
Not mutually exclusive, but most people said they'd prefer seeing rather than joining a discussion to analyze THAT erythritol paper, and I have some airport hours ahead...
Here go🧵.
In case you've been living under a rock, this is the paper:
nature.com/articles/s4159…
Here go🧵.
In case you've been living under a rock, this is the paper:
nature.com/articles/s4159…

Relevant disclosures for interpreting my interpretation?
I'll speak more as a clinician clinician who sees many ⬆️CVDrisk patients following a low-carb diet than as a healthy adult who follows a low-carb diet and occasionally consumes erythritol.
I'll speak more as a clinician clinician who sees many ⬆️CVDrisk patients following a low-carb diet than as a healthy adult who follows a low-carb diet and occasionally consumes erythritol.
Things I liked about the paper = ✅️.
Things I didn't like (and matter) = ⚠️
Things I didn't like (and are nitpicking) = 🧐.
🩸[] = blood concentration.
CVD = CardioVascular Disease.
MACE = Major Adverse Cardiovascular Events.
Why we "liked" erythritol in the first place?
Things I didn't like (and matter) = ⚠️
Things I didn't like (and are nitpicking) = 🧐.
🩸[] = blood concentration.
CVD = CardioVascular Disease.
MACE = Major Adverse Cardiovascular Events.
Why we "liked" erythritol in the first place?
Erythritol is an increasingly present (especially in "keto-friendly" products) sweetener.
Also, some studies showed some appealing effects.
Also, some studies showed some appealing effects.

PLUS
Since it doesn't raise insulin or glucose, #CIM people like it.
Since it doesn't "have calories" (because it's poorly metabolized and excreted almost entirely🚽), #CICO people like it too.
You don't get to see that every day🤣
Since it doesn't raise insulin or glucose, #CIM people like it.
Since it doesn't "have calories" (because it's poorly metabolized and excreted almost entirely🚽), #CICO people like it too.
You don't get to see that every day🤣
NHANES 2013-2018 (arguably, before it was "cool") showed the daily intake of erythritol could reach ~30g (this will be important later).
But erythritol is also endogenously produced in the PPP.
Thus,
🩸[erythritol] = endogenous production ➕️ intake
(also important later)
But erythritol is also endogenously produced in the PPP.
Thus,
🩸[erythritol] = endogenous production ➕️ intake
(also important later)

Now, this is one of those papers with many "nested" papers/studies/experiments. They likely were aggregated to aim at a more prestigious journal (which clearly worked).
In my opinion, its strongest point is the convergence/consistency of all studies, not their separate results.
In my opinion, its strongest point is the convergence/consistency of all studies, not their separate results.
Study 1: "Shotgun approach" (untargeted metabolomics) in people with ⬆️CVDrisk.
Result: Those with the ⬆️est 🩸[erythritol] had ⬆️CVDrisk.
Note it's 🩸[erythritol] not erythritol intake so...✅️
Result: Those with the ⬆️est 🩸[erythritol] had ⬆️CVDrisk.
Note it's 🩸[erythritol] not erythritol intake so...✅️

Small ().
✅️ their MACE definition (death, MI,stroke). Mixed outcomes often put together hardly comparable things (i.e. hospitalizations and death).
@NeuroImmuneGuy @IsaacNunezs and I published an editorial about why this was problematic in COVID RCTs.
doi.org/10.1016/j.cmi.…
✅️ their MACE definition (death, MI,stroke). Mixed outcomes often put together hardly comparable things (i.e. hospitalizations and death).
@NeuroImmuneGuy @IsaacNunezs and I published an editorial about why this was problematic in COVID RCTs.
doi.org/10.1016/j.cmi.…
So, erythritol raises your CVD risk?
Not so fast. There are other plausible explanations:
Confounding (maybe those with ⬆️CVD consume more erythritol)
Reverse causation (maybe the ⬆️CVD mileu with inflammation + insulin resistance ⬆️ the endogenous production of erythritol).
Not so fast. There are other plausible explanations:
Confounding (maybe those with ⬆️CVD consume more erythritol)
Reverse causation (maybe the ⬆️CVD mileu with inflammation + insulin resistance ⬆️ the endogenous production of erythritol).
Confounding first.
Does the ⬆️HR of ⬆️🩸[erythritol] goes ⬇️ (or away) AFTER accounting for other things that also ⬆️ CVDrisk (age, 🚻, diabetes, blood pressure, BMI, LDL, HDL, trigs & 🚬)?
No, not really.
Does the ⬆️HR of ⬆️🩸[erythritol] goes ⬇️ (or away) AFTER accounting for other things that also ⬆️ CVDrisk (age, 🚻, diabetes, blood pressure, BMI, LDL, HDL, trigs & 🚬)?
No, not really.

But👆🏻 this doesn't rule out something being intrinsically wrong with that cohort/dataset.
Study 2: Would you observe the same in other populations (🇺🇸 🇪🇺)?
Yes. And note in all cohorts the HR's magnitude is comparable and "resilient" to the adjustments.
Study 2: Would you observe the same in other populations (🇺🇸 🇪🇺)?
Yes. And note in all cohorts the HR's magnitude is comparable and "resilient" to the adjustments.

But HEY! The most important (statistically speaking) risk factor for MACE is already having some CVD history.
They adjusted for that, too.
They adjusted for that, too.

But HEY!
It's often a bad idea to break into quartiles a continuous variable like 🩸[erythritol] (doi.org/10.1016/j.ejim…).
PLUS, it actually looks like risk goes ⬆️ only for Q4.
They used 🩸 [erythritol] as a continuous variable as well.
It's often a bad idea to break into quartiles a continuous variable like 🩸[erythritol] (doi.org/10.1016/j.ejim…).
PLUS, it actually looks like risk goes ⬆️ only for Q4.
They used 🩸 [erythritol] as a continuous variable as well.

Ok, so far, it definitely looks like there is an association between ⬆️🩸[erythritol] and ⬆️CVDrisk that is resilient to all the relevant adjustments.
But, you know... correlation≠causation.
You need to show a plausible pathophysiology link between these two.
But, you know... correlation≠causation.
You need to show a plausible pathophysiology link between these two.

How can ⬆️erythritol cause ⬆️🧠🫀 infarctions?
How can we address the possibility of the ⬆️CVDrisk mileu raising ⬆️🩸[erythritol] instead?
Study 3: Platelet studies.
Does erythritol make your platelets "stickier"?
Yeah, it looks like it does.
How can we address the possibility of the ⬆️CVDrisk mileu raising ⬆️🩸[erythritol] instead?
Study 3: Platelet studies.
Does erythritol make your platelets "stickier"?
Yeah, it looks like it does.
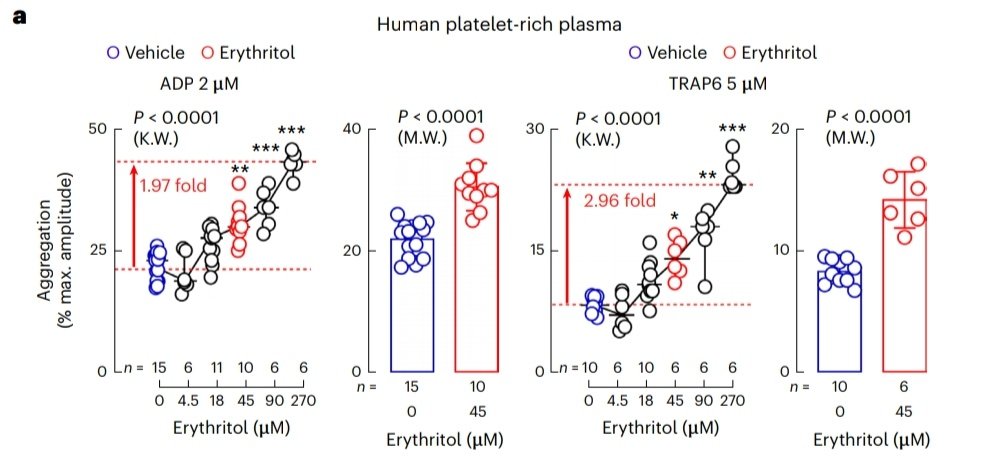
But, you know, this is really "just" a functional observation.
What if they messed up their experiments or there is something wrong with the equipment they used?
Anyone who has worked in a "wet-lab" knows this is more than a possibility.
What if they messed up their experiments or there is something wrong with the equipment they used?
Anyone who has worked in a "wet-lab" knows this is more than a possibility.
Would you observe other platelet aggregation related phenomena supporting "platelets are stickier when exposed to the same 🩸[erythritol]" with different methods, equipment?
In other words, with independent sources of error?
Study 4: Ca, IIb/IIIa & p-selectin.
Yup.
In other words, with independent sources of error?
Study 4: Ca, IIb/IIIa & p-selectin.
Yup.

Hold on👆🏻... Maybe this is just an interaction between erythritol and platelets from people with ⬆️CVDrisk.
Nope, they used platelets from healthy volunteers, so... ✅️
Nope, they used platelets from healthy volunteers, so... ✅️

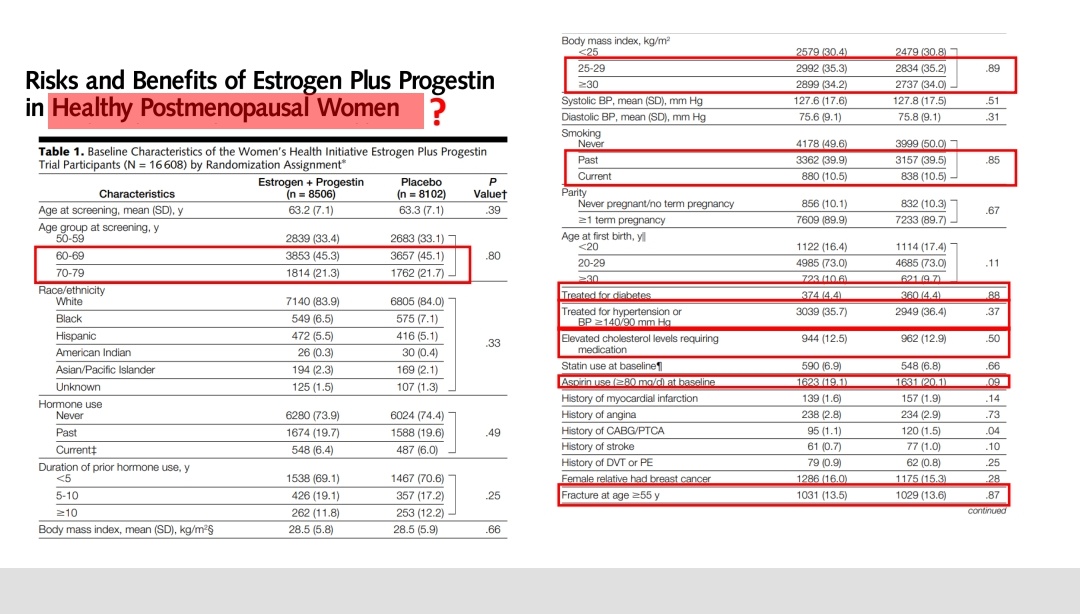
⚠️This is my biggest concern about his paper. I think it is necessary to actually show healthy=healthy.
You know... there are famous examples of "classic" RCTs with controversial definitions for "healthy."
You know... there are famous examples of "classic" RCTs with controversial definitions for "healthy."
Now, coagulation is way more than platelets. It involves whole blood and a vessel.
Did they observe phenomena supporting "stickier" 🩸when exposed to erythritol?
Study 5: In vivo platelet adhesion in human physiological conditions.
Study 6: Vessel injury 🐁 model.
Yeah.
Did they observe phenomena supporting "stickier" 🩸when exposed to erythritol?
Study 5: In vivo platelet adhesion in human physiological conditions.
Study 6: Vessel injury 🐁 model.
Yeah.

How "easy" it is to get that 🩸[erythritol]?
They used a drink with 30gr (because of NHANES 2013-2018).
Since vey few products disclose their erythritol content, it could not be intuitive to all how 30gr compares to an average "keto-snack".
Check it. It's comparable so...✅️
They used a drink with 30gr (because of NHANES 2013-2018).
Since vey few products disclose their erythritol content, it could not be intuitive to all how 30gr compares to an average "keto-snack".
Check it. It's comparable so...✅️

Study 7: Erythritol drinks for healthy volunteers.
🩸[erythritol] ⬆️1000x for many hours and stayed above the levels they saw in their coagulation studies induced platelet responses.
Maybe you don't have a 30gr snack daily, but what about one with ~10gr?
🩸[erythritol] ⬆️1000x for many hours and stayed above the levels they saw in their coagulation studies induced platelet responses.
Maybe you don't have a 30gr snack daily, but what about one with ~10gr?

Their fasting levels were comparable to the cohort low risk quartiles, and postprandial levels were like the Q4 ones.✅️
BUT!!!
Isn't n=8 too small? Their response is consistent, 8M wouldn't change this result.
Shouldn't they randomize them? Not for this research question.
BUT!!!
Isn't n=8 too small? Their response is consistent, 8M wouldn't change this result.
Shouldn't they randomize them? Not for this research question.
Is this paper perfect? Far from it (there's no such thing).
Are their pre-registration inconsistencies criticizable? Sure.
However, I really don't think all the points of criticism I've found or read from others invalidate their conclusions.
Are their pre-registration inconsistencies criticizable? Sure.
However, I really don't think all the points of criticism I've found or read from others invalidate their conclusions.
Many said they were surprised and/or criticized my conclusion of "these data being enough to recommend against it".
Let me elaborate (and remember the white-coat disclosure).
Let me elaborate (and remember the white-coat disclosure).
Do I believe after reading this paper that erythritol should be banned from food and you'll get a stroke if indulge a keto snack? Of course not.
Will I generally avoid erythritol even with my (so far) ⬇️CVDrisk? Yeah, probably.
Will I generally avoid erythritol even with my (so far) ⬇️CVDrisk? Yeah, probably.
Then why the hard line?
As mentioned, what I find convincing is the convergence of all their experiments (not their individual results).
What are the costs of avoiding erythritol? None, zero, zilch, nada.
I already focused on encouraging real-food anyway.
As mentioned, what I find convincing is the convergence of all their experiments (not their individual results).
What are the costs of avoiding erythritol? None, zero, zilch, nada.
I already focused on encouraging real-food anyway.
What are the benefits? For someone with high inflammation and/or insulin resistance... This COULD mean less risk of having to face a pretty bad scenario.
Lowering (even if just mildly or potentially) CVDrisk for free?
Yeah I'll take that deal.
Lowering (even if just mildly or potentially) CVDrisk for free?
Yeah I'll take that deal.
Thank you if you made it all the way down to here.
I hope you enjoyed this 🧵 interesting. Let me know if you'd join a more in-depth discussion.
I am sure not everyone will agree with that (which is, of course, fine). Let's just at least try to keep a constructive debate.
I hope you enjoyed this 🧵 interesting. Let me know if you'd join a more in-depth discussion.
I am sure not everyone will agree with that (which is, of course, fine). Let's just at least try to keep a constructive debate.
My 🧵 was incorrectly pasted. You can follow what's next here.
https://twitter.com/AdrianSotoMota/status/1630974021616402446?t=orcA67TDLYt95ykncYPKPw&s=19
• • •
Missing some Tweet in this thread? You can try to
force a refresh













