Young ♀️ w CKD on HD, seen in Cardiorenal clinic
Pt had torrential tricuspid regurgitation due to CVC induced leaflet perforation ➡️ She underwent tricuspid valve replacement surgery 🫀🔪
However, 1 month after discharge she is still using a wheelchair 🤔
1/12🧵
Pt had torrential tricuspid regurgitation due to CVC induced leaflet perforation ➡️ She underwent tricuspid valve replacement surgery 🫀🔪
However, 1 month after discharge she is still using a wheelchair 🤔
1/12🧵
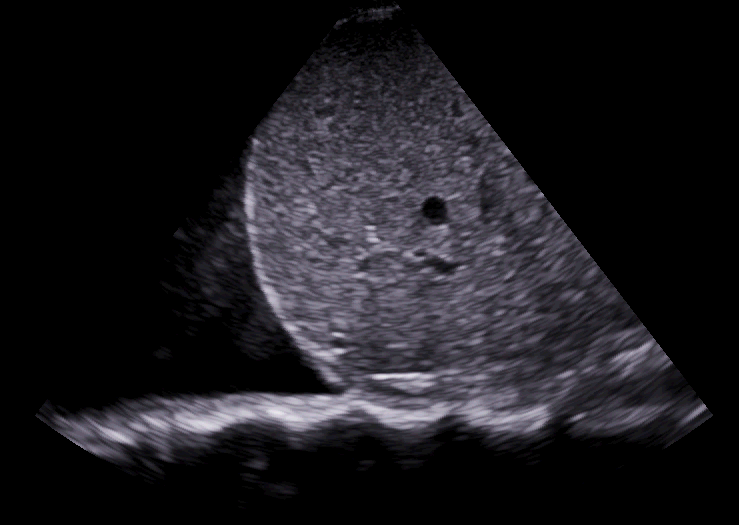
#POCUS above shows plethroic, non-collapsible IVC and Hepatic Veins
Did surgery work?
Is there residual tricuspid regurgitation?
#Echofist (PLAx RV view + A4ch) color Doppler lets us see there is no or minimal TR
Prosthetic valve seems to be working
2/12
Did surgery work?
Is there residual tricuspid regurgitation?
#Echofist (PLAx RV view + A4ch) color Doppler lets us see there is no or minimal TR
Prosthetic valve seems to be working
2/12
But there is still venous congestion. In fact congestion is significant, take a look at portal vein Doppler 👇
Pulsatility Fraction = 40%, this means there is significant venous congestion. Why?
Is this just volume overload? Should we probe a lower dry weight?
3/12
Pulsatility Fraction = 40%, this means there is significant venous congestion. Why?
Is this just volume overload? Should we probe a lower dry weight?
3/12

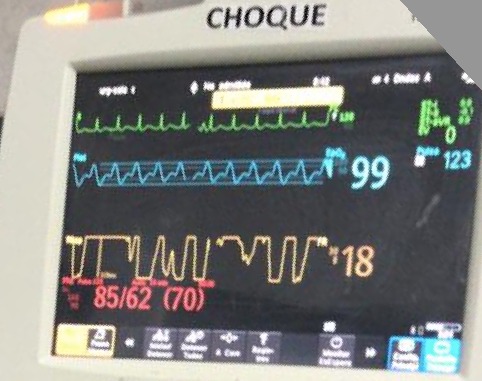
📂Chart review revealed patient has had borderline low pre-dialysis BP and several episodes of Intradialytic hypotension.
Lowering dry weight doesn't look feasible.
Let's take a closer look at the🫀: LV function looks OK. (RV fx also looked OK)
4/12
Lowering dry weight doesn't look feasible.
Let's take a closer look at the🫀: LV function looks OK. (RV fx also looked OK)
4/12
An important clue 🔎 was observed when assessing flow to the pulmonary artery.
Doppler at the Right Ventricular Outflow Tract (RVOT) shows mid-systolic Notch ➡️ This strongly suggests increased Pulmonary Vascular Resistance!
5/12

Doppler at the Right Ventricular Outflow Tract (RVOT) shows mid-systolic Notch ➡️ This strongly suggests increased Pulmonary Vascular Resistance!
5/12


Also, pulmonary acceleration time is 60 msec! These all suggests there is underlying severe PAH!
After this assessment, something about the patient should immediately catch your eye!
She had a Brachiobasilic fistula on her right arm 🤯!
6/12
After this assessment, something about the patient should immediately catch your eye!
She had a Brachiobasilic fistula on her right arm 🤯!
6/12

AV fistula is one of the five more common causes of High Output Heart Failure (HOHF)!
The risk for this disease increases with increased AV fistula flow.
Brachial AVFs are associated with higher CO and higher risk of RV disfunction than Radial AVFs!
7/12


The risk for this disease increases with increased AV fistula flow.
Brachial AVFs are associated with higher CO and higher risk of RV disfunction than Radial AVFs!
7/12



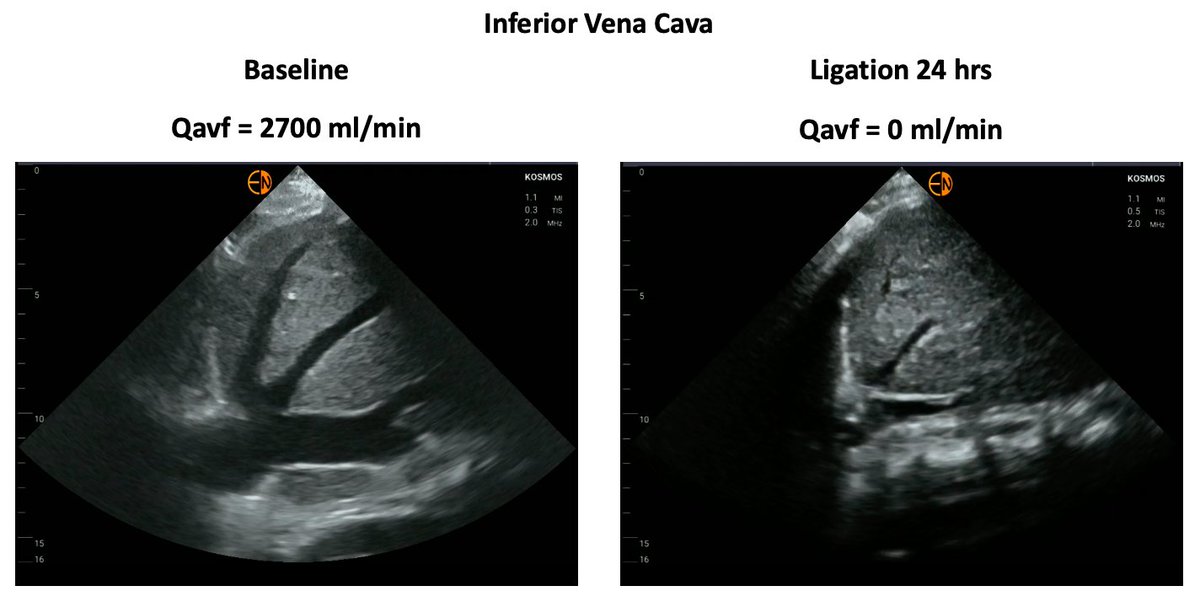
AVF Flow > 2 L/min or AVF flow > 30% of cardiac output are commonly used criteria for defining a hemodynamically significant flow
Doppler assessment of AVF flow can be performed at the feeding artery (Brachial artery) 👇
8/12

Doppler assessment of AVF flow can be performed at the feeding artery (Brachial artery) 👇
8/12


Doppler evaluation in this patient revealed a high flow fistula (2.7 L/min) and High Cardiac Output (7 L/min)!
Also AVF flow is 38% of cardiac output!
HOHF caused by AVF was strongly suspected!
9/12

Also AVF flow is 38% of cardiac output!
HOHF caused by AVF was strongly suspected!
9/12


All of these arguments favored AVF removal in this patient:
🔷 Low functional status (Wheelchair)
🔷 Significant venous congestion
🔷 Intradialytic hypotension
🔷Increased Pulmonary Vascular Resistance
🔷High Flow AVF and High CO (Also Qavf > 30% of CO)
10/12
🔷 Low functional status (Wheelchair)
🔷 Significant venous congestion
🔷 Intradialytic hypotension
🔷Increased Pulmonary Vascular Resistance
🔷High Flow AVF and High CO (Also Qavf > 30% of CO)
10/12
I Made the call to ligate AVF and place a tunneled CVC:
This fixed everything!
24 hrs after AVF ligation, there was no venous congestion, CO normalized and even RVOT Doppler became normal!
11/12



This fixed everything!
24 hrs after AVF ligation, there was no venous congestion, CO normalized and even RVOT Doppler became normal!
11/12



Despite this very interesting Doppler changes, nothing compares to the feeling when I received this text message from the patients mother:
"She is no longer using her wheelchair!"
/END
"She is no longer using her wheelchair!"
/END

Read more on High Output Heart Failure from AVF in this excellent 🧵:
https://twitter.com/aishaikh/status/1186390047689498630?s=20&t=-RBfPiF7u46F7p7P1J-dGg
• • •
Missing some Tweet in this thread? You can try to
force a refresh