
Every organization will encounter a crisis.
Here’s how we used the concept of pre-mortem to improve.
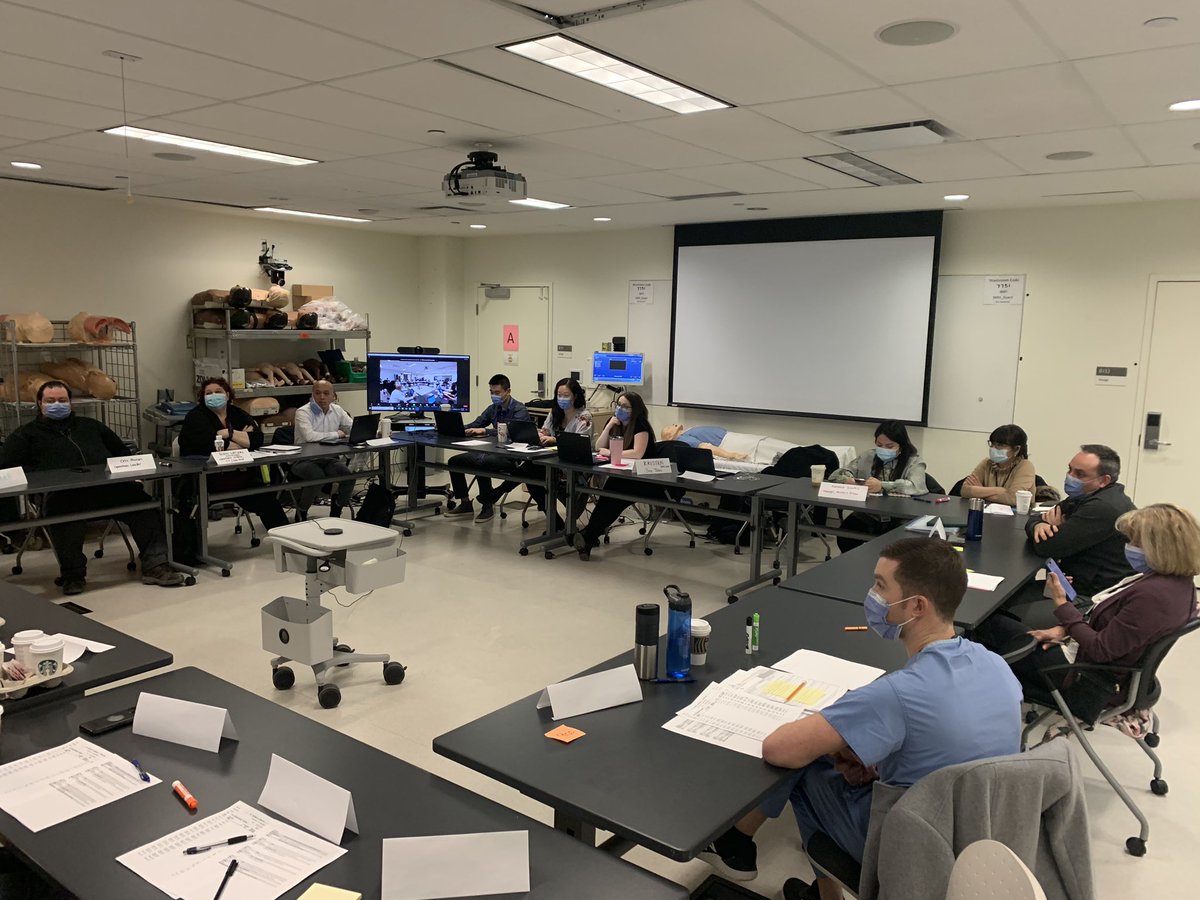
This week we @Sim_UnityHealth conducted a multi-disciplinary #simulation of a complete loss of IT infrastructure.
Goal: crash test our processes & ensure ongoing care
🧵
1/
Here’s how we used the concept of pre-mortem to improve.
This week we @Sim_UnityHealth conducted a multi-disciplinary #simulation of a complete loss of IT infrastructure.
Goal: crash test our processes & ensure ongoing care
🧵
1/
Frequently organizations develop policies for crises but we know that work as imagined is never the same as work as done. @StevenShorrock
Orgs guess how ppl respond.
They hope ppl will remember the procedures.
They 🤞 that the system under stress will work.
2/
Orgs guess how ppl respond.
They hope ppl will remember the procedures.
They 🤞 that the system under stress will work.
2/
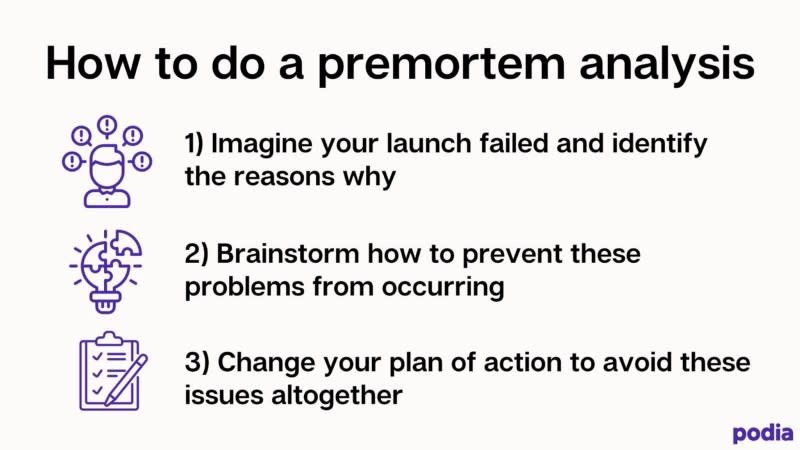
But there’s a better way to know with greater certainty how the system and people will respond. And what strengths and deficiencies exist.
We use #simulation to support a pre-mortem.
3/
We use #simulation to support a pre-mortem.
3/
We ran a #simulation of a complete loss of IT infrastructure and had our participants (front line clinicians) work thru the challenges.
We observed what processes they used successfully and what proved challenging.
4/
We observed what processes they used successfully and what proved challenging.
4/
Rather than guessing and hoping, we observed actual clinicians respond in real time - bridging the gap between work as imagined and work as done.
Then we debriefed and gained valuable perspectives from the end users.
The engagement among staff was amazing!
5/
Then we debriefed and gained valuable perspectives from the end users.
The engagement among staff was amazing!
5/
Our emergency management team takes these insights to update our system so that should this happen IRL we’ll have a closed gaps and be better prepared.
This is just another form of #simulation-informed design.
This is key part of a learning organization.
End
This is just another form of #simulation-informed design.
This is key part of a learning organization.
End
• • •
Missing some Tweet in this thread? You can try to
force a refresh














