
Assoc. Prof, University of Colorado Boulder CS and @BioFrontiers.
Math, infectious diseases, networks, and computational social science. https://t.co/Wx0ZlCB94L
How to get URL link on X (Twitter) App


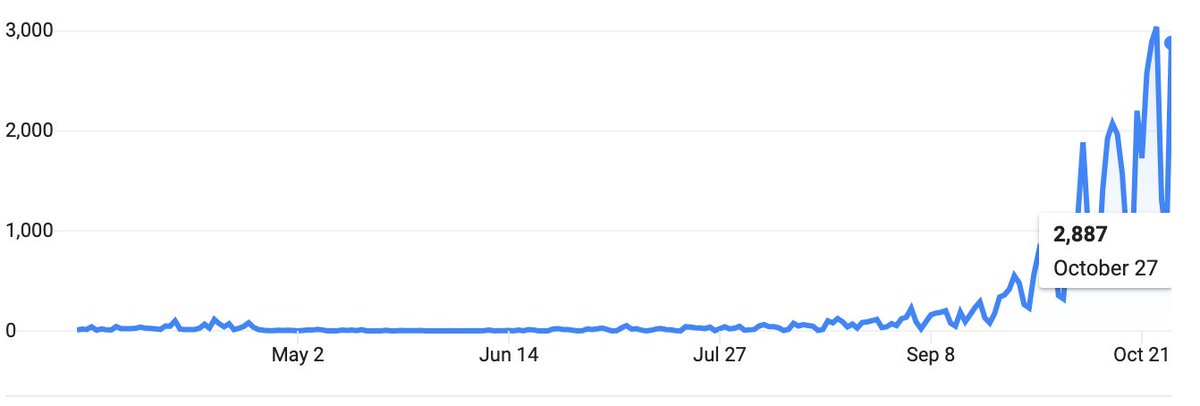
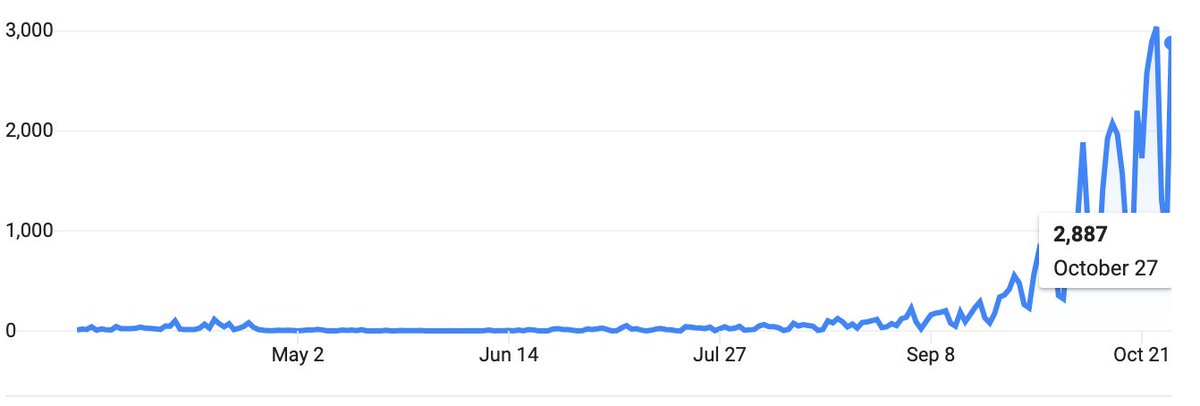
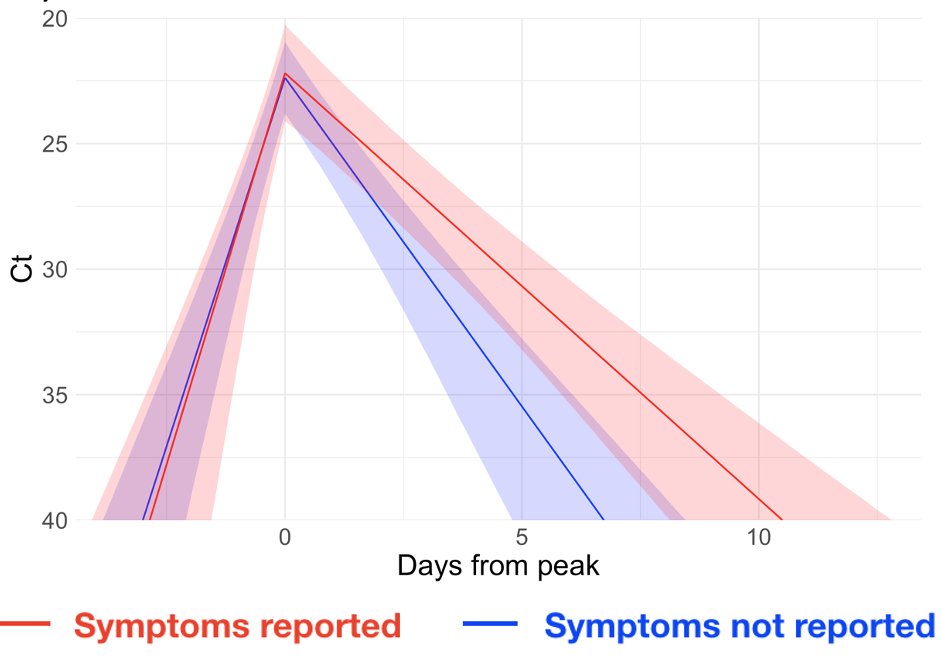
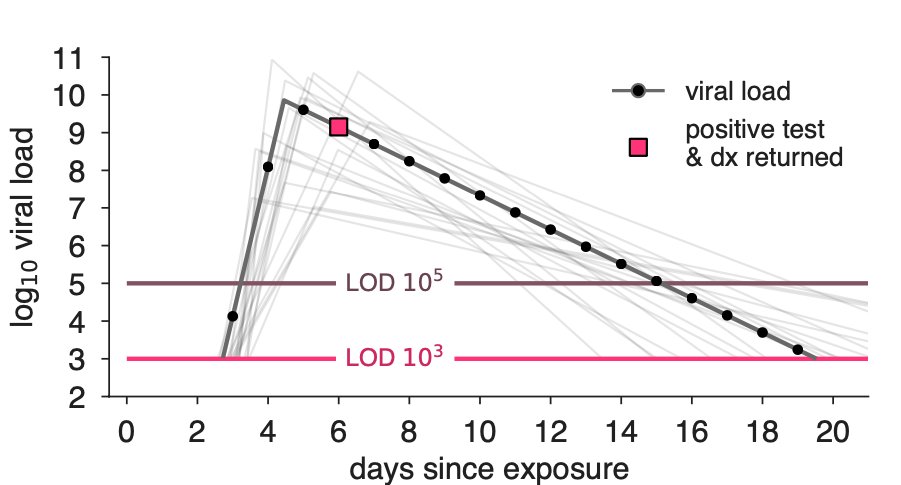
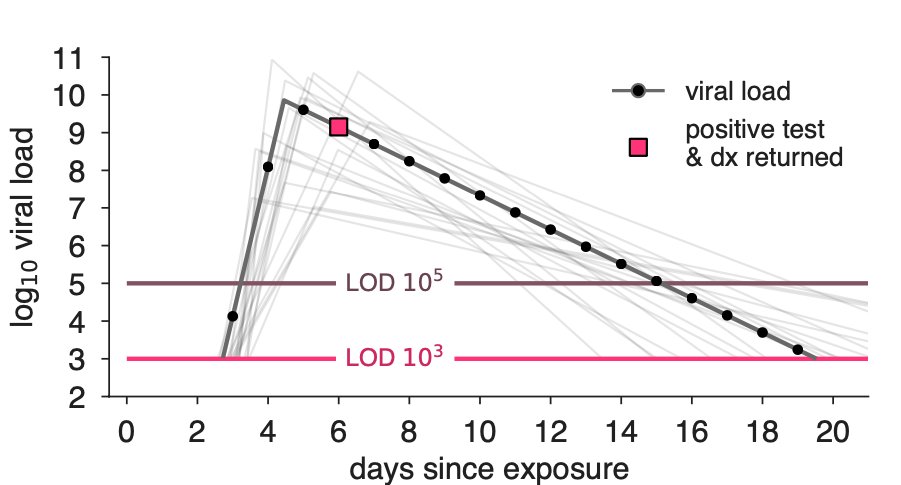
 This means that rapid tests aren't catching people during their first few days of infection. But sensitive PCR tests are slowed by day++ turnarounds.
This means that rapid tests aren't catching people during their first few days of infection. But sensitive PCR tests are slowed by day++ turnarounds.
 By definition: when no one is vaccinated, 0% of infections are breakthroughs. When everyone is vaccinated, 100% of infections are breakthroughs.
By definition: when no one is vaccinated, 0% of infections are breakthroughs. When everyone is vaccinated, 100% of infections are breakthroughs. 


 If vax & infection provided equivalent immunity, a dose-sparing strategy targeting seronegatives could be thought of as increasing vax supply (pic).
If vax & infection provided equivalent immunity, a dose-sparing strategy targeting seronegatives could be thought of as increasing vax supply (pic).


https://twitter.com/bubar_kate/status/1304472235214741504We asked whether transmission-blocking properties affect prioritization. Intuitively, as the vaccine's transmission blocking properties become worse, direct protection of adults 60+ became/remained the clear best prioritization—across countries, R0 values, & vaccine supplies. 2/


https://twitter.com/DanLarremore/status/1276260291764826112I love twitter+preprints precisely because of this community. In the updated preprint, we've corrected a couple typos, and created a new supplement, "Adjustments for false negatives and test refusal" which I'll quickly summarize below. 2/ medrxiv.org/content/10.110…
https://twitter.com/yhgrad/status/1250858246002348034
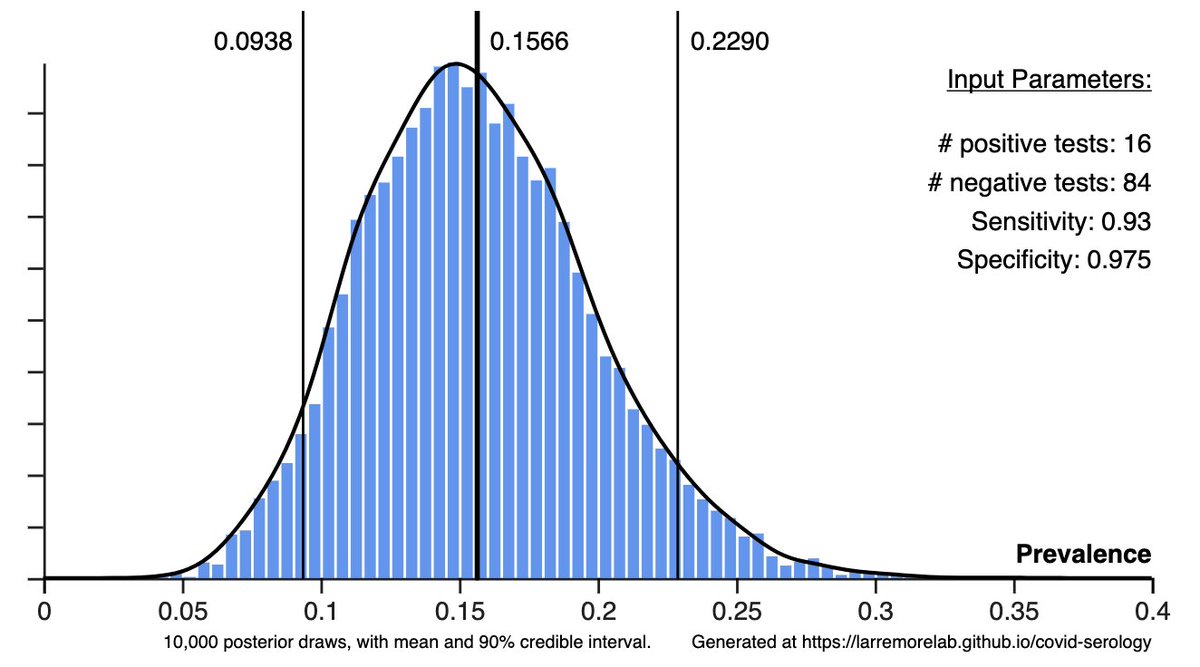
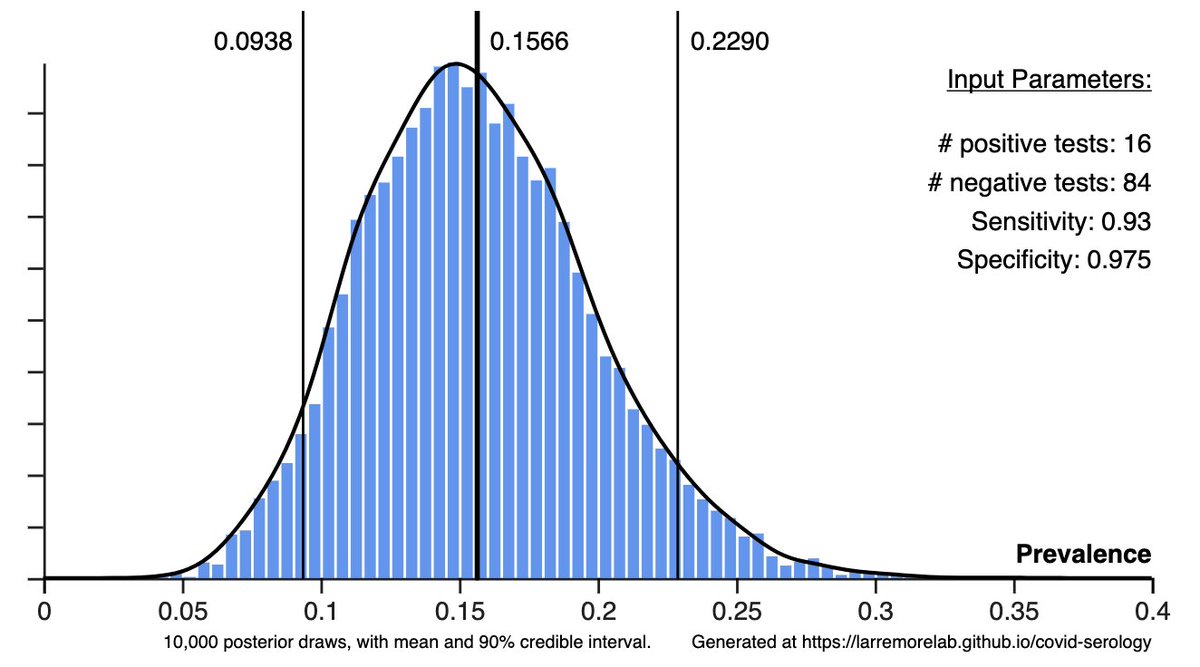 But let's also remember: sensitivity & specificity are *estimated from data*. That means that they, too, need statistical treatment. So for Calculator 2: survey data AND raw assay calibration data → posteriors for prevalence, sensitivity, and specificity. larremorelab.github.io/covid-calculat…
But let's also remember: sensitivity & specificity are *estimated from data*. That means that they, too, need statistical treatment. So for Calculator 2: survey data AND raw assay calibration data → posteriors for prevalence, sensitivity, and specificity. larremorelab.github.io/covid-calculat… 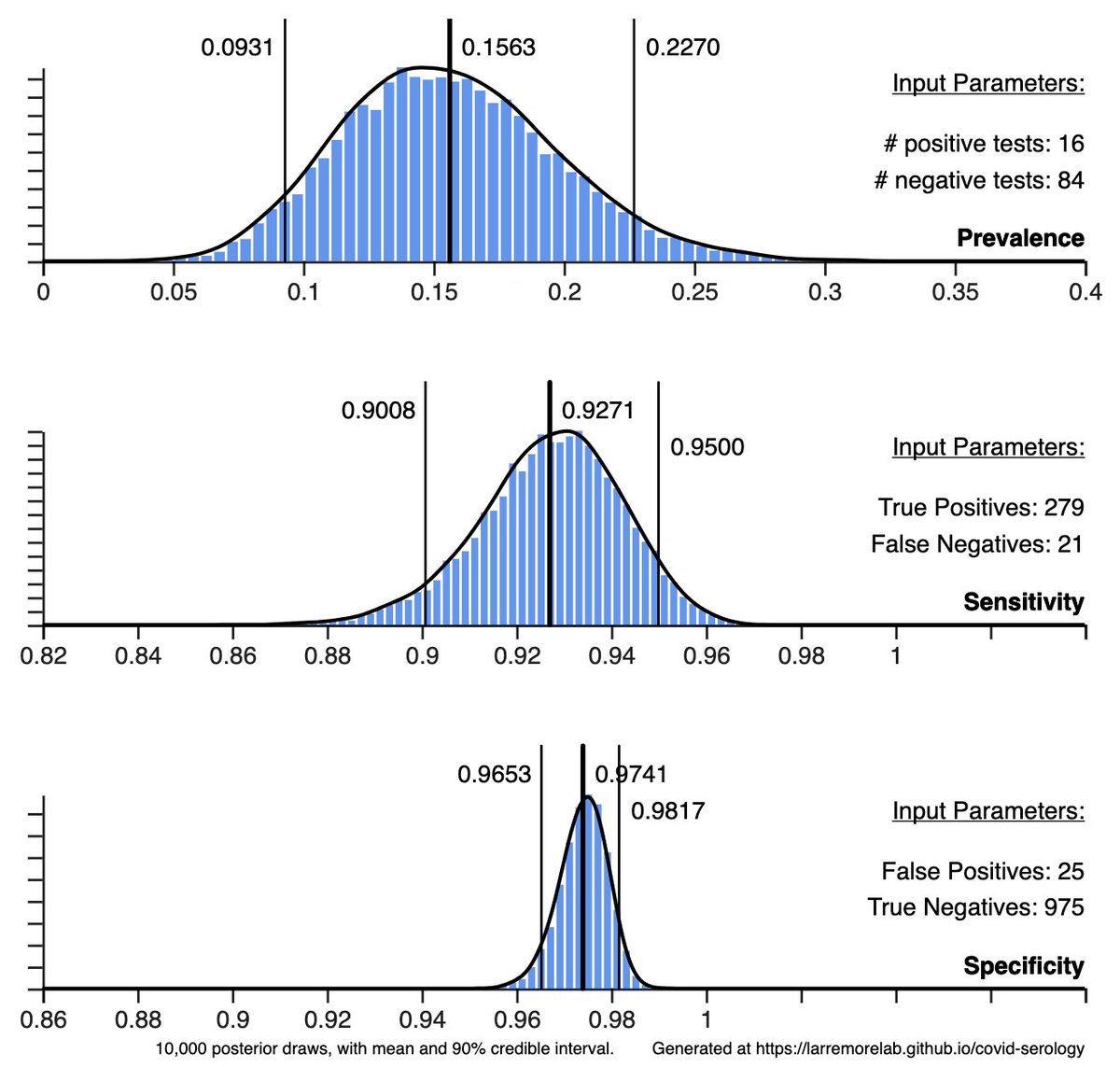

https://twitter.com/yhgrad/status/1250858246002348034?s=20] I want to highlight some #stats and #networks results. 1/ First, the basics. This paper's 1st result is like a statistical inference midterm problem: If you observe n+ positive tests, n- negative tests, and you know the sensitivity/specificity of your test, what is the posterior prob. of actual positives? Solution: Bayes' rule. ✅