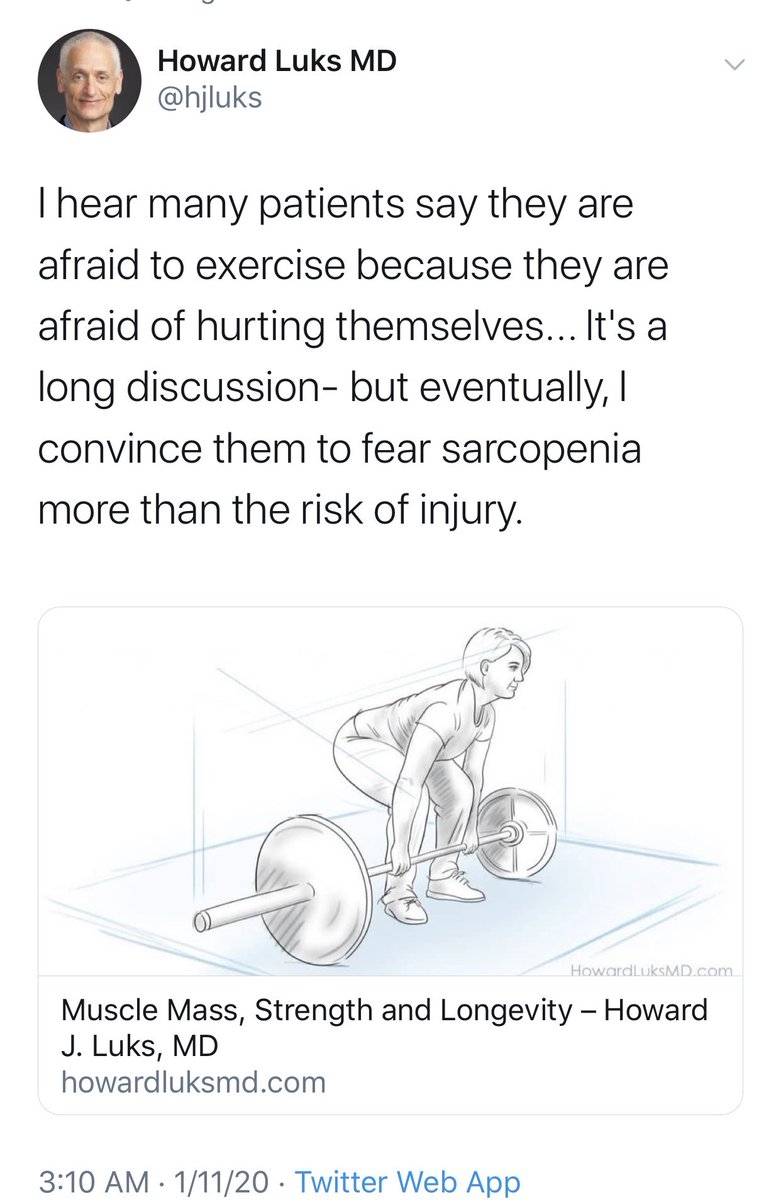
32) of exercise especially strength training benefits those over 85 then WHY do we manage people away from load w: MSK pain? 

39) Why consistency & therefore support & accountability are so crucial @Gareth_Sandford @StephenSeiler @stevemagness 

42) Let’s do this. Promoting #healthylongevity requires support, accountability, relatable goals, setting achievable targets, making it fun, community, activity > exercise, ongoing measurement, plateau & flare-up expectation. 

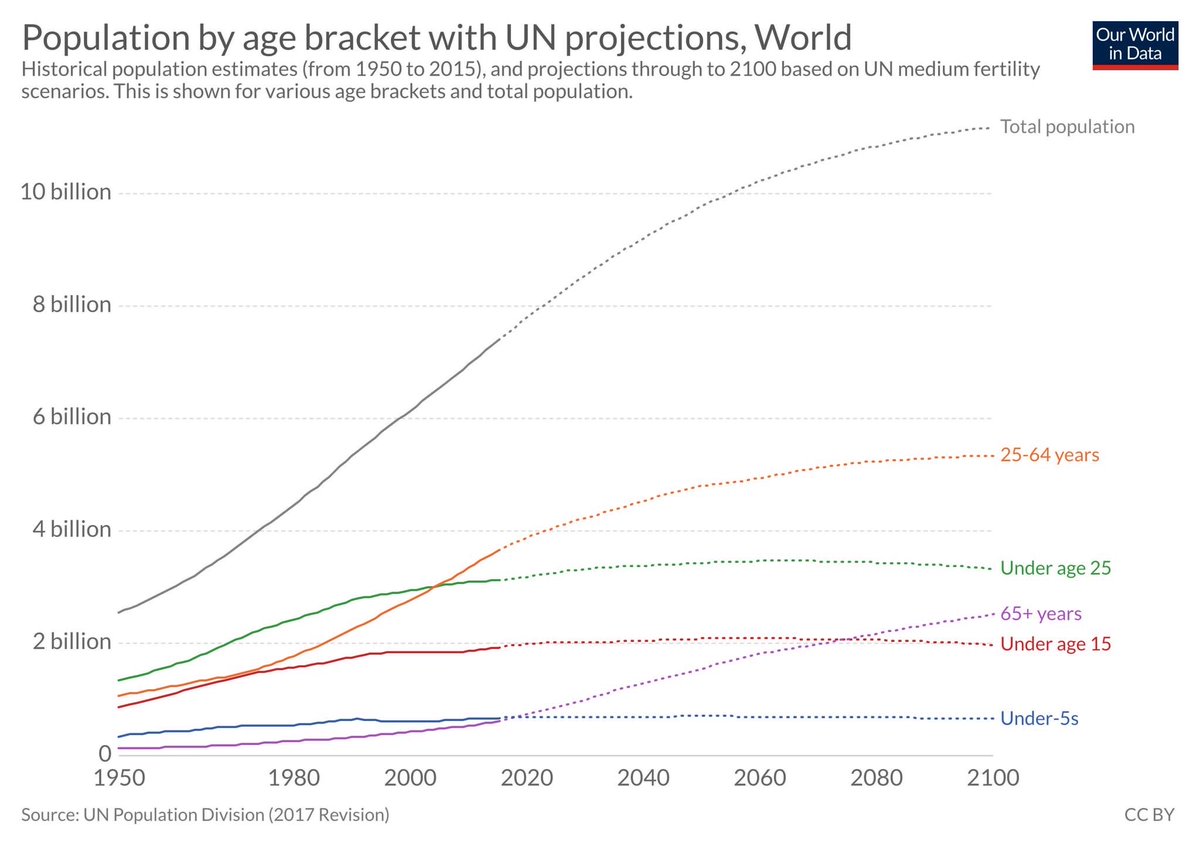
44) seeing how inactive our children are addressing PA throughout the lifespan is a crucial challenge we can all level up to together. It’s our mission statement at firstprinciplesofmovement.com to give a positive experience w/ movement & tackle “the tyranny of the mainstream”. #bowie 

45) @hjluks In middle age people are told they have “wear & tear” which is not innocent. In fact words based on over-medicalized false + diagnostic labels hurt as much as “sticks & stones” by leading to negative health procedures/interventions. @CGMMaher 

46) @doctorinigo What we invest in today determines our health in 10 years. Find a team that supports a positive health, long game mindset, rather than a negative health, transactional based “fix it” approach. 

47) I’d love to see MSK health receive the same evidence-informed, positive health, risk mitigation attention as CV health. 

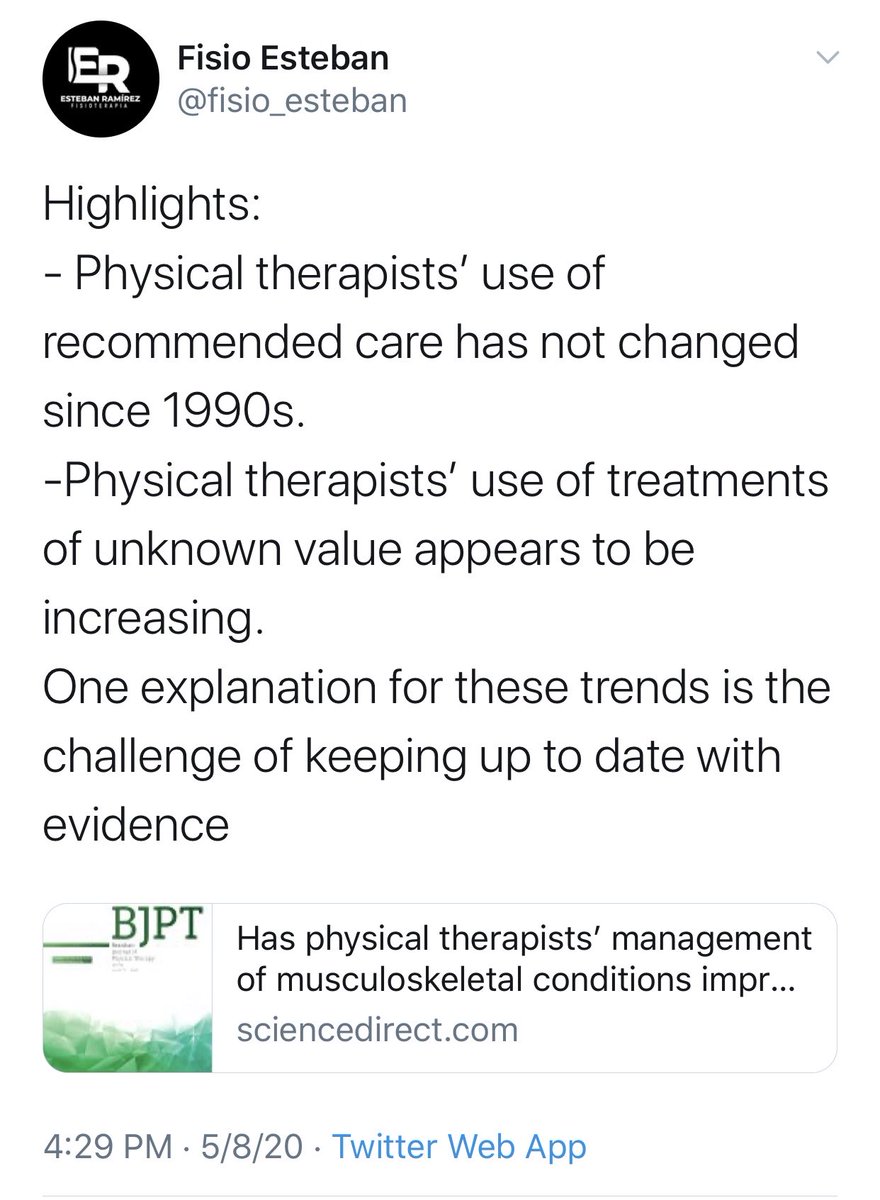
48) @giovanni_ef @zadro_josh Physio is not alone in this. DC/DO/AT/MD all have to look at their own cognitive dissonance & vested interests creating a costly blind spot driving low value & evidence-discordant MSK interventions rather than person-centered ones. 






50) @hjluks Crucial to use the gift of injury to promote positive health habits for enhancing health span sustainably rather than turn it into a promotion of temporary pain relieving transactional services. 
54) The evidence just keeps coming. This is our why at First Principles of Movement. To challenge the status quo & vested interests to give people a positive experience with movement. Join us. It will take a collective effort to move this boulder uphill.
journals.lww.com/acsm-esm/fullt…


journals.lww.com/acsm-esm/fullt…



@coachdancad @iangattphysio @chadcookpt @dr_mitch_dpt @CorKinetic @Professor_MRay @KineticImpactRP @AdamMeakins @NSaraceniPhysio @ToddHargrove
• • •
Missing some Tweet in this thread? You can try to
force a refresh