ADHF with overload is the most common cause of admission in the United States.
Confident diuresis is a skill set all IM interns must master.
Follow these tips to take your inpatient diuresis to the next level!
~ Diuretics 201: A Thread ~
#tipsfornewdocs #MedEd
1/18
Confident diuresis is a skill set all IM interns must master.
Follow these tips to take your inpatient diuresis to the next level!
~ Diuretics 201: A Thread ~
#tipsfornewdocs #MedEd
1/18

Check out the @pointofcaremed podcast episode on this topic.
spotifyanchor-web.app.link/e/hJ1tDQYEDzb
Here's a TL;DR for the episode
2/18
spotifyanchor-web.app.link/e/hJ1tDQYEDzb
Here's a TL;DR for the episode
2/18
When Admitting:
Immediate strict I/O's
Double the patient's home dose of loop diuretic (maybe more in CKD)
Find out if the patient put out well after the first dose in the ED (might not have the best I/O data)
Continue spironolactone if home med (to prevent hypokalemia)
3/18
Immediate strict I/O's
Double the patient's home dose of loop diuretic (maybe more in CKD)
Find out if the patient put out well after the first dose in the ED (might not have the best I/O data)
Continue spironolactone if home med (to prevent hypokalemia)
3/18
Following Up After Bolusing:
Assess response in 1 hour - if adequate, patient will know
If not peeing, make sure you aren't missing shock or obstruction
If peeing, check output in 3-4 hours in early afternoon - redose if not halfway to goal output
4/18
Assess response in 1 hour - if adequate, patient will know
If not peeing, make sure you aren't missing shock or obstruction
If peeing, check output in 3-4 hours in early afternoon - redose if not halfway to goal output
4/18
Yes, Lasix "lasts six hours", but you shouldn't wait that long to check on the output.
Pro Tip(s) - give the first bolus in the AM before rounds and don't leave diuresis decisions to the night team if you can avoid it!
5/18
Pro Tip(s) - give the first bolus in the AM before rounds and don't leave diuresis decisions to the night team if you can avoid it!
5/18
Troubleshooting Resistance - if 80-160mg IV lasix BID, consider:
- Switching to drip (start 10mg/hr AFTER bolusing to keep above threshold)
- Switching loops (40 PO lasix = 10-20 PO torsemide = 1 PO bumetanide)
- Augmenting with thiazide (metolazone or chlorthalidone)
6/18
- Switching to drip (start 10mg/hr AFTER bolusing to keep above threshold)
- Switching loops (40 PO lasix = 10-20 PO torsemide = 1 PO bumetanide)
- Augmenting with thiazide (metolazone or chlorthalidone)
6/18

Classic teaching is that bumetanide has better oral availability and that gut edema gets in the way of furosemide absorption.
The @CuriousClinPod did a deep dive debunking this common pearl - it may actually be due to delayed gastric emptying!
curiousclinicians.com/2022/10/01/epi…
7/18
The @CuriousClinPod did a deep dive debunking this common pearl - it may actually be due to delayed gastric emptying!
curiousclinicians.com/2022/10/01/epi…
7/18
Thiazide Timing:
Classic teaching says give thiazide 30 mins before loops since they act distally on the nephron.
This is because thiazides are PO, and loops are usually IV. PO takes longer to be absorbed.
If you are giving both PO, can be done at the same time.
8/18
Classic teaching says give thiazide 30 mins before loops since they act distally on the nephron.
This is because thiazides are PO, and loops are usually IV. PO takes longer to be absorbed.
If you are giving both PO, can be done at the same time.
8/18

Be sure to clearly communicate the desired timing when discussing augmentation with the bedside nurse.
Also, note that thiazides often need to come up from pharmacy and this may delay the timing that the patient receives their diuresis. Plan ahead.
9/18
Also, note that thiazides often need to come up from pharmacy and this may delay the timing that the patient receives their diuresis. Plan ahead.
9/18
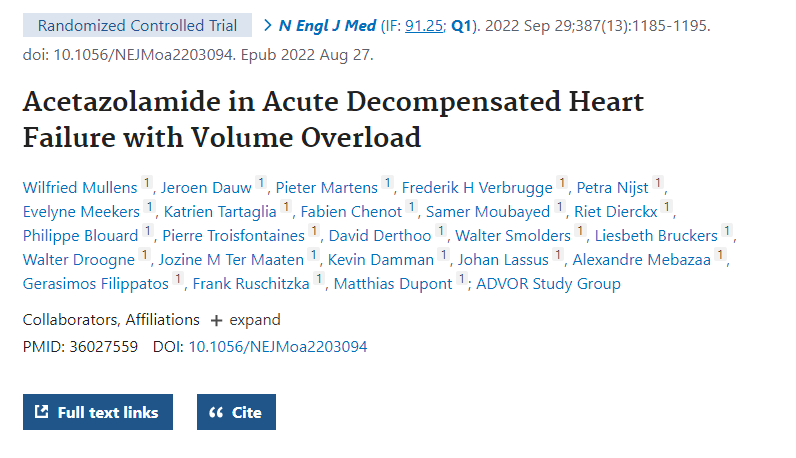
Historically, acetazolamide could be added if the patient was alkalotic.
The ADVOR Trial (NEJM, 2022) showed adding acetazolamide to a loop resulted in greater early decongestion (within 72 hours).
Frankly, idk whether this result should change day-to-day practice.
10/18
The ADVOR Trial (NEJM, 2022) showed adding acetazolamide to a loop resulted in greater early decongestion (within 72 hours).
Frankly, idk whether this result should change day-to-day practice.
10/18
Monitoring:
Daily or BID BMP (K, bicarb, creatinine) and Mag
Hypokalemia will often be the limiting factor holding up aggressive diuresis - replete generously
Watch for symptoms of gout - loop diuretics can lead to hyperuricemia and precipitate a flare!
11/18
Daily or BID BMP (K, bicarb, creatinine) and Mag
Hypokalemia will often be the limiting factor holding up aggressive diuresis - replete generously
Watch for symptoms of gout - loop diuretics can lead to hyperuricemia and precipitate a flare!
11/18
AKI and Diuresis:
Many patients will have prerenal physiology or congestion
Mobilizing 3rd-spaced fluid will decrease effective circulating volume, lower the GFR, and thus increase creatinine
Rarely reflects intrinsic renal damage
Go for euvolemia and trust your exam
12/18
Many patients will have prerenal physiology or congestion
Mobilizing 3rd-spaced fluid will decrease effective circulating volume, lower the GFR, and thus increase creatinine
Rarely reflects intrinsic renal damage
Go for euvolemia and trust your exam
12/18
Daily Volume Assessment:
JVP - surrogate for right atrial pressure; report as normal, high, or low
Hepatojugular Reflux - JVP stays elevated for 10+ seconds after compressing liver
LE Edema - push and hold - graded based on depth and time to rebound (3+ if 60+ seconds)
13/18
JVP - surrogate for right atrial pressure; report as normal, high, or low
Hepatojugular Reflux - JVP stays elevated for 10+ seconds after compressing liver
LE Edema - push and hold - graded based on depth and time to rebound (3+ if 60+ seconds)
13/18
Switching to PO Dosing:
Switch to PO when symptoms resolve and JVP/edema improved
"Sweet spot" of contraction alkalosis without AKI is unreliable
Dry weight is unreliable
Trial PO dose for 24 hours with goal net neg 500cc (patient will likely eat/drink more at home)
14/18
Switch to PO when symptoms resolve and JVP/edema improved
"Sweet spot" of contraction alkalosis without AKI is unreliable
Dry weight is unreliable
Trial PO dose for 24 hours with goal net neg 500cc (patient will likely eat/drink more at home)
14/18
Planning for Discharge:
Ask patient to weigh themselves daily.
If LE edema worsens OR gain 5+ lbs over 3-4 days OR gain 2-3 lbs over 24-48 hours, double the home diuretic dose and call PCP or cardiologist for further guidance.
15/18
Ask patient to weigh themselves daily.
If LE edema worsens OR gain 5+ lbs over 3-4 days OR gain 2-3 lbs over 24-48 hours, double the home diuretic dose and call PCP or cardiologist for further guidance.
15/18
Here are some other key trials that inform our diuresis strategies.
ESCAPE - no need for swans to guide diuresis in typical ADHF without shock
DOSE - bolusing diuretics just as good as drip
CARESS-HF - diuresis preferred first over ultrafiltration for volume removal
17/18
ESCAPE - no need for swans to guide diuresis in typical ADHF without shock
DOSE - bolusing diuretics just as good as drip
CARESS-HF - diuresis preferred first over ultrafiltration for volume removal
17/18

If You Remember Nothing Else:
- Don't miss shock (may see low UOP)
- Bolus early in AM; check within 1 hour
- Diurese based on symptoms and volume exam, not just weight
- Diurese through mild creatinine bumps
- Resistance - drip vs different loop vs thiazide
18/18
- Don't miss shock (may see low UOP)
- Bolus early in AM; check within 1 hour
- Diurese based on symptoms and volume exam, not just weight
- Diurese through mild creatinine bumps
- Resistance - drip vs different loop vs thiazide
18/18
@ASanchez_PS
@dereckwpaul
@EvonneMcArthur
@MadellenaC
@Gurleen_Kaur96
@Mark_Heslin
@bharatbalan
@lukasronnerMD
@EdanZitelny
Brain trust - anything else you like to highlight when teaching students and interns about diuresis?
@dereckwpaul
@EvonneMcArthur
@MadellenaC
@Gurleen_Kaur96
@Mark_Heslin
@bharatbalan
@lukasronnerMD
@EdanZitelny
Brain trust - anything else you like to highlight when teaching students and interns about diuresis?
I hope you've found this thread valuable!
Follow me @ROKeefeMD for more clinical threads and pearls!
Like/Retweet the first tweet below if you can:
Follow me @ROKeefeMD for more clinical threads and pearls!
Like/Retweet the first tweet below if you can:
https://twitter.com/ROKeefeMD/status/1655678995676172290
You can read the unrolled version of this thread here: typefully.com/ROKeefeMD/I4TR…
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter





