
Infectious diseases doctor, Clinical Assoc. Prof @StanfordDeptMed | @cidrap writer | views mine | no conflicts of interest
How to get URL link on X (Twitter) App

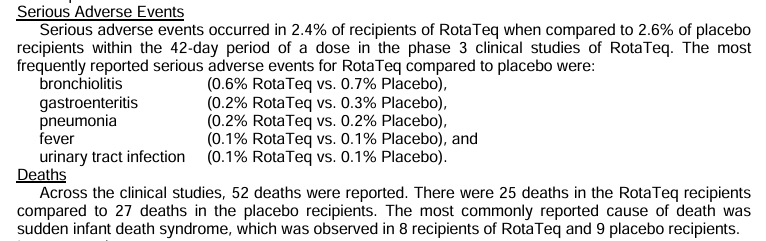
https://twitter.com/MAHA_Action/status/20112287918219841182/ The "three deaths" claim is wrong. Pre-vaccine, rotavirus caused 20 to 60 deaths annually in US children under 5. But focusing on deaths misses the point: rotavirus caused 410,000 physician visits, 200,000+ ER visits, and 55,000-70,000 hospitalizations every year, costing about $1 billion annually. Since vaccination, hospitalizations dropped ~80%. The vaccine prevents 40,000-50,000 hospitalizations per year.

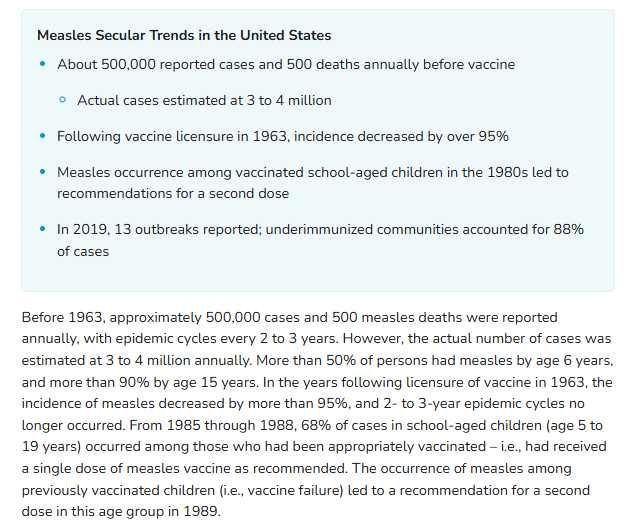
https://twitter.com/joeroganhq/status/2004582980958986471Joe Rogen was born in 1967. The measles vaccine was licensed in 1963, and by the time he was in school, incidence had dropped over 95%. "Everyone got measles" describes his parents' generation, but not his. Chickenpox was actually was universal for Gen X, so maybe he's thinking of that?
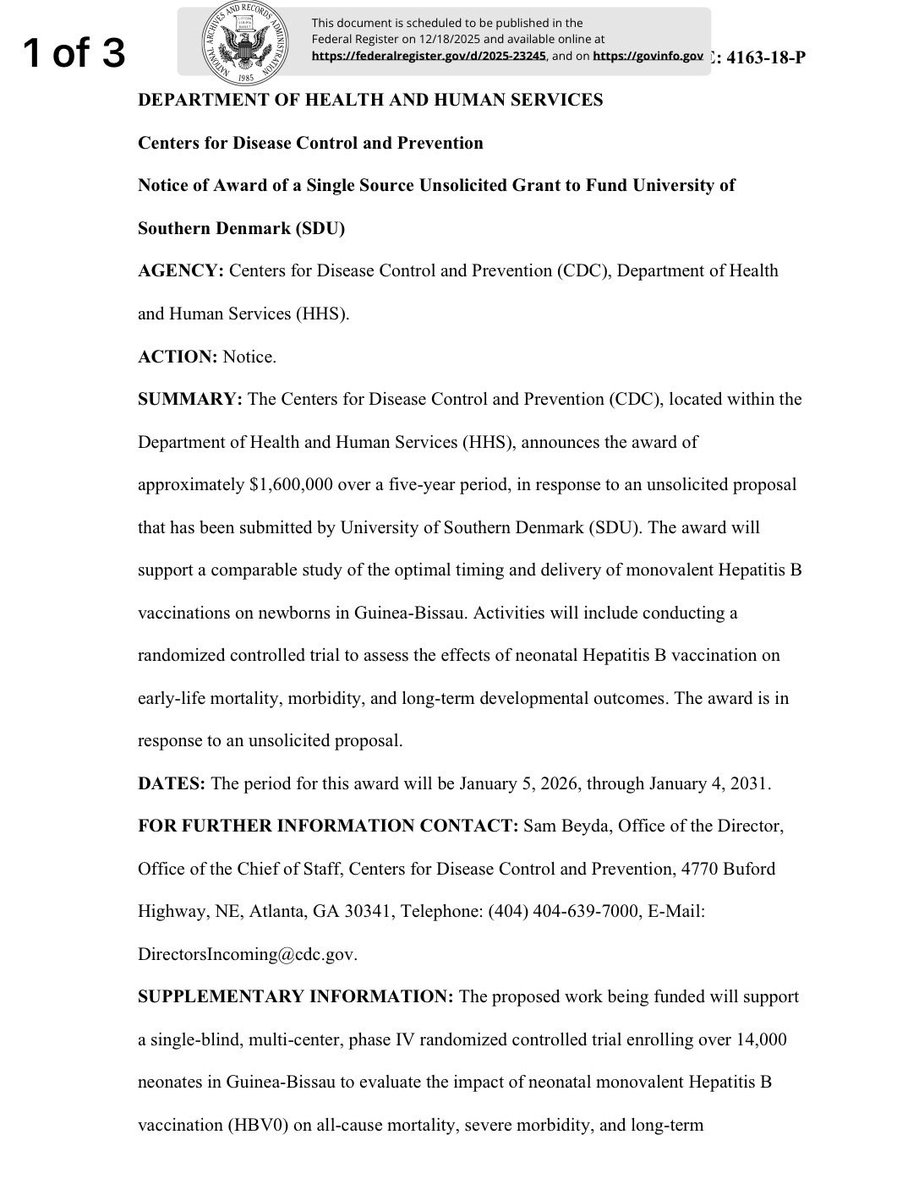
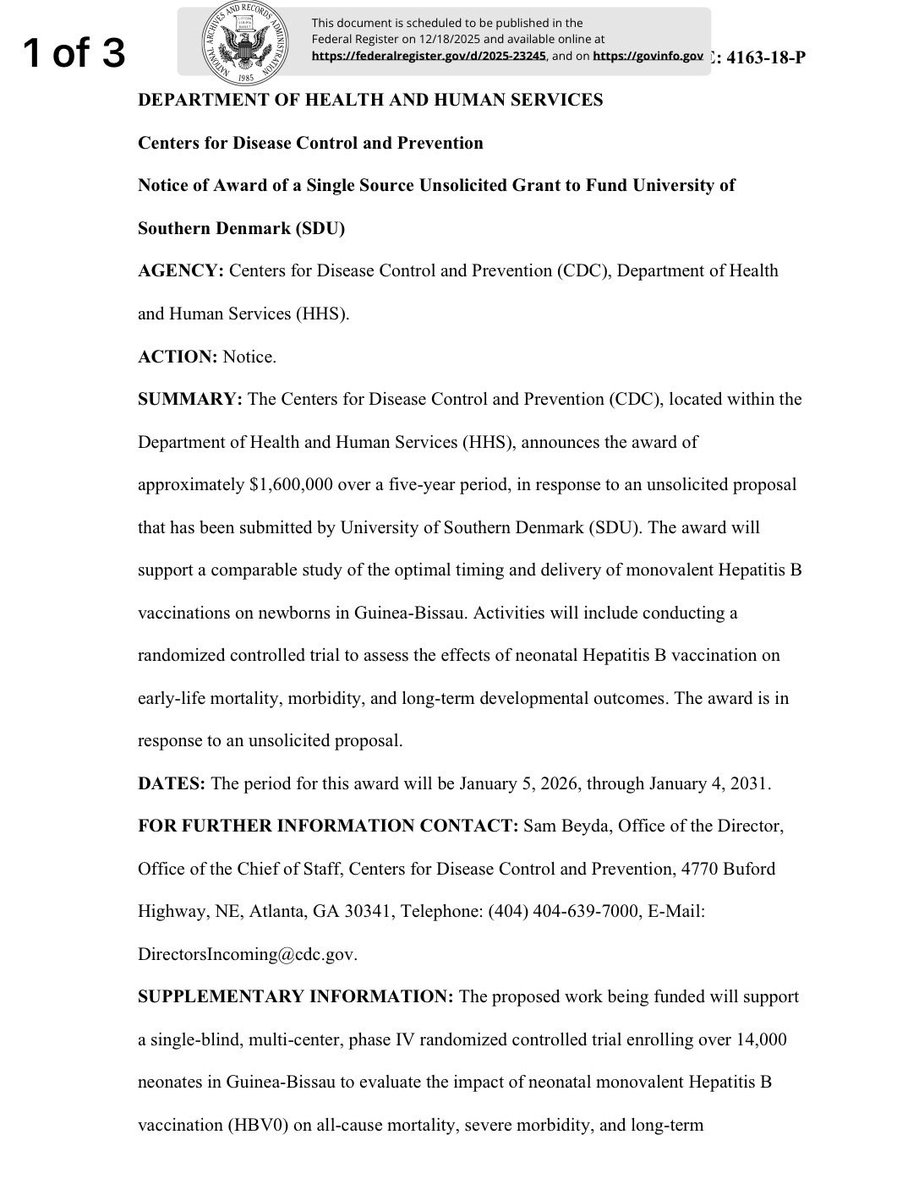 2/ The primary endpoint is “all-cause mortality” - not whether the vaccine prevents hepatitis B, but whether it affects deaths from other causes. This is the non-specific effects framework, which has been used to question established vaccine recommendations. RFK Jr. cited research using this methodology to justify cutting $1 billion to Gavi. npr.org/sections/goats…
2/ The primary endpoint is “all-cause mortality” - not whether the vaccine prevents hepatitis B, but whether it affects deaths from other causes. This is the non-specific effects framework, which has been used to question established vaccine recommendations. RFK Jr. cited research using this methodology to justify cutting $1 billion to Gavi. npr.org/sections/goats…
https://twitter.com/AaronSiriSG/status/19984155142347042771/ THE CORE TRICK
https://twitter.com/MAHA_Action/status/1993758243605110866First, kids don't get 72 vaccines by age 18. The CDC schedule recommends 50-55 doses total, including annual flu shots. The inflated "72" figure may be intended to scare parents but it's false. I wrote about the "too many, too soon" myth here:
https://twitter.com/AaronSiriSG/status/19814024758036032602/ First, the Cochrane review he quotes, but only selectively. Yes, the 2018 review reported “no convincing evidence” that flu vaccines reduced mortality, hospital admissions, serious complications, or community transmission in healthy children. But that reflects a basic limitation of the evidence it examined, not a verdict that vaccines do nothing. The review focused on randomized trials in healthy kids, which were designed to measure how vaccination affects the risk of getting influenza, not rare outcomes like death or ICU admission. Even with more than 200,000 children across 41 trials, you will not see enough deaths or hospitalizations to show a statistically clear difference. That is a limitation of trial size and design, not proof of lack of benefit against severe disease.
https://twitter.com/EvanMcFatridge/status/19648519096192782252/ MEASLES:

https://twitter.com/SecKennedy/status/19514238513149460832/ This study represents gold-standard epidemiological research. Over 24 years, researchers tracked 1.2 million children across 50 health outcomes. Edward Belongia, leading vaccine safety expert: "the largest and most definitive observational study on the safety of vaccine-related aluminum exposure in children" ever conducted. pubmed.ncbi.nlm.nih.gov/40658954/

https://twitter.com/RWMaloneMD/status/19453892269311836891/ Calling mRNA vaccines “genetic ‘vaccine’ products,” with “vaccine” in quotes, is a deliberate rhetorical move that undermines their legitimacy.

https://twitter.com/rwmalonemd/status/19393735838239953612/ Research shows that many Amish families do vaccinate their children. Studies find that anywhere from 41% to 85% of Amish parents have vaccinated at least some of their children, depending on the community and time period.
