
Intensivist & Anaesthetist // Critical Care Echo // ICU Liberty Singer // Podcaster // Clinical Lead for Organ Donation // All views own //
6 subscribers
How to get URL link on X (Twitter) App


https://twitter.com/GoughCJ/status/1305899939281752066One of the key principles here is that the positive pressure delivered into the thorax from the ventilator will affect the venous return to the right heart (with less returning during inspiration).

 The case is a post-op patient who is hypotensive. They have had some fluid resuscitation already. Do they need more filling? Do they need inotropes? Do they need vasopressors?
The case is a post-op patient who is hypotensive. They have had some fluid resuscitation already. Do they need more filling? Do they need inotropes? Do they need vasopressors?https://twitter.com/BBCHughPym/status/12935865627862343711. A person has mild Covid infection and isolates at home for 10 days. They go back to work and are fine. A week later they are killed crossing the road.

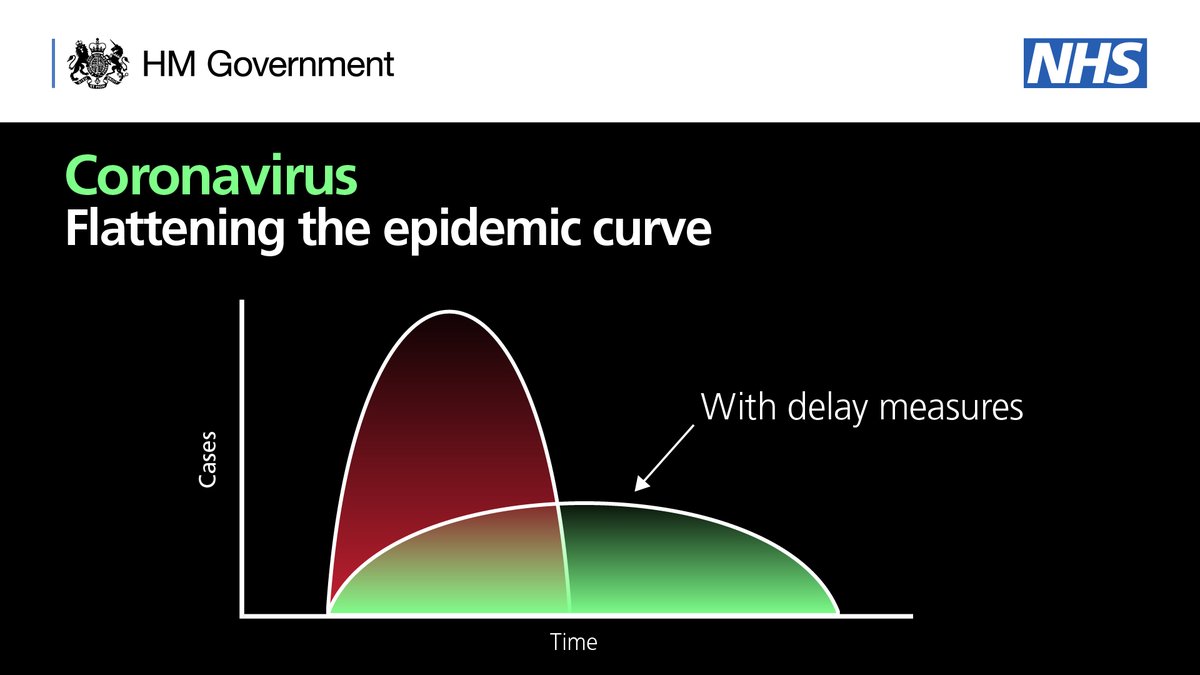
 Even before the #COVIDー19 pandemic, ITUs were typically short staffed and running at almost full capacity.
Even before the #COVIDー19 pandemic, ITUs were typically short staffed and running at almost full capacity. 
 There are two broad types of test:
There are two broad types of test: 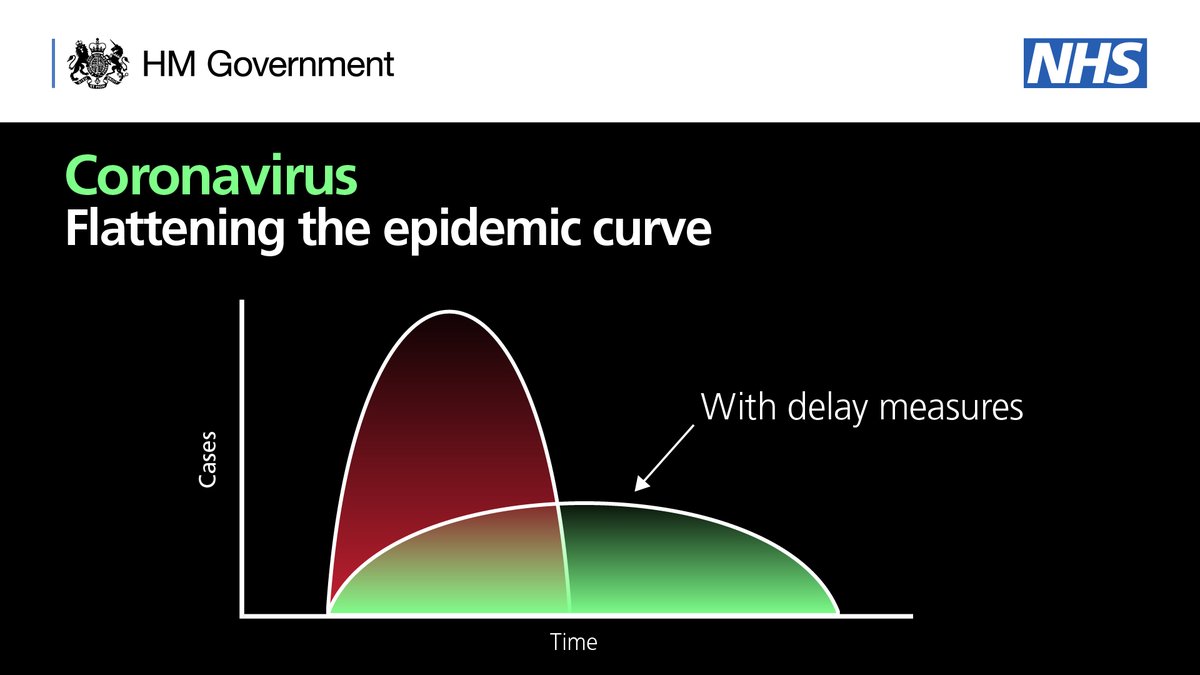
 The predictions were terrifying and depressing. Based on modelling from other countries, NHS England told us to prepare for 140-280 ventilated patients.
The predictions were terrifying and depressing. Based on modelling from other countries, NHS England told us to prepare for 140-280 ventilated patients.