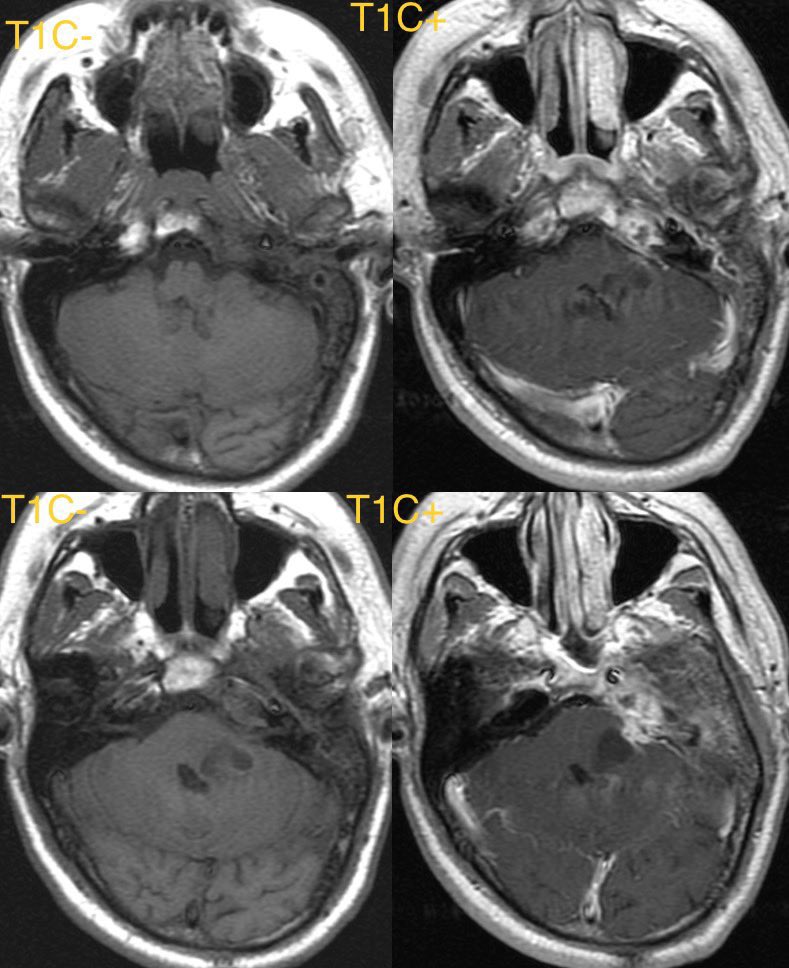
Learning case in this 40 y/o F with history of whole brain radiation as a child for brain tumor treatment
#NeuroRad #neurosurgery #Neurology @TheASNR #NeuroTwitter #meded #radres



#NeuroRad #neurosurgery #Neurology @TheASNR #NeuroTwitter #meded #radres


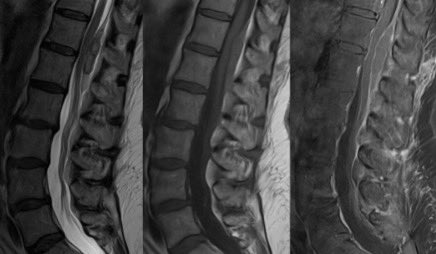
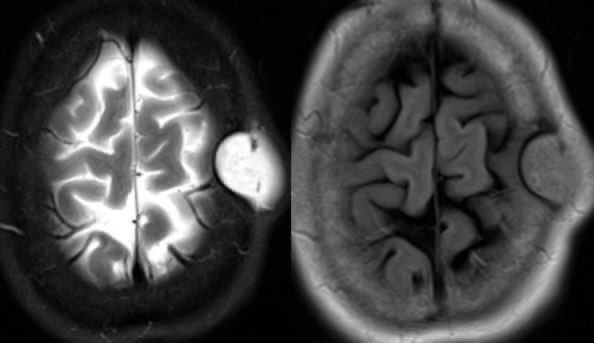
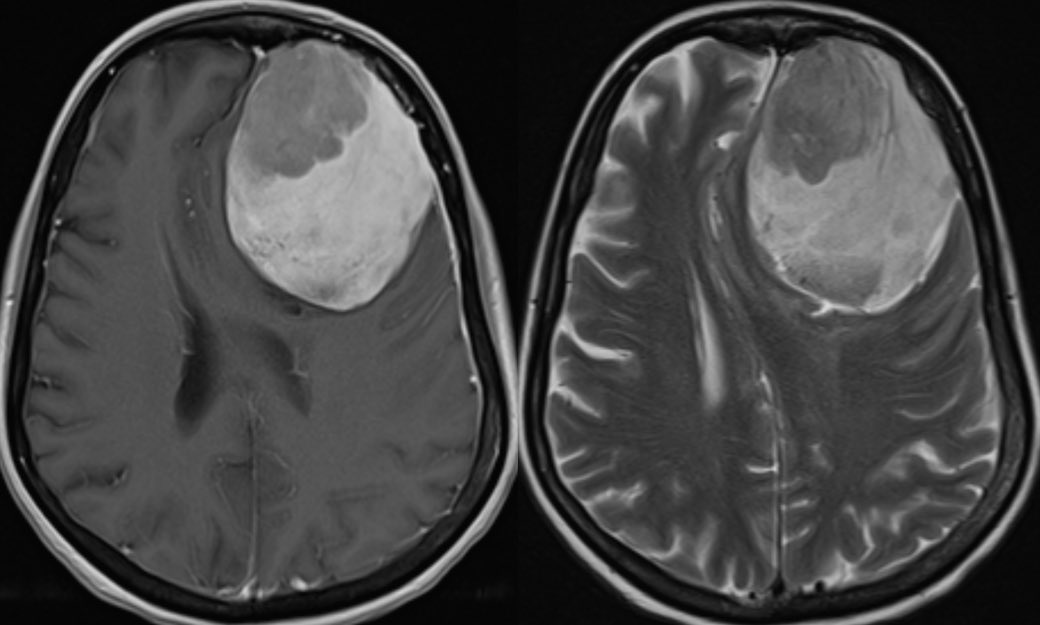
Brain radiation is a risk factor for the development of meningiomas …this patient subsequently developed multiple meningiomas including this large frontal meningioma 
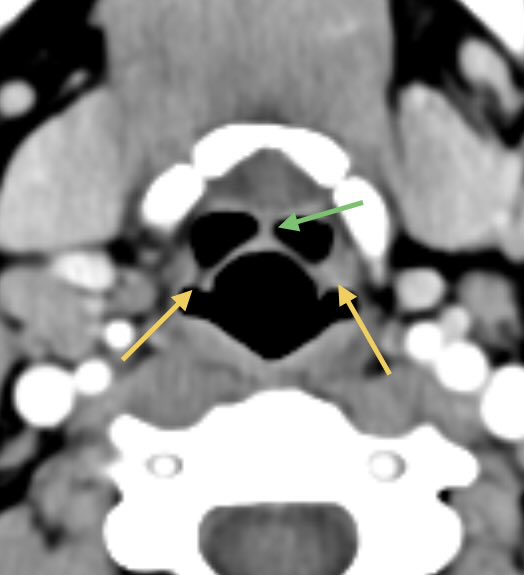
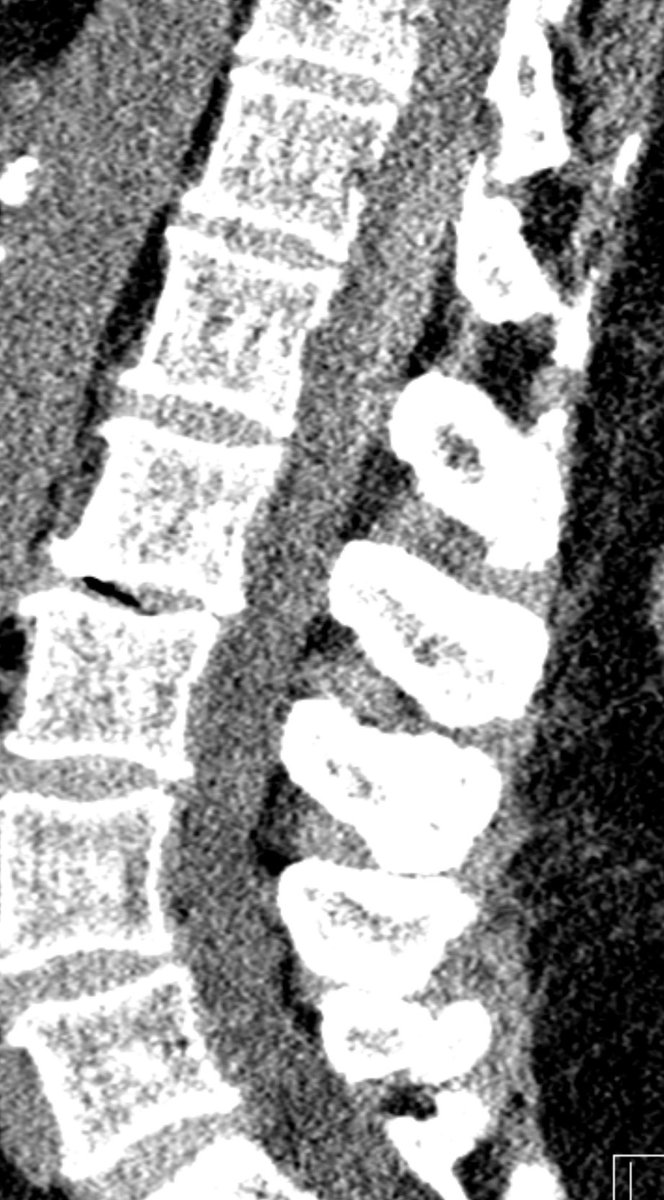
The mass was treated and immediate post op CT shows expected post op change with the resection cavity, some hemorrhage, and pneumocephalus 

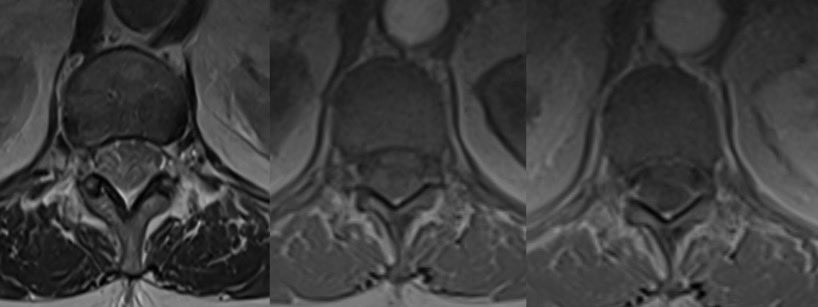
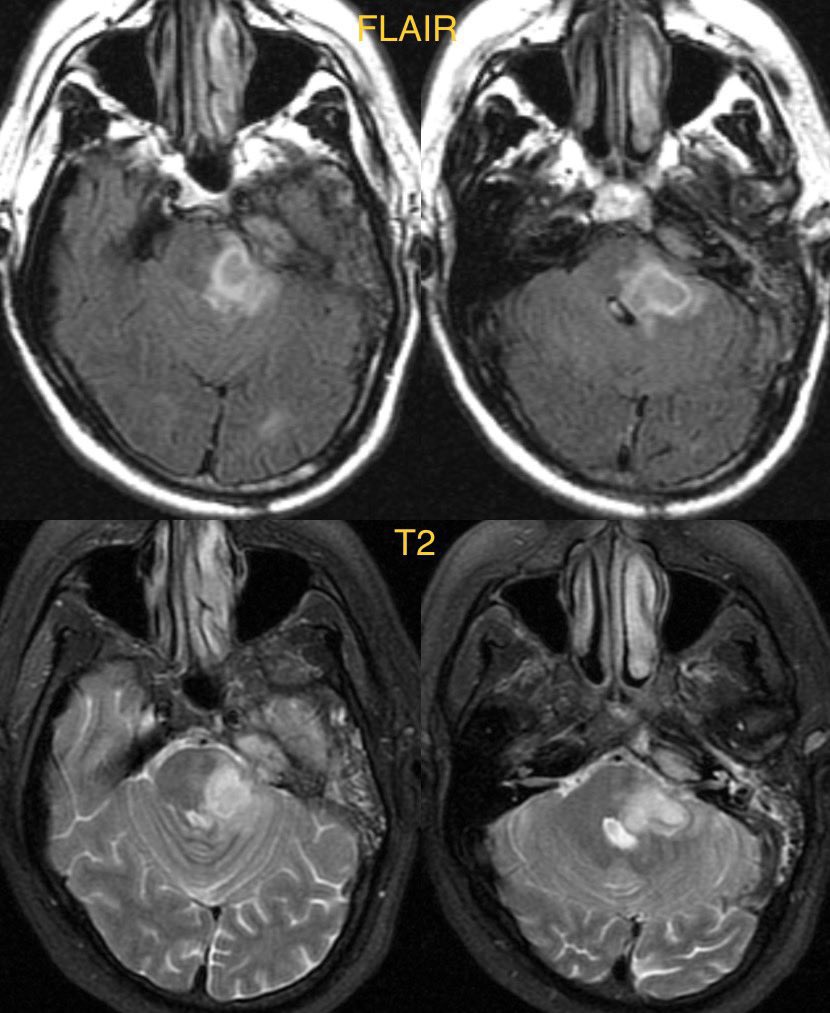
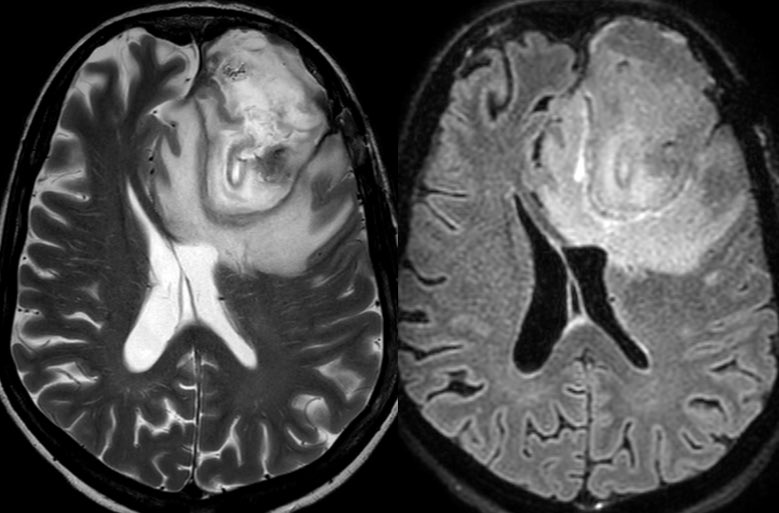
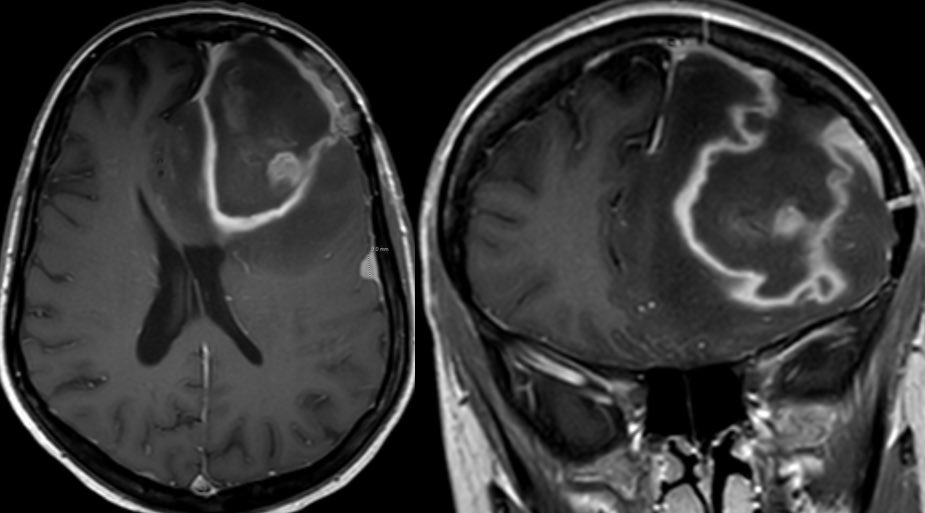
1 month later the patient presents with worsening headaches so an MRI was ordered to eval for post op infection
It can be tricky teasing out organizing hematoma from purulent material on MR. CT may not be as helpful as hematoma will reduce in density overtime
It can be tricky teasing out organizing hematoma from purulent material on MR. CT may not be as helpful as hematoma will reduce in density overtime
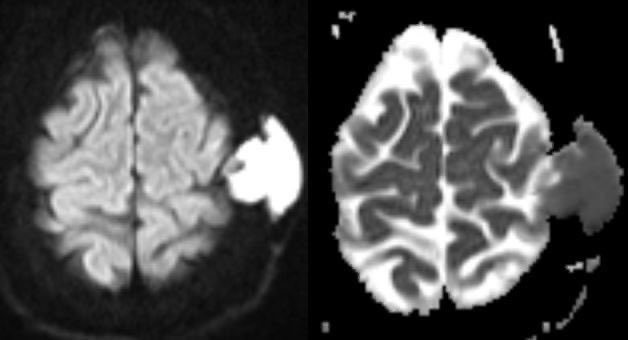
we see here there are areas of restricted and intermediate diffusivity within the resection cavity which can be from purulence or blood product 

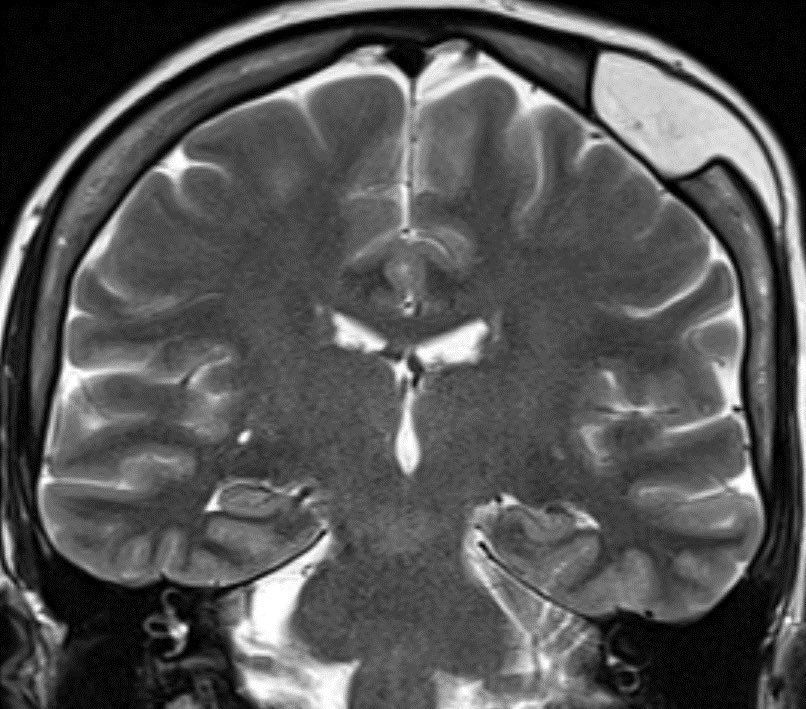
Given the patchy intrinsic T1 hyperintensity, we know at least some of this is related to subacute blood 

Patchy hypointensity on SWI is also out of proportion to what one would expect from free radical formation along the periphery in abscess, so this is mostly from blood and perhaps foci of pneumocephalus 

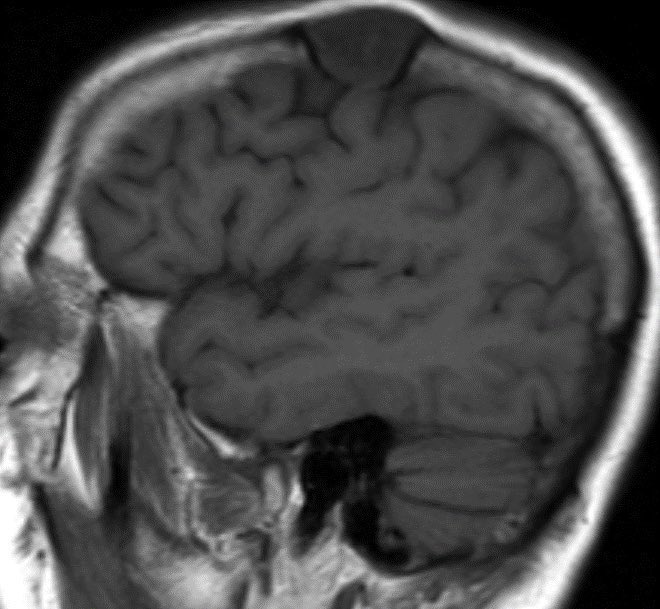
However, there is too much vasogenic edema and mass effect for a 1 month post op. Post op edema and blood should progressively decrease while an infected cavity would increase 



OR confirmed both blood and pus
Learning points:
💡 CLINICAL SIGNS OF INFECTION ARE MOST IMPORTANT
💡 PROGRESSIVE or OUT of proportion vasogenic edema suggests infection (though do NOT forget about possibility of tumor recurrence!)
Learning points:
💡 CLINICAL SIGNS OF INFECTION ARE MOST IMPORTANT
💡 PROGRESSIVE or OUT of proportion vasogenic edema suggests infection (though do NOT forget about possibility of tumor recurrence!)
• • •
Missing some Tweet in this thread? You can try to
force a refresh