An older man comes to the ED with abrupt onset nausea, & diarrhea
He is joined by her daughter whom he is visiting from abroad
Testing is below
The diagnosis is unclear
Until his daughter got just as sick too
🧵
#livertwitter #liverstory #MedTwitter
He is joined by her daughter whom he is visiting from abroad
Testing is below
The diagnosis is unclear
Until his daughter got just as sick too
🧵
#livertwitter #liverstory #MedTwitter

ALT >1000 has a narrow differential diagnosis
There's lots of tests you can order.
But most diagnoses are made in the H+P
Like this one
In fact, in this case, my attending said the diagnosis was obvious from the beginning
Just not to me
https://twitter.com/ebtapper/status/1031555677095948289?s=20
There's lots of tests you can order.
But most diagnoses are made in the H+P
Like this one
In fact, in this case, my attending said the diagnosis was obvious from the beginning
Just not to me
When I meet someone with ALT>1000, I think:
1⃣Ischemic hepatitis. Right 🫀failure? 🫀-genic shock? Cool legs?
2⃣Biliary 🪨. Pain? imaging!
3⃣Drug induced liver injury. Tylenol? Run every med through livertox.gov
4⃣Viral hep. Hep A/B/C
But these weren’t the answers
1⃣Ischemic hepatitis. Right 🫀failure? 🫀-genic shock? Cool legs?
2⃣Biliary 🪨. Pain? imaging!
3⃣Drug induced liver injury. Tylenol? Run every med through livertox.gov
4⃣Viral hep. Hep A/B/C
But these weren’t the answers
The daughter getting sick, that was the clue
Two people from the same house have acute liver injury
Was it hep A? Good thought. But both were immune.
Question: What exposure have they shared?
Answer: Dad made omelets this morning
Two people from the same house have acute liver injury
Was it hep A? Good thought. But both were immune.
Question: What exposure have they shared?
Answer: Dad made omelets this morning
Amanita Phalloides - Death Cap - mushroom poisoning
1. Case-fatality rate of 10-20%
2. Dose-dependent. 1 or 2 mushrooms can kill
3. Phases: incubation (6-24h), GI (severe N/V/D;24-48h), liver injury
4. The cause of death is liver failure


1. Case-fatality rate of 10-20%
2. Dose-dependent. 1 or 2 mushrooms can kill
3. Phases: incubation (6-24h), GI (severe N/V/D;24-48h), liver injury
4. The cause of death is liver failure



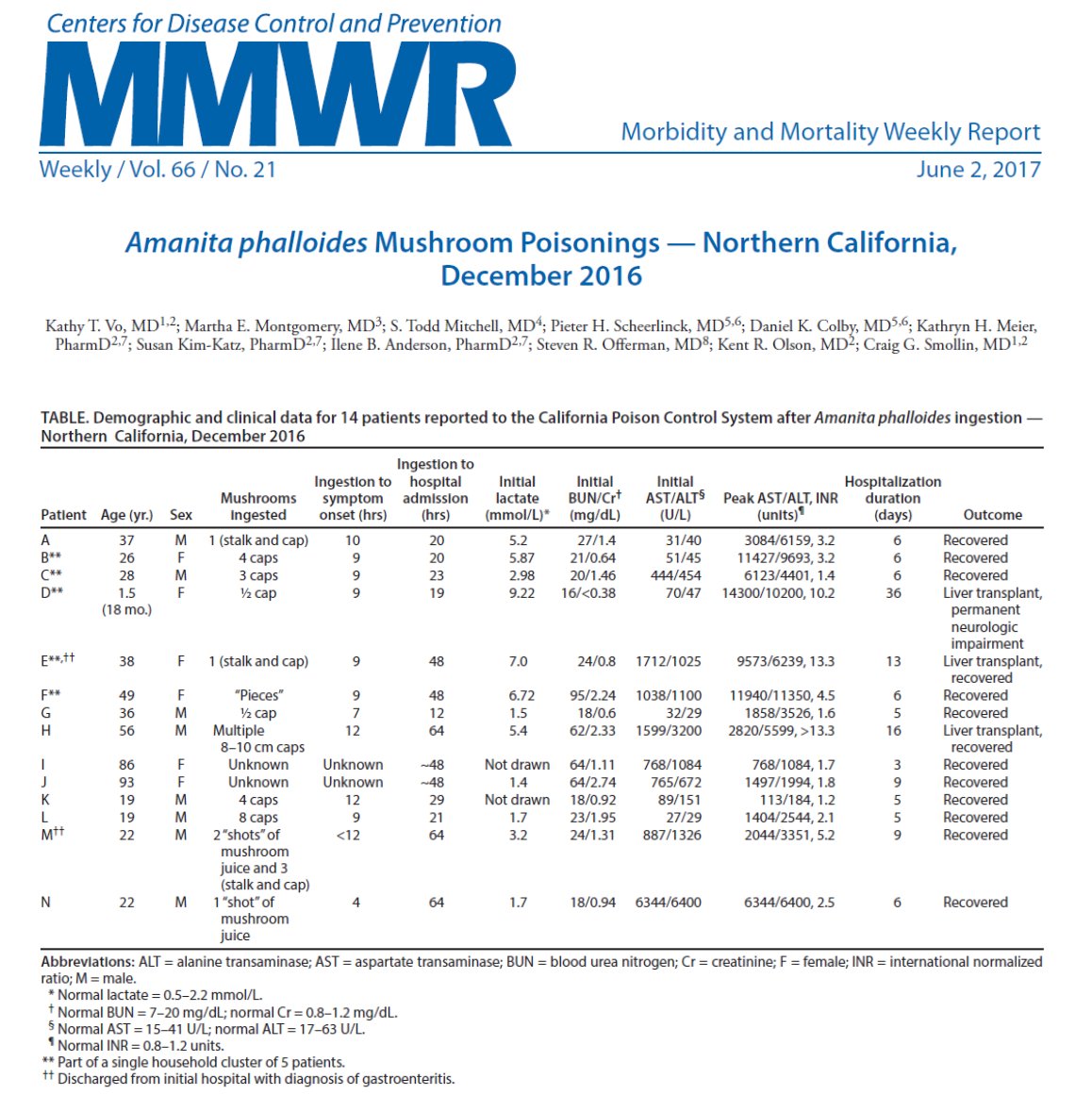
A recent outbreak of amanita poisoning in California showed that death can be avoided with liver transplant.
In this case series, many people recovered without transplant. All patients received a smattering of treatments
So how do we treat amanita poisoning?
In this case series, many people recovered without transplant. All patients received a smattering of treatments
So how do we treat amanita poisoning?
But first, we need to know how Amanita causes liver injury
1. It's heat stable. Cant cook it dead
2. Acid stable. Gut cant neutralize
3. Water soluble. Amanita is full of toxins but only amatoxin is absorbed in the gut. It goes directly to the liver
Also: it looks crazy👇
1. It's heat stable. Cant cook it dead
2. Acid stable. Gut cant neutralize
3. Water soluble. Amanita is full of toxins but only amatoxin is absorbed in the gut. It goes directly to the liver
Also: it looks crazy👇

When amatoxin reaches the liver, it binds OATPB13 and the hepatocyte brings it in
Then it inhibits DNA-dependent RNA polymerase II and cell function ceases
Massive liver cell necrosis ensues

Then it inhibits DNA-dependent RNA polymerase II and cell function ceases
Massive liver cell necrosis ensues


If - IF - there is a treatment, it acts by blocking gut absorption, liver cell uptake, or hepatocyte death
Gastric lavage is often recommended but this is only if the ingestion is very recent
After that...referral to a transplant center is all I am confident in
Gastric lavage is often recommended but this is only if the ingestion is very recent
After that...referral to a transplant center is all I am confident in
This figure shows the survival rates by treatments attempted.
One of the most common is Benzylpenicillin (Penicillin G, Bp). No one knows for sure if it works or how but it possibly blocks amatoxin-polymerase interaction
N-acetylcysteine is frequently given too. Why not?
One of the most common is Benzylpenicillin (Penicillin G, Bp). No one knows for sure if it works or how but it possibly blocks amatoxin-polymerase interaction
N-acetylcysteine is frequently given too. Why not?

Liver cell uptake may be inhibited by silibinin
1. It blocks amatoxin binding to OATPB13
2. It prevented liver injury in a controlled trial in beagles
3. Uncontrolled studies in people have been used to suggest benefit


1. It blocks amatoxin binding to OATPB13
2. It prevented liver injury in a controlled trial in beagles
3. Uncontrolled studies in people have been used to suggest benefit



You might wonder what silibinin is
It is an active ingredient from milk thistle!
Many of the patients in this case series received it IV in a Phase 2 trial that closed without data (clinicaltrials.gov/ct2/show/resul…)
There will be more on milk thistle in a forthcoming tweetorial
It is an active ingredient from milk thistle!
Many of the patients in this case series received it IV in a Phase 2 trial that closed without data (clinicaltrials.gov/ct2/show/resul…)
There will be more on milk thistle in a forthcoming tweetorial

So how did our patients do?
Both recovered without the need for liver transplant. One was enrolled in a phase 2 trial, receiving IV Milk Thistle (Silibinin).
Along the way they taught us many things:
Both recovered without the need for liver transplant. One was enrolled in a phase 2 trial, receiving IV Milk Thistle (Silibinin).
Along the way they taught us many things:
Summary
1⃣Think amanita if acute liver injury with severe nausea, vomiting, and diarrhea
2⃣Mechanism of amanita liver injury: inhibition of RNA polymerase
3⃣PenG, NAC, and Silibin are frequently given but robust evidence for use is limited
1⃣Think amanita if acute liver injury with severe nausea, vomiting, and diarrhea
2⃣Mechanism of amanita liver injury: inhibition of RNA polymerase
3⃣PenG, NAC, and Silibin are frequently given but robust evidence for use is limited
I hope you enjoyed this #liverstory from long ago. I will return soon with a tweetorial on milk thistle.
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter






