
Trainee psychiatrist/Researcher @NELFT @UCLPsychiatry (honorary) . Maudsley Deprescribing Guidelines: https://t.co/MdD00q9Yd1 (US) https://t.co/9eUVpPj52p (UK)
How to get URL link on X (Twitter) App


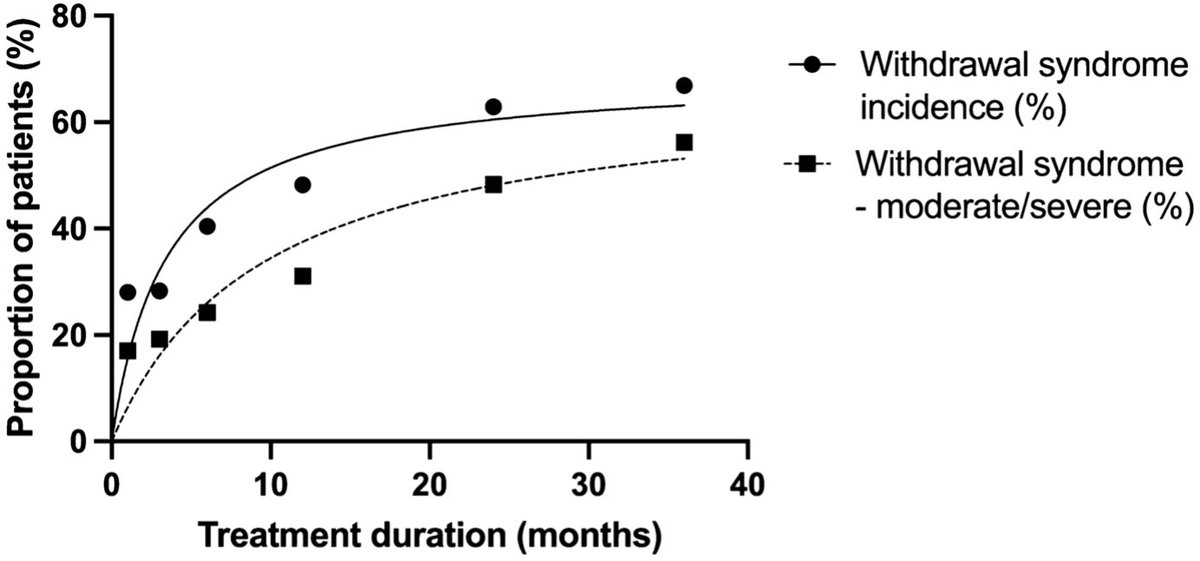
 The Zaccoletti study didn’t examine genuinely slowtapering. It used an old definition (“>4 weeks”), whereas modern guidelines suggest months or years. Only 4 of 76 studies tapered over >12 weeks. (2/n)
The Zaccoletti study didn’t examine genuinely slowtapering. It used an old definition (“>4 weeks”), whereas modern guidelines suggest months or years. Only 4 of 76 studies tapered over >12 weeks. (2/n)

 The main result is based on 11 randomised trials (picture). 6 go for 8 weeks, 4 go for 12 weeks and 1 for 26 weeks. The 26 week study and one of the 12 week studies involve agomelatine, a drug well known not to have much withdrawal effect. So mostly 8-12 week studies. 2/n
The main result is based on 11 randomised trials (picture). 6 go for 8 weeks, 4 go for 12 weeks and 1 for 26 weeks. The 26 week study and one of the 12 week studies involve agomelatine, a drug well known not to have much withdrawal effect. So mostly 8-12 week studies. 2/n

 The majority of published studies are short term studies conducted by the drug manufacturers. This is the same issue that beset the flawed Henssler review. 2/nbit.ly/4033836
The majority of published studies are short term studies conducted by the drug manufacturers. This is the same issue that beset the flawed Henssler review. 2/nbit.ly/4033836

 In a survey of 310 people from NHS therapy services, most of whom said that antidepressants had been helpful to them, 80% reported withdrawal effects. 35% said withdrawal effects were mild, 30% said moderate and 15% said severe. (2/n)
In a survey of 310 people from NHS therapy services, most of whom said that antidepressants had been helpful to them, 80% reported withdrawal effects. 35% said withdrawal effects were mild, 30% said moderate and 15% said severe. (2/n)



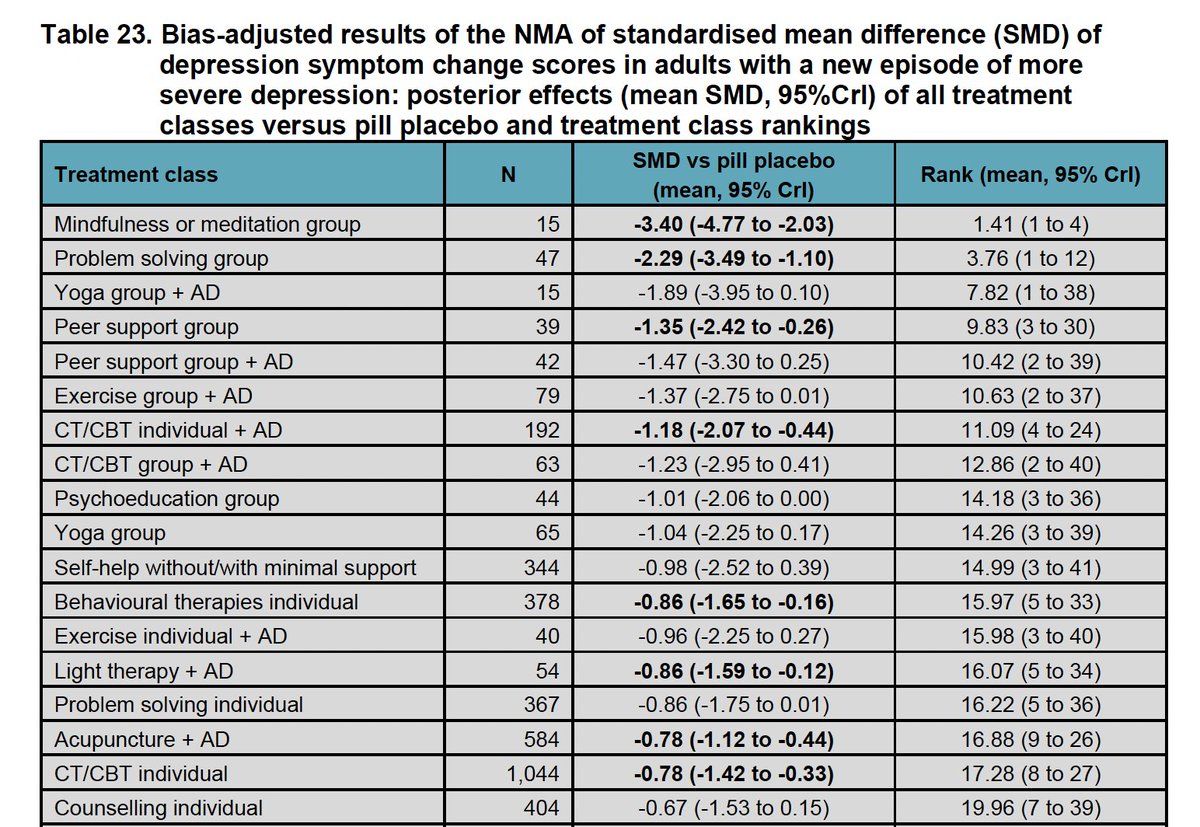
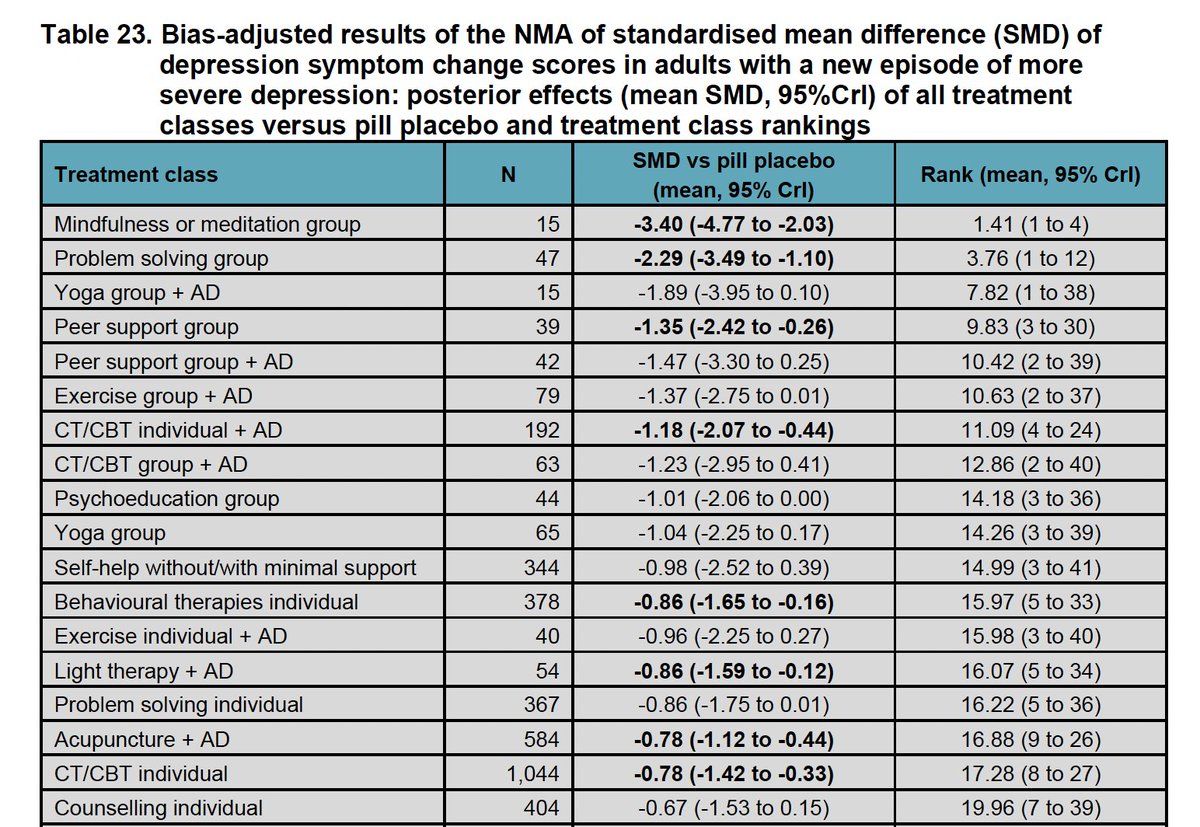 I should emphasise that is for MORE SEVERE depression - the new name for moderate to severe depression. The action on Sunday night is all at Evidence review B: nice.org.uk/guidance/GID-C…
I should emphasise that is for MORE SEVERE depression - the new name for moderate to severe depression. The action on Sunday night is all at Evidence review B: nice.org.uk/guidance/GID-C…
https://twitter.com/ReadReadj/status/1478813245741883407As the comments from GPs in the article reveal the main barrier is access to alternatives which requires investment. Troubling to see that GPs consider ADs mere placebos. Personally I have no issue at all with pbos – I am not shouting down crystal healers 2/n

