1/
#ContinuumCase
A 67 yo man with a known, active cancer presents to the ED. His wife reports that he has had worsening headaches, forgetfulness, & confusion. Today, he was increasingly sleepy which triggered the presentation.
An MRI is ordered.
🤔🤔🤔 @ContinuumAAN @LyellJ
#ContinuumCase
A 67 yo man with a known, active cancer presents to the ED. His wife reports that he has had worsening headaches, forgetfulness, & confusion. Today, he was increasingly sleepy which triggered the presentation.
An MRI is ordered.
🤔🤔🤔 @ContinuumAAN @LyellJ

2/
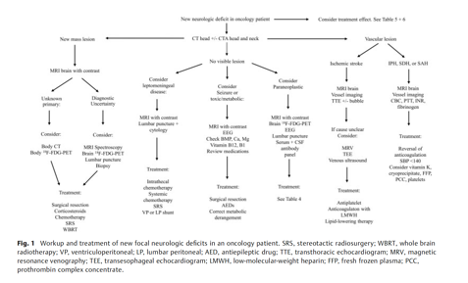
Neurologic complications in cancer patients are tricky. They can be due to
✨Malignant lesions
✨Systemic complications of disease
✨Paraneoplastic disorders
✨Treatment Side effects
Neurologic complications in cancer patients are tricky. They can be due to
✨Malignant lesions
✨Systemic complications of disease
✨Paraneoplastic disorders
✨Treatment Side effects
3/
You absolutely must have a systemic approach to these patients. I think the best framework for this is in this review by @holroyd_katie, Dan Rubin and Henrikas Vaitkevicius:
pubmed.ncbi.nlm.nih.gov/34619783/
You absolutely must have a systemic approach to these patients. I think the best framework for this is in this review by @holroyd_katie, Dan Rubin and Henrikas Vaitkevicius:
pubmed.ncbi.nlm.nih.gov/34619783/
4/
Reviewing his cancer treatment history which do you find?
Reviewing his cancer treatment history which do you find?
5/
Cancer treatments can cause a wide variety of PNS/CNS complications ranging from Myasthenia Gravis to PML. This review is an excellent overview of some of the CNS complications of various anti-cancer treatments: insightsimaging.springeropen.com/articles/10.11…
Awesome table:
Cancer treatments can cause a wide variety of PNS/CNS complications ranging from Myasthenia Gravis to PML. This review is an excellent overview of some of the CNS complications of various anti-cancer treatments: insightsimaging.springeropen.com/articles/10.11…
Awesome table:

6/
Briefly, Rituximab may cause PRES and very, very rarely result in reactivation of JC Virus and cause PML.
pubmed.ncbi.nlm.nih.gov/25489887/
Briefly, Rituximab may cause PRES and very, very rarely result in reactivation of JC Virus and cause PML.
pubmed.ncbi.nlm.nih.gov/25489887/

7/
Methotrexate is known to cause a diffuse acute or chronic leukoencephalopathy.
The acute presentation is often hours after treatment and presents with confusion and seizures.
Chronic confusion and worsening aphasia may also occur. See radiopaedia:
radiopaedia.org/articles/metho…
Methotrexate is known to cause a diffuse acute or chronic leukoencephalopathy.
The acute presentation is often hours after treatment and presents with confusion and seizures.
Chronic confusion and worsening aphasia may also occur. See radiopaedia:
radiopaedia.org/articles/metho…

8/
Treatment for this includes rescue leucovorin, dextromethorphan and aminophylline.
Treatment for this includes rescue leucovorin, dextromethorphan and aminophylline.
9/
CAR T-cells can have a whole host of systemic complications and I am eagerly awaiting @pulmcrit’s chapter on @emcrit / @iBookCC
Generally, the most feared complication of this is diffuse cerebral edema.
A nice “practical” review: pubmed.ncbi.nlm.nih.gov/32503897/
CAR T-cells can have a whole host of systemic complications and I am eagerly awaiting @pulmcrit’s chapter on @emcrit / @iBookCC
Generally, the most feared complication of this is diffuse cerebral edema.
A nice “practical” review: pubmed.ncbi.nlm.nih.gov/32503897/
10/
But, the lesion in this case?
Due to nivolumab!
Immune checkpoint inhibitors (ipilimumab, nivolumab ad prembrolizumab) may have a range of PNS/CNS adverse events.
One feature that is unique to ICIs is inducing a subcortical immune-mediated encephalitis👇
But, the lesion in this case?
Due to nivolumab!
Immune checkpoint inhibitors (ipilimumab, nivolumab ad prembrolizumab) may have a range of PNS/CNS adverse events.
One feature that is unique to ICIs is inducing a subcortical immune-mediated encephalitis👇

11/
Encephalitis typically falls into two categories for these patients:
📍focal encephalitis, which can include limbic encephalitis
🧠meningoencephalitis (presents with fever, headache, and inflammatory CSF).
Rarely ICIs can cause hypophysitis (particularly ipilimumab).
Encephalitis typically falls into two categories for these patients:
📍focal encephalitis, which can include limbic encephalitis
🧠meningoencephalitis (presents with fever, headache, and inflammatory CSF).
Rarely ICIs can cause hypophysitis (particularly ipilimumab).
12/
It is hypothesized that the focal encephalitis may be an unmasking of a previously occult paraneoplastic encephalitis when the patient is exposed to the ICI. These cases are associated with a significantly worse prognosis.
More here:
pubmed.ncbi.nlm.nih.gov/33720308/
It is hypothesized that the focal encephalitis may be an unmasking of a previously occult paraneoplastic encephalitis when the patient is exposed to the ICI. These cases are associated with a significantly worse prognosis.
More here:
pubmed.ncbi.nlm.nih.gov/33720308/
13/
Really not much is known about how to treat these patients. Usually the treatment is withholding the ICI and administering corticosteroids...other induction immunosuppression has also been tried.
Really not much is known about how to treat these patients. Usually the treatment is withholding the ICI and administering corticosteroids...other induction immunosuppression has also been tried.
14/
Recap, when approaching neurologic complications in cancer patients, think
♋️cancer itself?
💊 treatment side effect?
🦀paraneoplastic phenomenon?
Neuroradiology can be very helpful in addition to the time course and localization.
Recap, when approaching neurologic complications in cancer patients, think
♋️cancer itself?
💊 treatment side effect?
🦀paraneoplastic phenomenon?
Neuroradiology can be very helpful in addition to the time course and localization.
15/ To check out more awesome ways in which imaging offers a window into autoimmune, paraneoplastic, and neuro-rheumatologic brain pathology, this is a fantastic review by @Lamaaw27 and TCho @ContinuumAAN
journals.lww.com/continuum/Full…
journals.lww.com/continuum/Full…
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter








