1/ You're finally settled in as an attending and you get a new patient.
They sound brain brain dead.
They clinically look brain dead.
Your team asks if they're brain dead.
Well this turned serious… a quick #tweetorial about 🧠 death
#NeuroTwitter #Neurocrit #MedTwitter
They sound brain brain dead.
They clinically look brain dead.
Your team asks if they're brain dead.
Well this turned serious… a quick #tweetorial about 🧠 death
#NeuroTwitter #Neurocrit #MedTwitter
2/ The transfer 📞 you got was a 28 yo with no other history. They were concerned about her being in status epilepticus.
You turn off all sedation. They're still unresponsive.
You turn off all sedation. They're still unresponsive.
3/ Clinically, they're intubated and have fixed and dilated 👀. No corneal or cough and not breathing over the vent. No motor response w/ painful stimuli 🤕
You scan their labs - ✅ no significant abnormalities You check their vitals - ✅ looks all good
What should we do next?
You scan their labs - ✅ no significant abnormalities You check their vitals - ✅ looks all good
What should we do next?
5/ No seizures on continuous EEG. With weaning sedation, you notice some myoclonic movements (MM). A medical student asks if it's time for brain death testing.
What do you tell your team?
What do you tell your team?
6/ Remembering there's a guideline, we quickly pull it up. AAN requires specific prerequisites before 🧠 death testing
1) Coma, irreversible and cause known
2) Neuroimaging explains coma
3) CNS depressant drug effect absent
4) sBP >100 mmHg
5) No spontaneous breathing
1) Coma, irreversible and cause known
2) Neuroimaging explains coma
3) CNS depressant drug effect absent
4) sBP >100 mmHg
5) No spontaneous breathing
7/ So going back to our patient, let’s ask again.
Now that we've looked at the prerequisites, what do you tell your team?
Now that we've looked at the prerequisites, what do you tell your team?
8/ If you chose C both times, you are correct! Our patient does not qualify for a brain death testing.
1) Coma, irreversible and cause known ❌
2) Neuroimaging explains coma ❌
3) CNS depressant drug effect absent ❓
4) sBP >100 mmHg ✅
5) No spontaneous breathing ✅
1) Coma, irreversible and cause known ❌
2) Neuroimaging explains coma ❌
3) CNS depressant drug effect absent ❓
4) sBP >100 mmHg ✅
5) No spontaneous breathing ✅
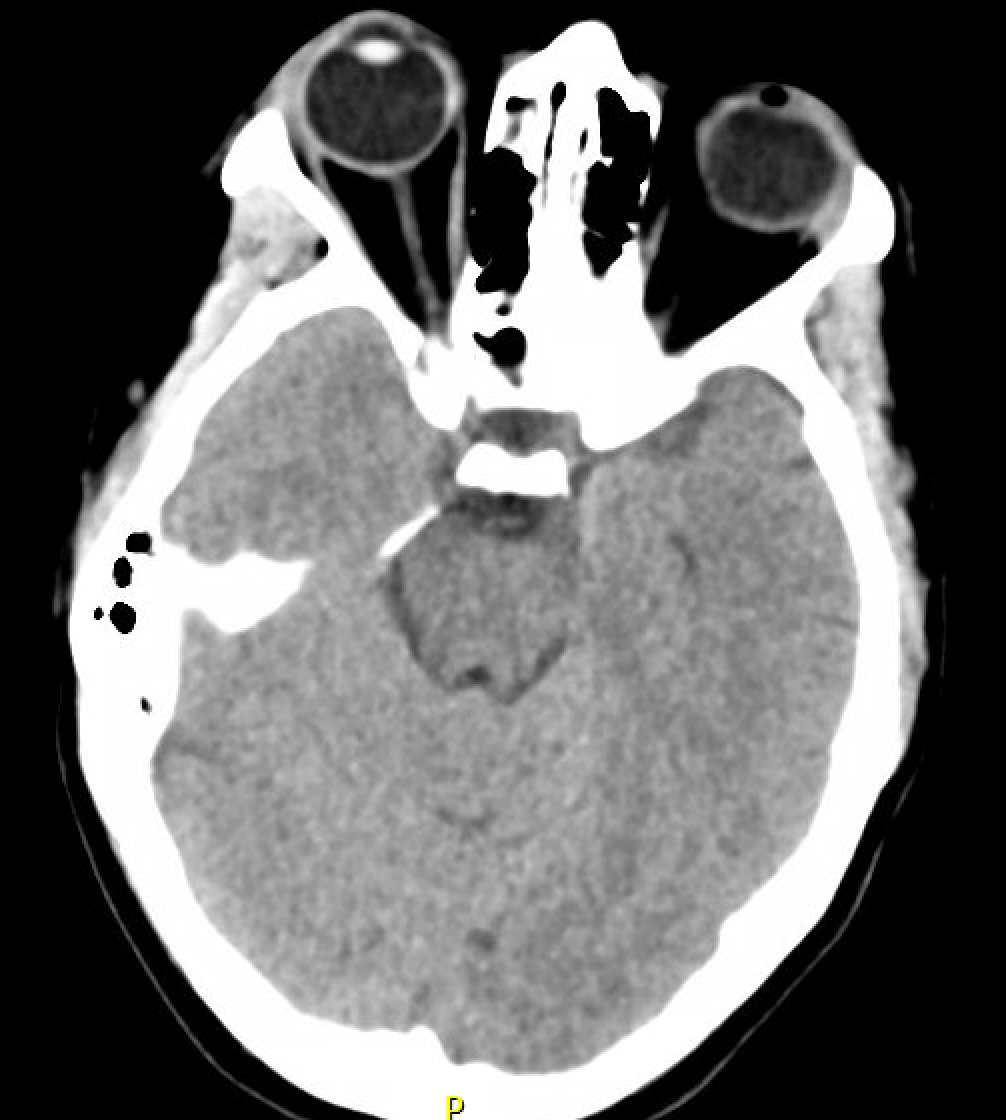
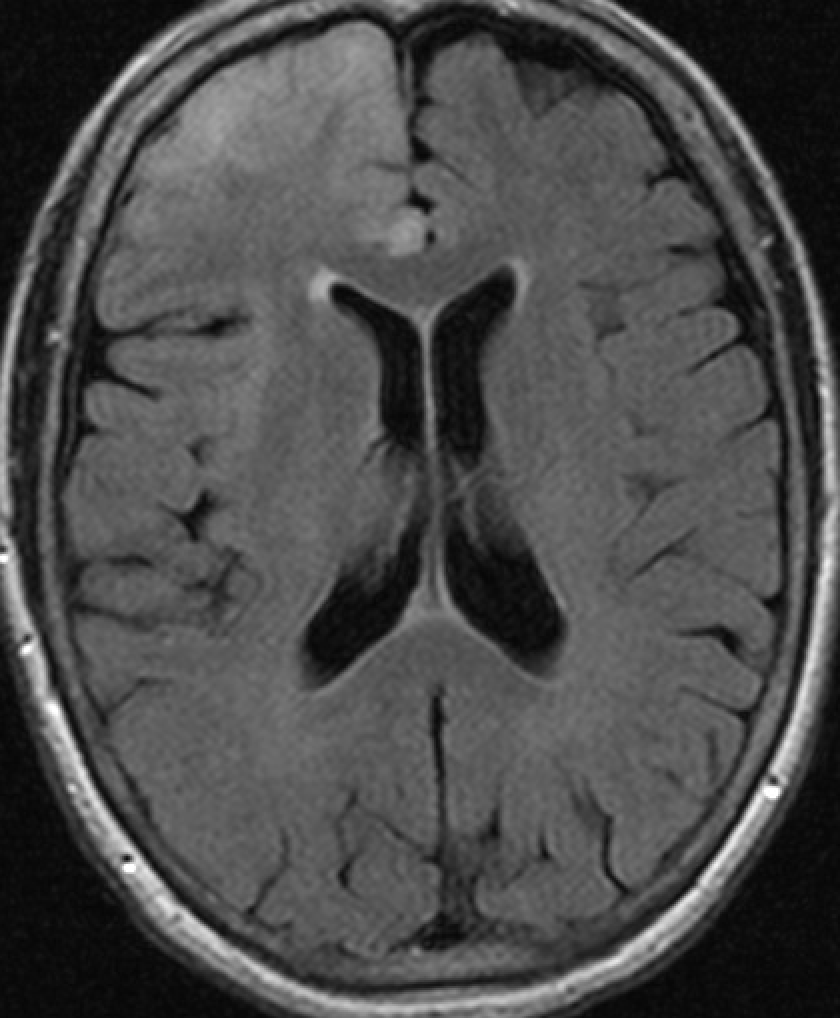
9/ We don't have any irreversible causes known, nor do we have any radiographic evidence for her coma (ie anoxia or ICH). In fact, her CTH looks normal!
And while we can assume her sedation was held long enough, we don't know about other drugs effects.
Her UDS is shown below
And while we can assume her sedation was held long enough, we don't know about other drugs effects.
Her UDS is shown below

10/ While some additional information was withheld at the start, this is an important reminder that just because someone looks “brain dead” doesn’t mean they’re actually brain dead.
Here's a good overview of brain death criteria
ncbi.nlm.nih.gov/books/NBK54514…
Here's a good overview of brain death criteria
ncbi.nlm.nih.gov/books/NBK54514…
11/ Another thing to remember is 🧠 death testing varies throughout the world.
Published in Jama 2020, Greer et al does a great job providing recommendations for the minimum clinical standard for determining 🧠 death (w/ hopes of a greater consistency within and b/t countries)
Published in Jama 2020, Greer et al does a great job providing recommendations for the minimum clinical standard for determining 🧠 death (w/ hopes of a greater consistency within and b/t countries)

12/ Courtesy of @rkchoi, here's another interesting article about #BrainDeath by Truog from JAMA 2023
https://twitter.com/rkchoi/status/1623405976475795459
13/ In general, before I even consider doing a brain death testing, I always ask myself the following question
"Do we have evidence of a catastrophic and irreversible CNS injury?"
"Do we have evidence of a catastrophic and irreversible CNS injury?"
14/ If the answer is no, I stop right there. No need for anything else, we don't go down the brain death route.
In my opinion, this is the one test that we need to be absolutely 100% certain. Being wrong even 1% of the time can lead to devastating consequences.
In my opinion, this is the one test that we need to be absolutely 100% certain. Being wrong even 1% of the time can lead to devastating consequences.
15/ While actual 🧠 death testing is saved for another #tweetorial, a few pearls that I've encountered
- Brain death mimickers; locked in syndrome, paralytics, hypothermia, drugs OD, among many others
- Use meds/equipments to meet prerequisites (ie pressors, bair hugger etc)
- Brain death mimickers; locked in syndrome, paralytics, hypothermia, drugs OD, among many others
- Use meds/equipments to meet prerequisites (ie pressors, bair hugger etc)
16/ Another important tip (taught to me by @Capt_Ammonia) I've used a few times on consults
- In intubated pts who are 🧠 dead, the flow trigger can make it look like there’s “spontaneous breathing." This can solved by changing the threshold or flipping to a pressure trigger
- In intubated pts who are 🧠 dead, the flow trigger can make it look like there’s “spontaneous breathing." This can solved by changing the threshold or flipping to a pressure trigger
17/ So going back to our pt, we actually found out she ODed on bupropion.
If you were thinking ahead, yes she was diagnosed w/ serotonin syndrome given her myoclonus and dilated pupils (she also ODed on a few other drugs making her exam different than the the classic one)
If you were thinking ahead, yes she was diagnosed w/ serotonin syndrome given her myoclonus and dilated pupils (she also ODed on a few other drugs making her exam different than the the classic one)
18/ Supportive care is the key for these patients. She was started on a Versed gtt for ~24-48 hours before being slowly weaned off. She was ultimately extubated without any neurologic deficit.
19) Any other thoughts/wisdom?
@KateOConnellDO @GangaNavada @JayKinariwala @maness_caroline @EricLawson90 @caseyalbin @sigman_md @CajalButterfly @rkchoi @Capt_Ammonia @NeyensRon @theABofPharmaC @katskript @pouyeah @snelgrove_dan @chalela1 @cmandrewsmd @namorrismd @radomingoc
@KateOConnellDO @GangaNavada @JayKinariwala @maness_caroline @EricLawson90 @caseyalbin @sigman_md @CajalButterfly @rkchoi @Capt_Ammonia @NeyensRon @theABofPharmaC @katskript @pouyeah @snelgrove_dan @chalela1 @cmandrewsmd @namorrismd @radomingoc
@MuscNeurology @MUSCNeuroICU @HolyCityNsgy
@EmoryNeuroCrit @EmoryNeurology @PennNeurology
@upmcneuro @NeurocriticalE @NaomiNiznick @omarshahmd @MBowerMD @SubinMatthews @GhadaMohamedMD
@EmoryNeuroCrit @EmoryNeurology @PennNeurology
@upmcneuro @NeurocriticalE @NaomiNiznick @omarshahmd @MBowerMD @SubinMatthews @GhadaMohamedMD
• • •
Missing some Tweet in this thread? You can try to
force a refresh