1/
You’re staffing a complex patient w/ a learner on your consult team.
As they present it's clear the case was challenging for them.
They get to their assessment & take a breath.
You hit ⏸️ & say…”You know what? Let’s think through this dx together.”
What next?
This week:
You’re staffing a complex patient w/ a learner on your consult team.
As they present it's clear the case was challenging for them.
They get to their assessment & take a breath.
You hit ⏸️ & say…”You know what? Let’s think through this dx together.”
What next?
This week:
2/
Consultants are often asked to assist with diagnosis.
What do we bring to the table?
An easy answer is deeper knowledge of a specific subset of presenting problems & diseases.
Focused clinical exposure means that we develop a unique & rich library of schemas & scripts.
Consultants are often asked to assist with diagnosis.
What do we bring to the table?
An easy answer is deeper knowledge of a specific subset of presenting problems & diseases.
Focused clinical exposure means that we develop a unique & rich library of schemas & scripts.
3/
Though specialty-specific knowledge is essential to effective diagnostic reasoning for consultants, it is not enough.
Our unique 'invited' role in cases means we also need to have specific (meta)cognitive skills & habits.
Those skills/habits are part of a teachable process.
Though specialty-specific knowledge is essential to effective diagnostic reasoning for consultants, it is not enough.
Our unique 'invited' role in cases means we also need to have specific (meta)cognitive skills & habits.
Those skills/habits are part of a teachable process.
4/
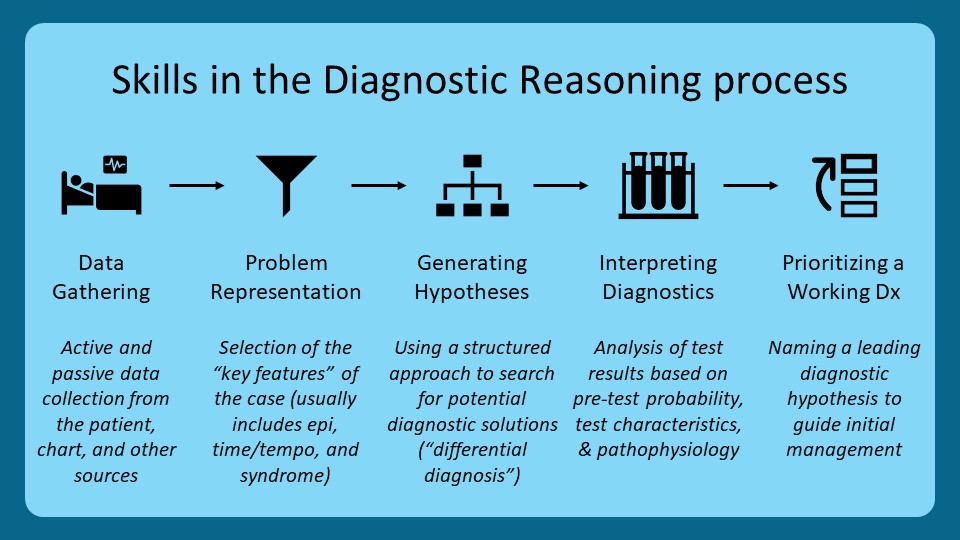
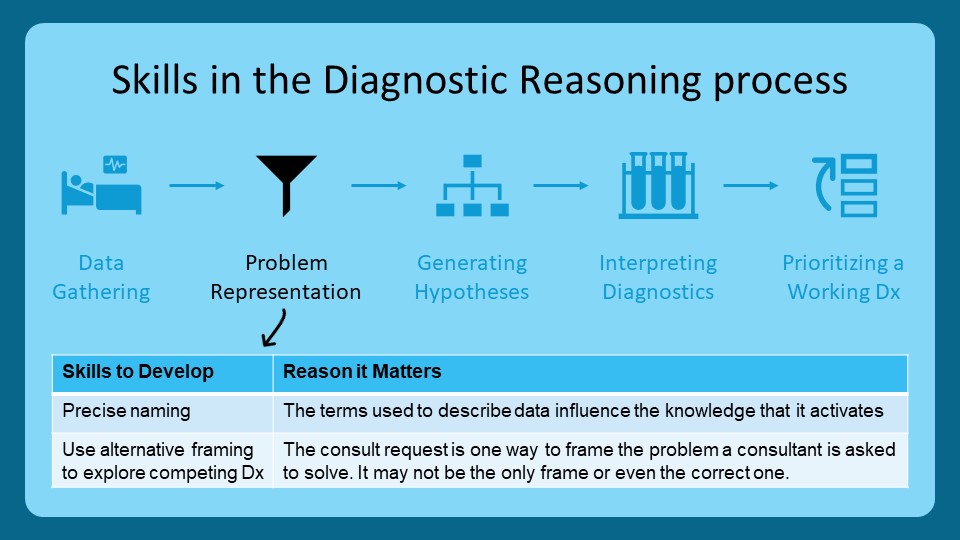
Here I’ve depicted a well-established framework for diagnostic reasoning (not specialty-specific).
We may not consciously engage in this process for every case we encounter.
But, analyzing reasoning as a process lets us identify deficiencies & teach more intentionally.
Here I’ve depicted a well-established framework for diagnostic reasoning (not specialty-specific).
We may not consciously engage in this process for every case we encounter.
But, analyzing reasoning as a process lets us identify deficiencies & teach more intentionally.
5/
Let’s now analyze some of the steps in this process w/ two specific objectives:
🎯 Identify how a consultant’s knowledge & skills at that step may be unique
🎯 Describe strategies for developing that knowledge/skill to improve diagnostic reasoning
Let’s now analyze some of the steps in this process w/ two specific objectives:
🎯 Identify how a consultant’s knowledge & skills at that step may be unique
🎯 Describe strategies for developing that knowledge/skill to improve diagnostic reasoning
6/
First: Data-gathering
Two 🗝️ consultant skills:
1⃣ Collect data targeted to your specialty & informed by specific diagnostic hypotheses
2⃣"Trust but verify" - this old dogma is actually a useful cognitive forcing strategy to deploy when receiving new consults
First: Data-gathering
Two 🗝️ consultant skills:
1⃣ Collect data targeted to your specialty & informed by specific diagnostic hypotheses
2⃣"Trust but verify" - this old dogma is actually a useful cognitive forcing strategy to deploy when receiving new consults

7/
How do we instill these habits?
@JenniferSpicer4 discussed specialty-specific frameworks to focus data-gathering in a prior thread
And I've discussed how peppering a consult requester w/ questions you will answer yourself anyway is counterproductive.
How do we instill these habits?
@JenniferSpicer4 discussed specialty-specific frameworks to focus data-gathering in a prior thread
https://twitter.com/JenniferSpicer4/status/1602704071588290561?s=20&t=IpNMTP0DPvGnkAOh30uWKA
And I've discussed how peppering a consult requester w/ questions you will answer yourself anyway is counterproductive.
8/
Next: Problem representation
This step involves distilling a case to the most diagnostically high-yield information.
Two 🗝️ skills for specialists:
1⃣ Be precise in how data are described
2⃣ Use different formulations of the problem to explore competing diagnostic pathways
Next: Problem representation
This step involves distilling a case to the most diagnostically high-yield information.
Two 🗝️ skills for specialists:
1⃣ Be precise in how data are described
2⃣ Use different formulations of the problem to explore competing diagnostic pathways
9/
Basically, it comes down to naming & framing.
The consult request is one way to formulate the diagnostic problem that needs to be solved. But other formulations may be better.
How do we develop learners to do this effectively?
🔁 By RE-framing cases & thinking “out loud”.
Basically, it comes down to naming & framing.
The consult request is one way to formulate the diagnostic problem that needs to be solved. But other formulations may be better.
How do we develop learners to do this effectively?
🔁 By RE-framing cases & thinking “out loud”.

10/
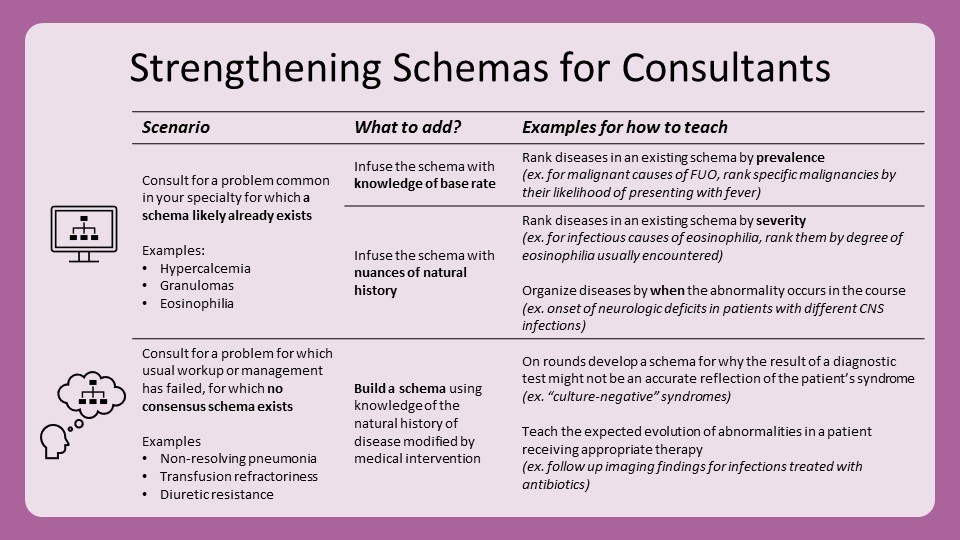
Next: Hypothesis generation
Diagnostic schemas for many subspecialty problems already exist (TY @cpsolvers!).
So, what can consultants add?
1⃣ Richer knowledge of natural history
2⃣ Schemas for problems recalcitrant to usual management
3⃣ Schemas for "endpoint diagnoses”
Next: Hypothesis generation
Diagnostic schemas for many subspecialty problems already exist (TY @cpsolvers!).
So, what can consultants add?
1⃣ Richer knowledge of natural history
2⃣ Schemas for problems recalcitrant to usual management
3⃣ Schemas for "endpoint diagnoses”
11/
How do we teach this?
For existing schemas, we can add nuance w/ knowledge of base rate & natural history (e.g., how is this disease supposed to present?)
For cases where ‘usual care’ hasn't worked, we can create schemas using experiential wisdom about how things go wrong.
How do we teach this?
For existing schemas, we can add nuance w/ knowledge of base rate & natural history (e.g., how is this disease supposed to present?)
For cases where ‘usual care’ hasn't worked, we can create schemas using experiential wisdom about how things go wrong.
12/
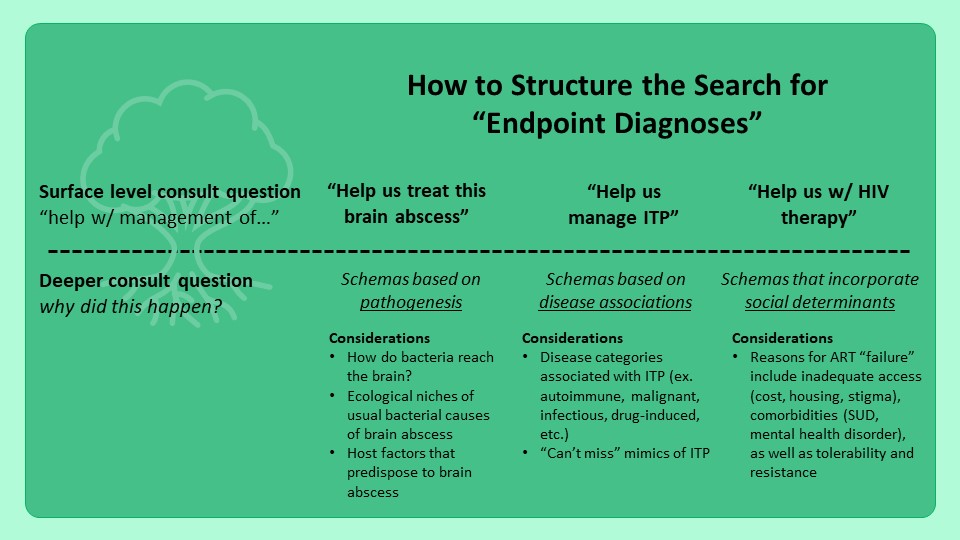
One more point: Consultants are often asked to help manage a differentiated (read: diagnosed) problem.
But that problem may not be an “endpoint diagnosis” (see pubmed.ncbi.nlm.nih.gov/35942949/).
We thus need to teach schemas that explore etiologic explanations for common problems!
One more point: Consultants are often asked to help manage a differentiated (read: diagnosed) problem.
But that problem may not be an “endpoint diagnosis” (see pubmed.ncbi.nlm.nih.gov/35942949/).
We thus need to teach schemas that explore etiologic explanations for common problems!
13/
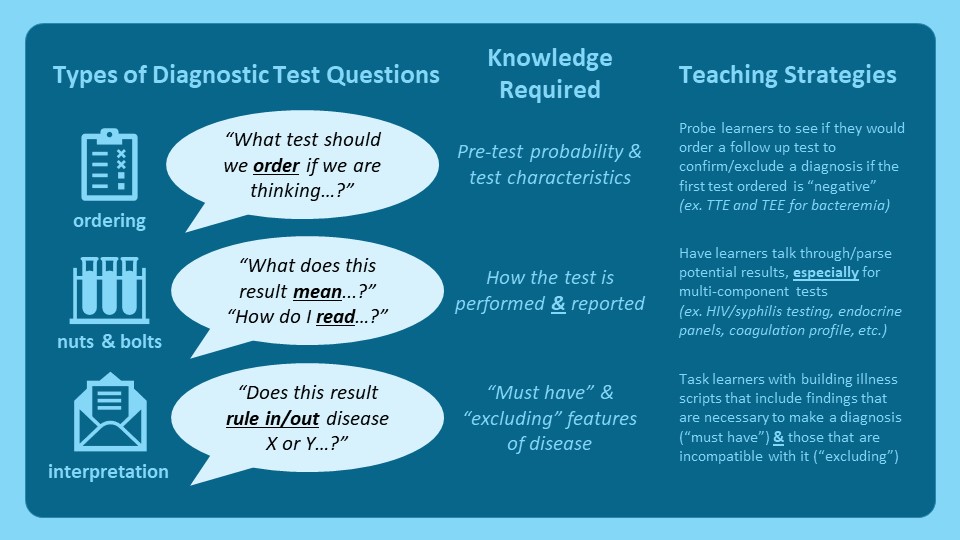
Next: Test interpretation
Consults are often prompted by obscure or equivocal test results.
Reasoning skills we can develop here:
1⃣ How to parse complex results (ex. flow cytometry, discordant HIV Ab/PCR, etc.)
2⃣ Estimating pre/post-test probability
Next: Test interpretation
Consults are often prompted by obscure or equivocal test results.
Reasoning skills we can develop here:
1⃣ How to parse complex results (ex. flow cytometry, discordant HIV Ab/PCR, etc.)
2⃣ Estimating pre/post-test probability
14/
To build this skill, our teaching should derive from the kinds of questions we get.
All these strategies use hypothetical scenarios to:
🤔 Probe how learners are prioritizing diagnoses
🔁 Create opportunities for deliberate practice
📚 Augment disease/management scripts
To build this skill, our teaching should derive from the kinds of questions we get.
All these strategies use hypothetical scenarios to:
🤔 Probe how learners are prioritizing diagnoses
🔁 Create opportunities for deliberate practice
📚 Augment disease/management scripts
15/
Finally: Working Dx
Consultants often add value just by clarifying the active problem(s).
Specialty learners need to learn to formulate their working Dx to help teams:
1⃣ Synthesize & prioritize
2⃣ Halt diagnostic/therapeutic momentum
3⃣ Capture the level of uncertainty
Finally: Working Dx
Consultants often add value just by clarifying the active problem(s).
Specialty learners need to learn to formulate their working Dx to help teams:
1⃣ Synthesize & prioritize
2⃣ Halt diagnostic/therapeutic momentum
3⃣ Capture the level of uncertainty
16/
How can we teach this?
Notes are an effective medium to model these skills & @JenniferSpicer4 shared one framework:
Re-phrasing the assessment concisely conveys the working dx as you (the teacher) are formulating it.
Some ID examples to illustrate:
How can we teach this?
Notes are an effective medium to model these skills & @JenniferSpicer4 shared one framework:
https://twitter.com/JenniferSpicer4/status/1612864363068624928?s=20&t=JIVHFksXcQMK5TXwpv4_1w
Re-phrasing the assessment concisely conveys the working dx as you (the teacher) are formulating it.
Some ID examples to illustrate:

17/
Let’s recap:
In this 🧵 we:
📌 Dissected the diagnostic reasoning process & explored unique considerations for specialists.
📌 Identified elements that require intentional development of specific knowledge/skills/habits.
📌 Summarized teaching strategies to build them!
Let’s recap:
In this 🧵 we:
📌 Dissected the diagnostic reasoning process & explored unique considerations for specialists.
📌 Identified elements that require intentional development of specific knowledge/skills/habits.
📌 Summarized teaching strategies to build them!

18/
Next week I will continue this series on “Teaching the Consult Team” w/ “Management Reasoning.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam & follow @YihanYangMD @GStetsonMD @ChrisDJacksonMD to keep up with all our threads!
See you next week!
Next week I will continue this series on “Teaching the Consult Team” w/ “Management Reasoning.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam & follow @YihanYangMD @GStetsonMD @ChrisDJacksonMD to keep up with all our threads!
See you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh