
Senior Fellow @AEI. Partner @NEA. Contributor @CNBC. 23rd Commissioner of the @US_FDA. Public Boards: @Pfizer @Illumina @TempusAI @UHC
86 subscribers
How to get URL link on X (Twitter) App

 It says off label use of a drug will be considered when establishing the "fair price," but only if the use is listed in a CMS recognized compendia -- this probably means that for purposes of setting a price, CMS will only consider the off label uses for cancer drugs. 2/7
It says off label use of a drug will be considered when establishing the "fair price," but only if the use is listed in a CMS recognized compendia -- this probably means that for purposes of setting a price, CMS will only consider the off label uses for cancer drugs. 2/7 





 Recent controversies around at home Ketamine and history related to sublingual formulations of opioids could inform how @US_FDA considers issues related to drugs with characteristics like the new compound being developed by @LusarisTx @rfsquared
Recent controversies around at home Ketamine and history related to sublingual formulations of opioids could inform how @US_FDA considers issues related to drugs with characteristics like the new compound being developed by @LusarisTx @rfsquared https://twitter.com/margbrennan/status/1588704413774147584My argument Summer 2020, after first wave, was: "Schools should open in the fall. It’s critical for meeting the educational and social needs of children. But local officials should have the discretion to take tailored actions to help keep children safe" wsj.com/articles/schoo…
https://twitter.com/scottgottliebmd/status/1457119597723795458?s=42&t=IDUGV6-4zci0lF5bZSLfoA


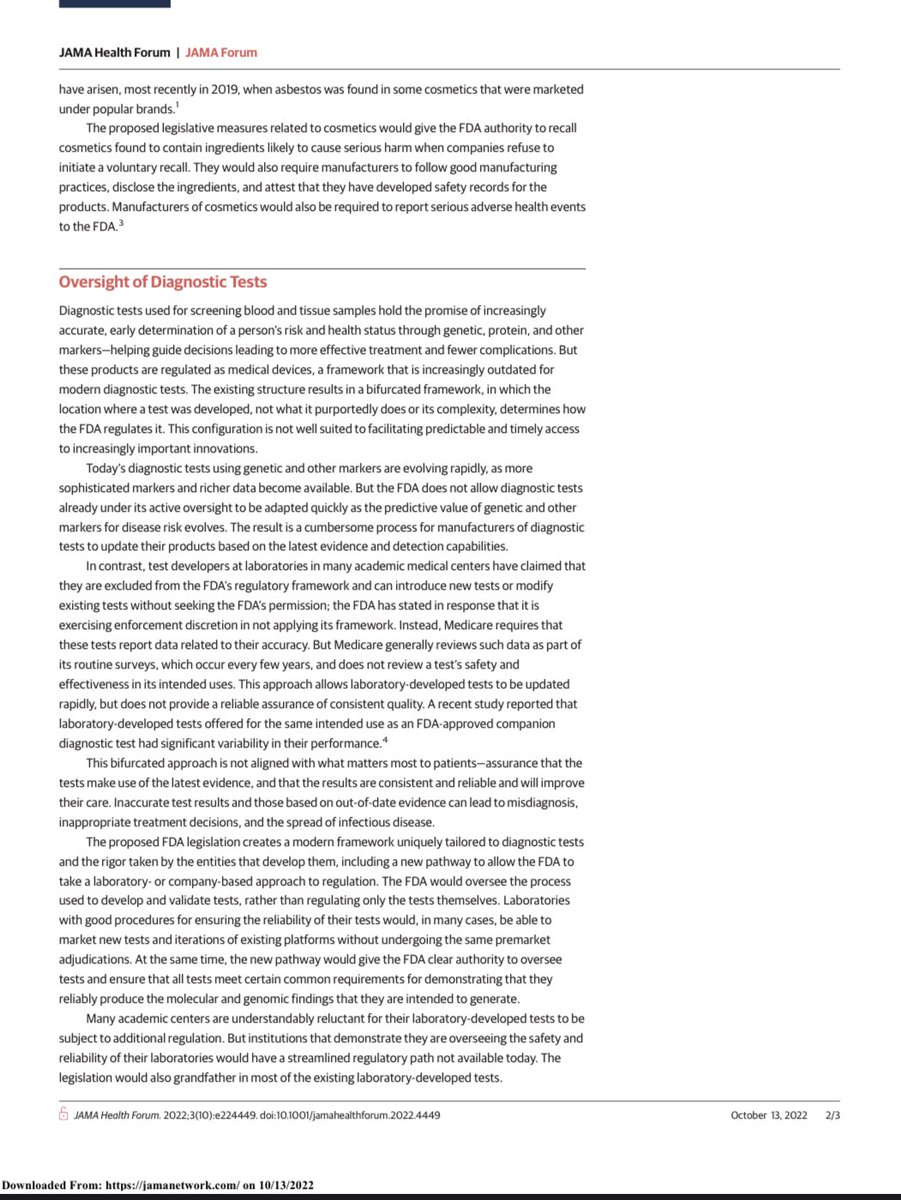
 Background: When I was FDA commissioner, the agency delivered to Congress comprehensive technical assistance on which VALID is based; as I discussed at Friends of Cancer Research in 2017:
Background: When I was FDA commissioner, the agency delivered to Congress comprehensive technical assistance on which VALID is based; as I discussed at Friends of Cancer Research in 2017: https://twitter.com/scottgottliebmd/status/1235692686750797825


 80% of US consumers report using dietary supplements; most mistakenly believe FDA reviews or tests products before they reach market. No such requirements exist and manufacturers often don't disclose ingredients of new products to regulators, consumers 2/x pewtrusts.org/en/research-an…
80% of US consumers report using dietary supplements; most mistakenly believe FDA reviews or tests products before they reach market. No such requirements exist and manufacturers often don't disclose ingredients of new products to regulators, consumers 2/x pewtrusts.org/en/research-an…

 The study supporting intradermal inoculation found similar safety and immunogenicity using 20% of full dose 28 days apart to standard formulation of MVA, concluding that intradermal vaccination could be used to increase number of available doses 5-fold 2/x sciencedirect.com/science/articl…
The study supporting intradermal inoculation found similar safety and immunogenicity using 20% of full dose 28 days apart to standard formulation of MVA, concluding that intradermal vaccination could be used to increase number of available doses 5-fold 2/x sciencedirect.com/science/articl…

https://twitter.com/bbcbreaking/status/1550846981764964353Washington Post writing on the prior WHO decision not to make the declaration: “Monkeypox cases surge as WHO stops short of declaring a global emergency”




 100 million doses of ACAM2000 doesn’t meet the CDC’s claim that “The Strategic National Stockpile (SNS) has stockpiled enough smallpox vaccine to vaccinate every person in the United States,” a pledge that President Bush made in 2002 amidst concerns about the risk of bioterrorism
100 million doses of ACAM2000 doesn’t meet the CDC’s claim that “The Strategic National Stockpile (SNS) has stockpiled enough smallpox vaccine to vaccinate every person in the United States,” a pledge that President Bush made in 2002 amidst concerns about the risk of bioterrorism 




 On closely watched provisions on accelerated approval
On closely watched provisions on accelerated approval


