⚠️NEW PAPER⚠️
@AJCNutrition with: Mark Pereria, Cara Ebbeling, @LuciaAronica & @davidludwigmd
doi.org/10.1016/j.ajcn…
With many of my favorite things:
1) Open Science.
2)Critical analysis of high quality research.
3) Causal inference.
4) #CiCo vs #CIM
5) 1600 lines of R code.
@AJCNutrition with: Mark Pereria, Cara Ebbeling, @LuciaAronica & @davidludwigmd
doi.org/10.1016/j.ajcn…
With many of my favorite things:
1) Open Science.
2)Critical analysis of high quality research.
3) Causal inference.
4) #CiCo vs #CIM
5) 1600 lines of R code.
This is a post-hoc analysis of the DIETFITS, a high-quality RCT from @StanfordMed lead by @GardnerPhD (who kindly reviewed an earlier version of our manuscript) which compared carbohydrate vs fat restriction to achieve weight-loss during one year.
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…
This trial found non-significant weight-loss differences between both diets.
Additionally, no interaction was observed with genotype nor hyperinsulinemia.
Additionally, no interaction was observed with genotype nor hyperinsulinemia.

A later study did find weight-loss differences between diets favoring carbohydrate restriction for the intermediate time points (3 & 6 months).
doi.org/10.1002/oby.22…
doi.org/10.1002/oby.22…

However, these results were interpreted by some (@JohnSpeakman4, @KevinH_PhD ) as evidence against the Carbohydrate Insulin Model.
science.org/doi/10.1126/sc…

science.org/doi/10.1126/sc…


Of course, we could argue that absence of evidence against the null ≠ Evidence in favor of the null.
In other words, lack of evidence in favor of the #CIM is not necessarily evidence in favor of the #CiCo.
link.springer.com/article/10.100…
In other words, lack of evidence in favor of the #CIM is not necessarily evidence in favor of the #CiCo.
link.springer.com/article/10.100…
But, thanks to the openess and transparency of the DIETFITS research team who uploaded their data and R-code, we were able to test if DIETFITS data support or contradict the #CIM 🔎⚖️.
osf.io/kyiuj/?view_on…
osf.io/kyiuj/?view_on…
First, we analyzed what effect participant dropouts had on the only non-significant time point using two different multiple imputation methods.
Note these are the only results with imputed data.
ALL other analyses used the original and non-imputed dataset.
Note these are the only results with imputed data.
ALL other analyses used the original and non-imputed dataset.

Please, remember ALL methods for dealing with missing values have subjective assumptions and our method is not necessarily better than the original. It just suggests the lack of a 12-month significant difference in weight-loss could involve less stat power and diet convergence.
Since:
1) Most of the weight-loss occurred within the first 3 months.
2) It is comparable to the weight-loss at the end of the trial.
3) Most participants (90%) reached the 3-month timepoint and there is more statistical power.
Our main results are for the 3-month timepoint.
1) Most of the weight-loss occurred within the first 3 months.
2) It is comparable to the weight-loss at the end of the trial.
3) Most participants (90%) reached the 3-month timepoint and there is more statistical power.
Our main results are for the 3-month timepoint.

However, we ran ALL analyses for the 6 and 12 months too.
They show a consistent picture with the main results (and with patient dropouts reducing statistical significance).
You can find those results in our supplemental material:
ars.els-cdn.com/content/image/…
They show a consistent picture with the main results (and with patient dropouts reducing statistical significance).
You can find those results in our supplemental material:
ars.els-cdn.com/content/image/…
While having different diets, both groups ⬇️ their calorie, carbohydrate and fat intake (with different proportions).
Both groups ⬇️ their glycemic load (which considers the glycemic response to foods and their portion size). So, we combined groups for some of our comparisons.
Both groups ⬇️ their glycemic load (which considers the glycemic response to foods and their portion size). So, we combined groups for some of our comparisons.

What explains weight-loss best?
We compared different adjusted (for sex, baseline BMI, baseline calorie-intake and diet group) models and found those with carbohydrate-related variables predict weight loss better than the others.
(Larger areas = better predictive performance)
We compared different adjusted (for sex, baseline BMI, baseline calorie-intake and diet group) models and found those with carbohydrate-related variables predict weight loss better than the others.
(Larger areas = better predictive performance)

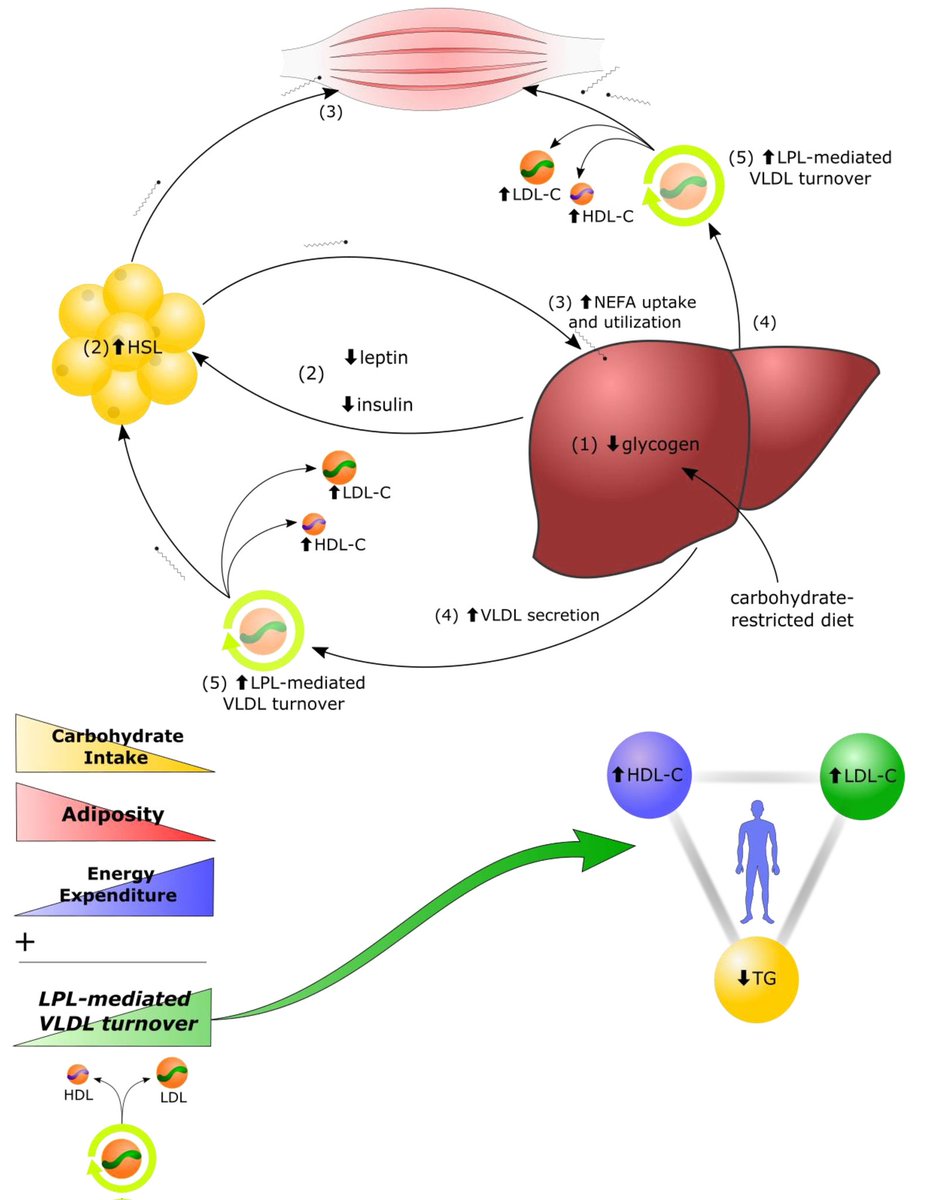
OK but, the #CIM states HIGH GLYCEMIC LOAD as the staring point of the weight-gain process.
So, what about it?
Is glycemic load reduction a significant predictor of weight-loss?
Sure, it is ✅️
(remember both groups ⬇️ their glycemic load)
So, what about it?
Is glycemic load reduction a significant predictor of weight-loss?
Sure, it is ✅️
(remember both groups ⬇️ their glycemic load)

What about fat intake?
(remember both groups ⬇️ their fat intake too)
Is it a significant predictor of weight-loss?
No, it is not ❌️
(remember both groups ⬇️ their fat intake too)
Is it a significant predictor of weight-loss?
No, it is not ❌️

Ok. Adherence is essential for any intervention.
Did those who adhered the most to their randomized intervention lose more weight?
Sure, they did ✅️
(but notice one slope is twice as steep as the other)
Did those who adhered the most to their randomized intervention lose more weight?
Sure, they did ✅️
(but notice one slope is twice as steep as the other)

But HEY!
Dietary recollection methods are often inaccurate, right?
Sure, however:
1) No reason to believe their bias would favor one group over the other (and we are analyzing all participants together).
2) We can use their lipid data as a biomarker of micronutrient intake.
Dietary recollection methods are often inaccurate, right?
Sure, however:
1) No reason to believe their bias would favor one group over the other (and we are analyzing all participants together).
2) We can use their lipid data as a biomarker of micronutrient intake.
Triglycerides/HDL is a good biomarker for carbohydrate restriction and total cholesterol is a good biomarker of fat restriction:
doi.org/10.3390/nu1212…
doi.org/10.1016/j.jand…
(since the database doesn't have total cholesterol, we used 【LDL+HDL】 as proxy)
doi.org/10.3390/nu1212…
doi.org/10.1016/j.jand…
(since the database doesn't have total cholesterol, we used 【LDL+HDL】 as proxy)
So,
Is the biomarker of carbohydrate restriction a significant predictor of weight-loss?
Sure, it is ✅️
Is the biomarker of fat restriction a significant predictor of weight-loss?
No, it is not ❌️
Is the biomarker of carbohydrate restriction a significant predictor of weight-loss?
Sure, it is ✅️
Is the biomarker of fat restriction a significant predictor of weight-loss?
No, it is not ❌️

On the other hand, one of the predictions of the #CIM is that those with the highest insulin responses should lose more weight when restricting their glycemic load.
Was that the case?
Yes, it was ✅️.
Was that the case?
Yes, it was ✅️.

Finally, we did mediation analyses.
Calorie-reduction is a significant predictor of weight-loss but its significance goes away if glycemic load is in the equation (complete mediation).
Using 100 simulations, 93% of the effect of calorie reduction is mediated by glycemic load.
Calorie-reduction is a significant predictor of weight-loss but its significance goes away if glycemic load is in the equation (complete mediation).
Using 100 simulations, 93% of the effect of calorie reduction is mediated by glycemic load.

In conclusion, carbohydrate intake predicts better weight-loss than other dietary factors. Calorie and fat reduction had little relevance.
These findings extend, NOT OPPOSE, the original conclusions of DIETFITS.
The emphasis should be on restricting processed carbohydrates.
These findings extend, NOT OPPOSE, the original conclusions of DIETFITS.
The emphasis should be on restricting processed carbohydrates.
We hope you'll find our work interesting 🙏🏼🔃🙏🏼🔃
@drjasonfung @zoeharcombe @robertlufkinmd @PeterAttiaMD @hubermanlab @garytaubes @lowcarbGP @drericwestman @DietDoctor @foundmyfitness @bschermd @KenDBerryMD @DominicDAgosti2 @Mangan150
@EricTopol @bigfatsurprise @DrAseemMalhotra
@drjasonfung @zoeharcombe @robertlufkinmd @PeterAttiaMD @hubermanlab @garytaubes @lowcarbGP @drericwestman @DietDoctor @foundmyfitness @bschermd @KenDBerryMD @DominicDAgosti2 @Mangan150
@EricTopol @bigfatsurprise @DrAseemMalhotra

MACROnutrient* 🤦♂️🙃🤣
• • •
Missing some Tweet in this thread? You can try to
force a refresh