1/Do you know all the aspects of, well, ASPECTS?
Many know the anterior circulation #stroke scoring system—but posterior circulation (pc) ASPECTS is often unknown
Here’s a #tweetorial to help you remember pc-ASPECTS
#medtwitter #neurotwitter #meded #neurorad #neurology #FOAMed
Many know the anterior circulation #stroke scoring system—but posterior circulation (pc) ASPECTS is often unknown
Here’s a #tweetorial to help you remember pc-ASPECTS
#medtwitter #neurotwitter #meded #neurorad #neurology #FOAMed
2/Many know anterior circulation ASPECTS. It uses a 10 point scoring system to semi-quantitate the amount of the MCA territory infarcted on non-contrast head CT.
If you need a review: here’s my tweetorial on ASPECTS:
If you need a review: here’s my tweetorial on ASPECTS:
https://twitter.com/teachplaygrub/status/1587472264764657664
3/But it’s only useful for the anterior circulation. Posterior circulation accounts for ~25% of infarcts. Even w/recanalization, many of these pts do poorly bc of the extent of already infarcted tissue. So there’s a need to quantitate the amount of infarcted tissue in these pts 

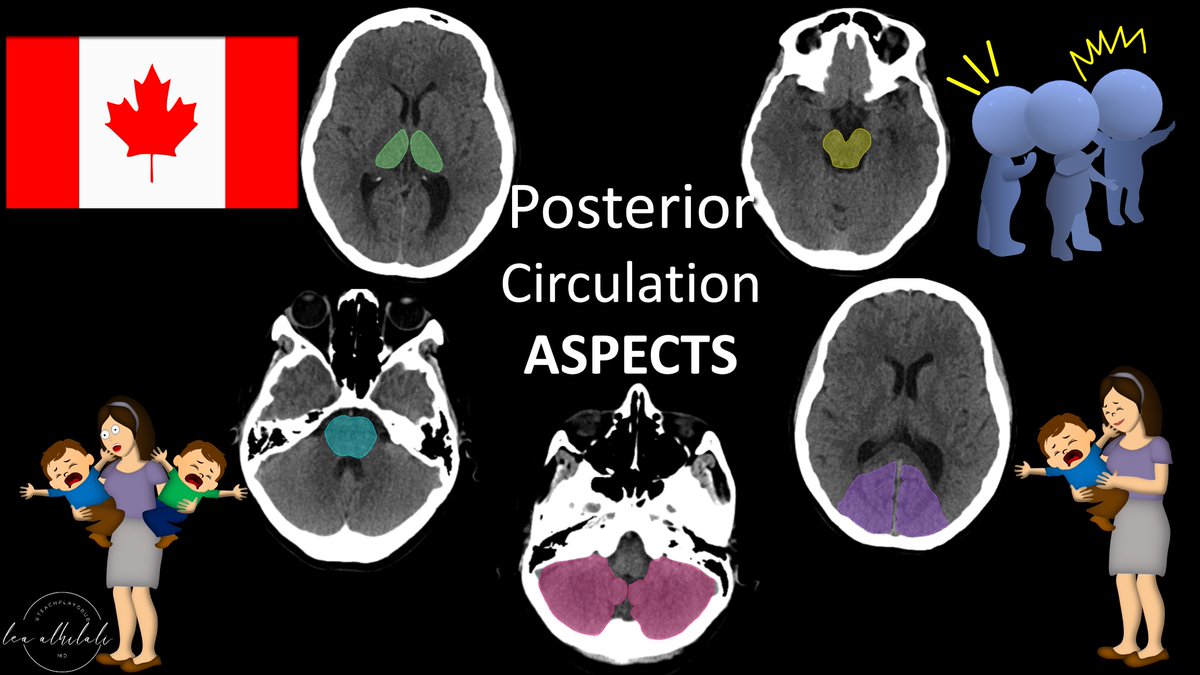
4/Posterior circulation ASPECTS, or pc-ASPECTS for short, is also a 10 point system—but for the vertebrobasilar circulation. Patients get points for each region NOT infarcted on the initial CT. 

5/Similar to anterior ASPECTS, points are GOOD
It’s like a city—when a region infarcts, it is like the lights go out in that city region (literally, tissue darkens on CT)
In ant & post ASPECTS, you are counting the regions where the lights are still on—so high ASPECTS is good
It’s like a city—when a region infarcts, it is like the lights go out in that city region (literally, tissue darkens on CT)
In ant & post ASPECTS, you are counting the regions where the lights are still on—so high ASPECTS is good

6/Which regions get scored?
The biggest prognostic factors in posterior strokes are time & amount of already infarcted tissue.
So my mnemonic to remember pc-ASPECTS regions is:
Time & Mortal Brain decide Posterior Circulation Outcomes
(mortal brain= infarcted brain)
The biggest prognostic factors in posterior strokes are time & amount of already infarcted tissue.
So my mnemonic to remember pc-ASPECTS regions is:
Time & Mortal Brain decide Posterior Circulation Outcomes
(mortal brain= infarcted brain)

7/How do you assign points?
It’s a little different than anterior ASPECTS, where every region just got one point
For pc-ASPECTS, think of it like a mother. She only has 2 arms. So if there are two kids, they have to split the arms—only one arm can be wrapped around each kid
It’s a little different than anterior ASPECTS, where every region just got one point
For pc-ASPECTS, think of it like a mother. She only has 2 arms. So if there are two kids, they have to split the arms—only one arm can be wrapped around each kid

8/So unpaired structures, like the brainstem, are like having only one kid—you get both arms wrapped around you = 2 arms = 2 points.
If the structures are paired, like the cerebellum, it’s like having two kids--they must split the arms. Each gets only 1 arm = 1 point
If the structures are paired, like the cerebellum, it’s like having two kids--they must split the arms. Each gets only 1 arm = 1 point

9/So lets go through our regions using the mnemonic.
Each thalmus is worth only 1 point, bc they’re paired & have to share their mother’s arms.
The unpaired midbrain is worth 2 points (gets both arms)
Each thalmus is worth only 1 point, bc they’re paired & have to share their mother’s arms.
The unpaired midbrain is worth 2 points (gets both arms)

10/Pons is unpaired, so it is worth 2 points.
But the paired cerebellar hemispheres & occipital cortex are each only worth 1 point per side, as each side claims only one of the mother’s arms
But the paired cerebellar hemispheres & occipital cortex are each only worth 1 point per side, as each side claims only one of the mother’s arms

11/While there’s evidence that higher pc-ASPECTS means poorer outcome, there’s no consensus about what pc-ASPECTS score definitively confers a UFO (unfavorable outcome).
But the consensus about what confers a UFO in anterior circulation ASPECTS may change soon as well!
But the consensus about what confers a UFO in anterior circulation ASPECTS may change soon as well!

12/So now you know the regions & scoring for pc-ASPECTS!
Remember, the anterior circulation isn’t the only aspect of ASPECTS!
Remember, the anterior circulation isn’t the only aspect of ASPECTS!

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















