HV Doppler from a pt with severe group 1 pulmonary hypertension 👇
Many of us don't have ECG when doing POCUS...
Is it posible to determine this waveform components?
The answer is yes! I'll show you how I did it here
A 🧵on HV Doppler in Pulmonary Hypertension
#VExUS 1/12
Many of us don't have ECG when doing POCUS...
Is it posible to determine this waveform components?
The answer is yes! I'll show you how I did it here
A 🧵on HV Doppler in Pulmonary Hypertension
#VExUS 1/12

Normal HV is a mirror image of normal CVP waveform.
It usually has 4 waves:
2 antegrade (flow from liver to 🫀) waves (S and D)
2 retrograde (flow from 🫀 to liver) waves (A and V)
2/12

It usually has 4 waves:
2 antegrade (flow from liver to 🫀) waves (S and D)
2 retrograde (flow from 🫀 to liver) waves (A and V)
2/12


A frequent alteration in pts w severe PH is Severe Tricuspid Regurgitation
In severe TR, there is retrograde flow from the RV to the RA in systole. If the right atrium is not compliant, this flow reaches the HV and gives a reverse S wave!
Example from another case 👇
3/12
In severe TR, there is retrograde flow from the RV to the RA in systole. If the right atrium is not compliant, this flow reaches the HV and gives a reverse S wave!
Example from another case 👇
3/12

Even without EKG, when scanning the kidneys we can take advantage of the fact that the venules run parallel to arterioles!
This tells us where systole and diastole are!
Applying this to the case in tweet #2, it is clear that there is S wave reversal!
4/12

This tells us where systole and diastole are!
Applying this to the case in tweet #2, it is clear that there is S wave reversal!
4/12


Back to our initial case...
As mentioned in the 1st tweet, this patient has severe PAH
In fact, there is severe TR in this case, so S reversal is a good guess!
5/12

As mentioned in the 1st tweet, this patient has severe PAH
In fact, there is severe TR in this case, so S reversal is a good guess!
5/12


However, when we scan of HV and Intra-renal vein at the same time we get this👇!
Intra-renal doppler suggests that the antegrade wave is an S wave!
This means the large retrograde wave must be an A wave!
Understanding why this happens requires knowledge 📚...
6/12


Intra-renal doppler suggests that the antegrade wave is an S wave!
This means the large retrograde wave must be an A wave!
Understanding why this happens requires knowledge 📚...
6/12



Did't we say there was severe TR in this case? There is severe TR!
But there is also a HUGE RA that can accommodate all systolic retrograde flow!
Antegrade S wave is due to atrial relaxation in this case
OK, but where is the D wave?
7/12
But there is also a HUGE RA that can accommodate all systolic retrograde flow!
Antegrade S wave is due to atrial relaxation in this case
OK, but where is the D wave?
7/12

Severe PAH leads to RV Hypertrophy and impaired relaxation. This leads to a delay in TV valve opening and can lead to an absent D wave!
Also RVH leads to ⬆️ RVEDP causing large A waves!
8/12

Also RVH leads to ⬆️ RVEDP causing large A waves!
8/12


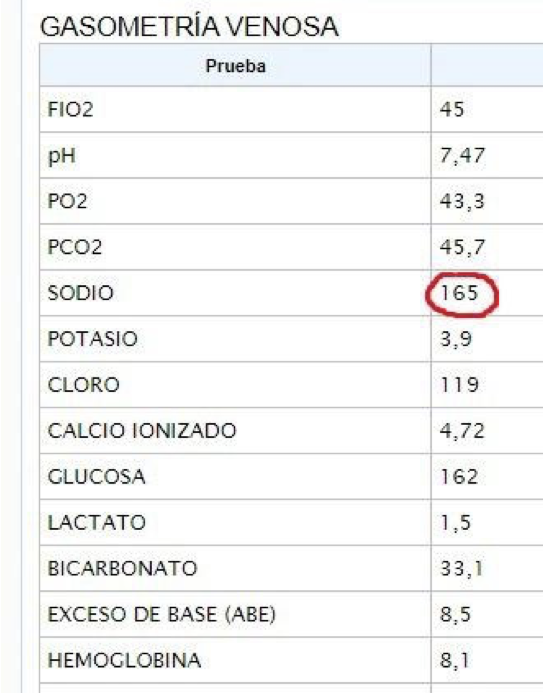
So if we are right then this patient must have severe PAH with severe RVH..
EKG and Tricuspid Regurgitation Velocity confirms this!
(TRV lets us estimate pulmonary artery pressure, here it is higher than 110 mmHg!!)
So, the correct labeling of waves is this one:
9/12


EKG and Tricuspid Regurgitation Velocity confirms this!
(TRV lets us estimate pulmonary artery pressure, here it is higher than 110 mmHg!!)
So, the correct labeling of waves is this one:
9/12



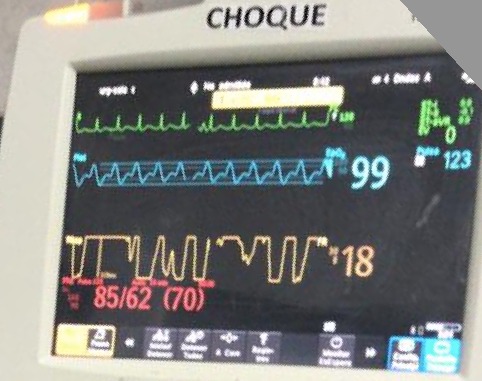
I initially saw this patient in the ED, then got admitted to the ICU...
After a few hours I re-scanned the pt. Heart rate had improved and I was NOW able to see the D wave!
Severe TR was still there, but again, definitely NO "S" reversal!
10/12
After a few hours I re-scanned the pt. Heart rate had improved and I was NOW able to see the D wave!
Severe TR was still there, but again, definitely NO "S" reversal!
10/12

Invasive CVP waveform allowed me to confirm that there was no S reversal and there was Blunted D wave ("y descent") with respiration!
Also, I enjoyed looking at how uncannily similar CVP waveform and HV waveform were!! 🤯
11/12

Also, I enjoyed looking at how uncannily similar CVP waveform and HV waveform were!! 🤯
11/12


Conclusions:
HV changes in severe PAH are:
In patients without severe TR or with good RA compliance:
🔷 Increased RVEDP: Large A waves
🔷 Delayed TV opening: Absent D wave
🚨 If patient has severe TR with non-compliat RA
🔷 S wave reversal (with reappearance of D wave)
/END
HV changes in severe PAH are:
In patients without severe TR or with good RA compliance:
🔷 Increased RVEDP: Large A waves
🔷 Delayed TV opening: Absent D wave
🚨 If patient has severe TR with non-compliat RA
🔷 S wave reversal (with reappearance of D wave)
/END

• • •
Missing some Tweet in this thread? You can try to
force a refresh