Stress fractures - a detailed thread 🦴🦴🦴
I thought I'd put together an overview & some clinical nuggets from the 'coal-face'
First up, I prefer to call them 'bone stress injuries' - majority don't have a # line on imaging & the language can be scary / nocebic for some
I thought I'd put together an overview & some clinical nuggets from the 'coal-face'
First up, I prefer to call them 'bone stress injuries' - majority don't have a # line on imaging & the language can be scary / nocebic for some

Pathophysiology & risk factors
Stress fractures-
Occur in normal bone that is placed under abnormal / persistent load & strain ('training / sporting error')
Insufficiency fractures-
Occur in bone that is under normal strain but is structurally vulnerable eg metabolic conditions
Stress fractures-
Occur in normal bone that is placed under abnormal / persistent load & strain ('training / sporting error')
Insufficiency fractures-
Occur in bone that is under normal strain but is structurally vulnerable eg metabolic conditions

In reality, can be a combination of both to varying degrees - not 'black & white'
Special mention goes to RED-S which often underpins BSI in athletes - men & women!
Ask about relationship with food (past & present) & menstrial history - periods are a barometer of athlete health
Special mention goes to RED-S which often underpins BSI in athletes - men & women!
Ask about relationship with food (past & present) & menstrial history - periods are a barometer of athlete health

At a granular level, bone physiology, its hormonal control & homeostasis is complex - but the fundamentals are pretty straight forward ⬇️ 

Grading
Fredericson classification originally created for Medial Tibial Stress Syndrome (MTSS) - now extrapolated to other BSIs
Is it helpful?🧐
I occasionally see high grade injuries with minimal pain - & low grade stress reactions with significant symptoms & functional loss
Fredericson classification originally created for Medial Tibial Stress Syndrome (MTSS) - now extrapolated to other BSIs
Is it helpful?🧐
I occasionally see high grade injuries with minimal pain - & low grade stress reactions with significant symptoms & functional loss

However, generally if cortical involvement with fracture line = significant injury & correlates with extended RTP / running timescales
A useful platform for discussion with patient around severity of injury and respecting the injury & realistic timescales
A useful platform for discussion with patient around severity of injury and respecting the injury & realistic timescales
High vs Low risk BSI
Some stress #s need to be treated with extra respect & caution - see table
These are typically under sustained high strain coupled with relatively poor blood supply
Some stress #s need to be treated with extra respect & caution - see table
These are typically under sustained high strain coupled with relatively poor blood supply

These are more likely to go through delayed union & take longer to recover - or indeed even need early orthopaedic opinion - tension / lateral side neck of femur is a good eg
Keep them on your clinical radar & assess specifically for them - lower threshold for imaging

Keep them on your clinical radar & assess specifically for them - lower threshold for imaging


Presentation
Gradual onset with persistent impact activity - but occasionally patient describes acute onset pain/ 'crack'
Pain on impact / 'first step' - tendon conditions often ‘warm up’ - unusual with BSI
Some with lower grade BSI can often run through it, but ⬇️performance
Gradual onset with persistent impact activity - but occasionally patient describes acute onset pain/ 'crack'
Pain on impact / 'first step' - tendon conditions often ‘warm up’ - unusual with BSI
Some with lower grade BSI can often run through it, but ⬇️performance

Rest & night pain when high grade
Ache, throb at rest - sharp, shooting under load - pelvic & proximal femur BSIs can feel 'neural' & refer into lower limb
Description of loss of power output, control, heaviness
Ache, throb at rest - sharp, shooting under load - pelvic & proximal femur BSIs can feel 'neural' & refer into lower limb
Description of loss of power output, control, heaviness
Assessment
Lower limb & pelvic - 'Hop test' invariably positive - shut down, reduced power output
Sacral stress # - SIJ provocation tests
FADIR test positive for pubic & neck of femur BSI
Swelling & oedema (esp foot & ankle) around bony tenderness site in absence of trauma

Lower limb & pelvic - 'Hop test' invariably positive - shut down, reduced power output
Sacral stress # - SIJ provocation tests
FADIR test positive for pubic & neck of femur BSI
Swelling & oedema (esp foot & ankle) around bony tenderness site in absence of trauma


Imaging - X-ray
X-rays ➡️poor sensitivity eg ~ 85% of pelvic stress #s are missed on plain films
More likely to pick up a BSI in later stages (eg 4 weeks+) due to callus formation
But better than nothing, esp if suspecting high grade high risk BSI eg ant tibial

X-rays ➡️poor sensitivity eg ~ 85% of pelvic stress #s are missed on plain films
More likely to pick up a BSI in later stages (eg 4 weeks+) due to callus formation
But better than nothing, esp if suspecting high grade high risk BSI eg ant tibial


MRI
Close to 100% sensitivity & the modality of choice
It picks up medullary bone oedema (earlier stress reaction) which X-ray & CT can't
It's more sensitive than 2 phase bone scan - plus bone scan non-specific
It also assesses periosteal & wider soft tissue involvement


Close to 100% sensitivity & the modality of choice
It picks up medullary bone oedema (earlier stress reaction) which X-ray & CT can't
It's more sensitive than 2 phase bone scan - plus bone scan non-specific
It also assesses periosteal & wider soft tissue involvement



MRI VIBE sequences ('pseudo CT') are excellent for detailed assessment of pars stress injuries
This can be repeated to assess pars bony healing which takes longer than other BSIs (~3-6 months)
journals.assaf.org.za/index.php/sajs…
https://twitter.com/DrJN_SportsMed/status/1404740855756431362?s=20
This can be repeated to assess pars bony healing which takes longer than other BSIs (~3-6 months)
journals.assaf.org.za/index.php/sajs…

CT
Misconception re CT being accurate at identifying stress
Excellent at picking up & delineating high grade cortical disruption or long-standing changes eg callus formation / periosteal changes
But it's not a first line modality - MRI is gold standard
Misconception re CT being accurate at identifying stress
Excellent at picking up & delineating high grade cortical disruption or long-standing changes eg callus formation / periosteal changes
But it's not a first line modality - MRI is gold standard

Lower threshold for using CT alongside MRI in high risk BSI
Useful where concern re:
Fracture configuration or cortical involvement underestimated on MRI
Healing status / delayed union
Ruing out differential diagnosis eg tumour, osteomyelitis
Useful where concern re:
Fracture configuration or cortical involvement underestimated on MRI
https://twitter.com/DrJN_SportsMed/status/1653786457436307456?s=20
Healing status / delayed union
Ruing out differential diagnosis eg tumour, osteomyelitis
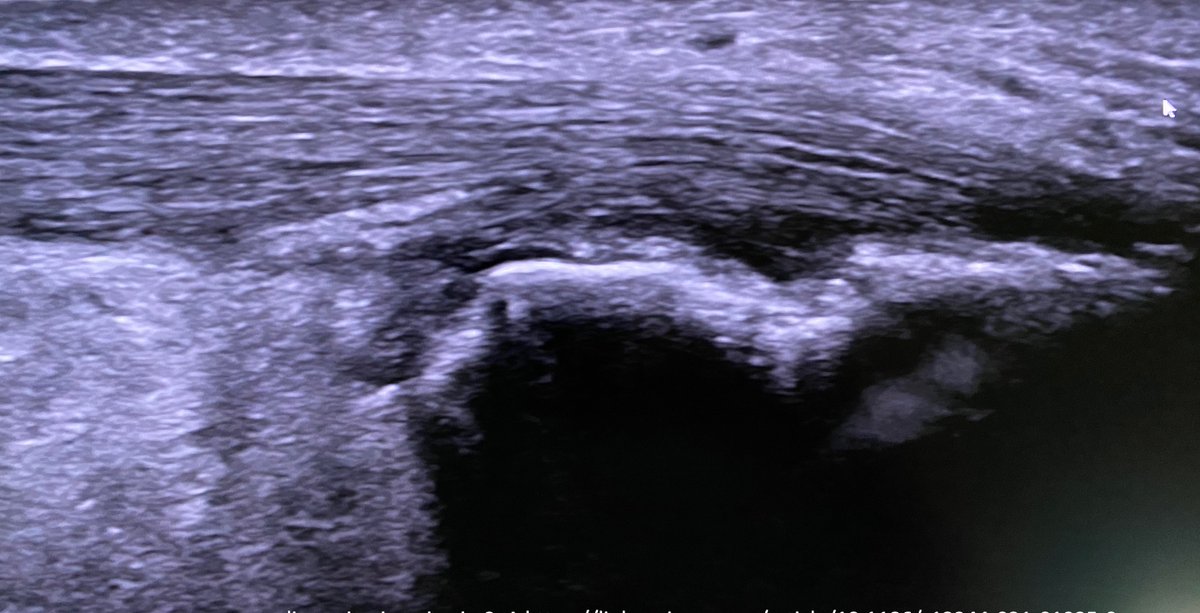
Ultrasound
A quick useful tool at the point of care, time efficient
Can pick up periosteal reaction, callus formation, local soft tissue swelling & inflammation
Like x-ray & CT, won't pick up medullary bone oedema
On balance probably more sensitive than x-ray
A quick useful tool at the point of care, time efficient
Can pick up periosteal reaction, callus formation, local soft tissue swelling & inflammation
Like x-ray & CT, won't pick up medullary bone oedema
On balance probably more sensitive than x-ray

Management
Ideally an MDT approach best esp if RED-S part of the picture - see slide below
Communication key - ? SEM led
Pharmacological Rx 💊💊- specialist decision in difficult cases eg bisphosphonates, teriparatide, transdermal oestrogen (RED-S)
Ideally an MDT approach best esp if RED-S part of the picture - see slide below
Communication key - ? SEM led
Pharmacological Rx 💊💊- specialist decision in difficult cases eg bisphosphonates, teriparatide, transdermal oestrogen (RED-S)

Nutritional & dietary modifications - eg improving macro / calorie intake in cases of low energy availability (LEA)
Vitamin D
Other adjuncts eg shockwave therapy, LIPUS - controversial
Vitamin D
Other adjuncts eg shockwave therapy, LIPUS - controversial
Rehab fundamentals
Return to running & load progressions guided by pain levels & function
Beware 'lag phenomenon' when assessing pain response / flare on⬆️load - delay over 2-3 days
Generally 12-16 weeks RTR
<8 weeks seems a recipe for recurrence & back to 'square 1'
Return to running & load progressions guided by pain levels & function
Beware 'lag phenomenon' when assessing pain response / flare on⬆️load - delay over 2-3 days
Generally 12-16 weeks RTR
<8 weeks seems a recipe for recurrence & back to 'square 1'
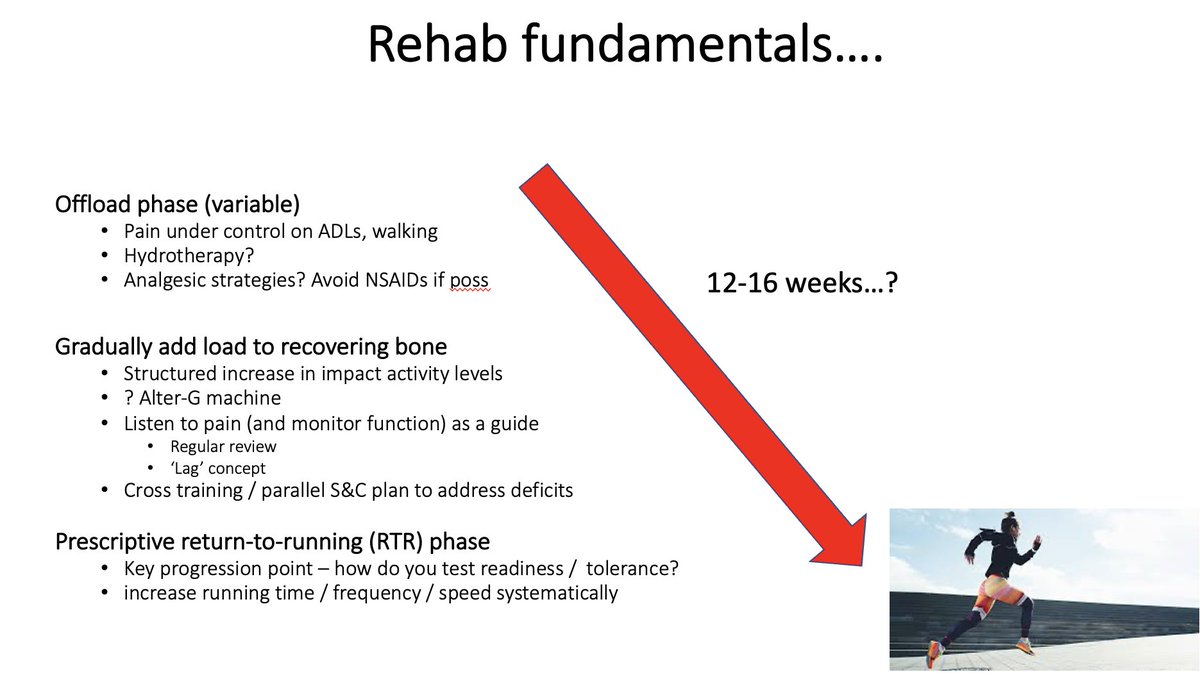
Challenge 😤🙄 the small number of patients who have low levels of pain - or pain settles v quickly with early offload - but high grade stress radiologically
In these cases seems sensible to respect physiology & set arbitrary number of weeks before moving into RTR
In these cases seems sensible to respect physiology & set arbitrary number of weeks before moving into RTR
Some clinicians might not agree with this & have a more pragmatic approach
@rwilly2003 paper has suggested that with MTSS, if pain free for 5 days can begin graded RTR
So clearly can't be rigidly prescriptive / recipe based - every patient different due to personal factors ++
@rwilly2003 paper has suggested that with MTSS, if pain free for 5 days can begin graded RTR
So clearly can't be rigidly prescriptive / recipe based - every patient different due to personal factors ++
Tips:
Time scales variable
Respect physiology
Not ‘one size fits all’
Step count?
Pragmatic approach to cross training
Parallel S&C programme
Education
Alter G – graded exposure?
Time scales variable
Respect physiology
Not ‘one size fits all’
Step count?
Pragmatic approach to cross training
Parallel S&C programme
Education
Alter G – graded exposure?

Why aren't they getting better?
Compliance aside - misdiagnosis might be the cause -
eg rheumatological - enthesopathy with florid bone oedema
Osteoid osteoma tumour - eg proximal femur & calcaneum - here CT will help differentiate



Compliance aside - misdiagnosis might be the cause -
eg rheumatological - enthesopathy with florid bone oedema
Osteoid osteoma tumour - eg proximal femur & calcaneum - here CT will help differentiate
https://twitter.com/DrJN_SportsMed/status/1628905076616994819?s=20



• • •
Missing some Tweet in this thread? You can try to
force a refresh