#Zentensivist passionate about PH/RV Hemodynamics (esp in Liver Disease & ARDS) | Anti-structural violence | co-EIC https://t.co/uW5ThxyUNk views = mine
How to get URL link on X (Twitter) App



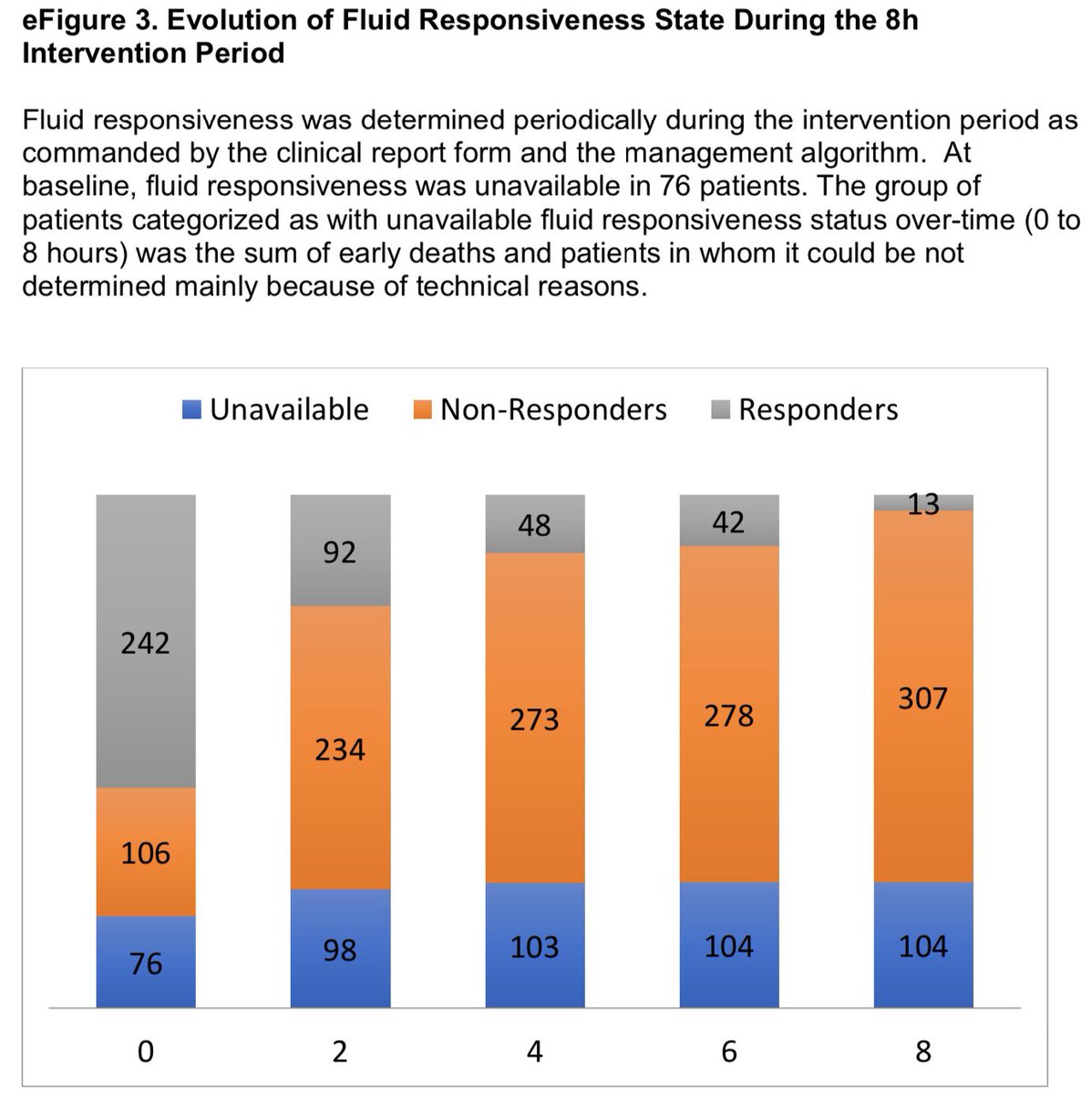
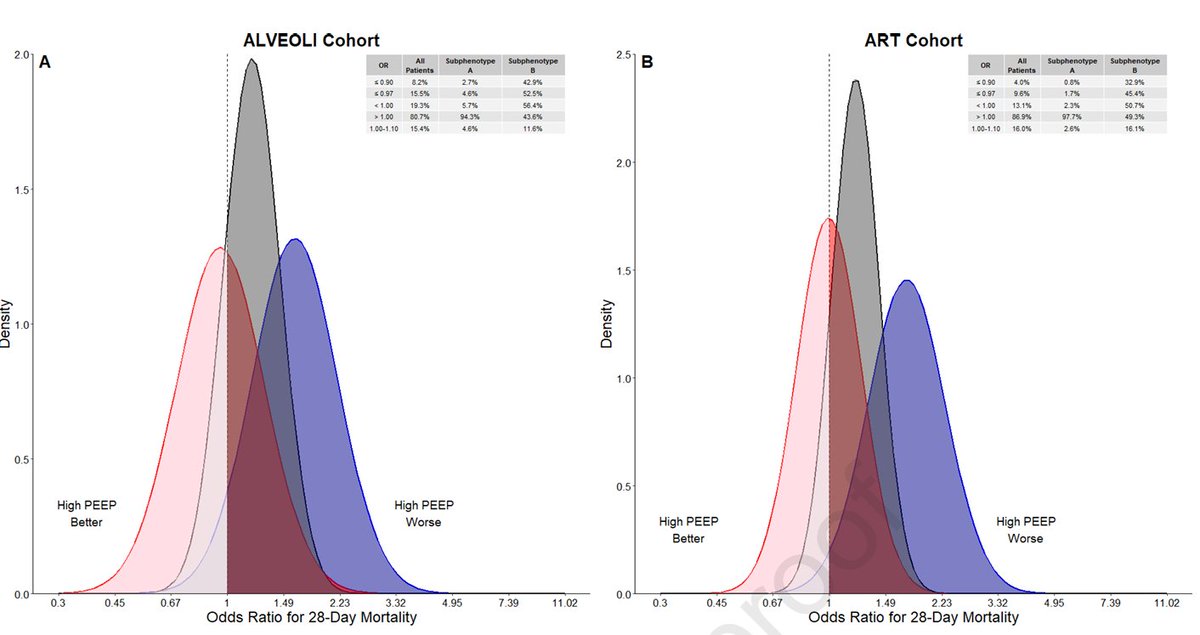 We previously identified two subphenotypes of ARDS using 9 routinely collected clinical variables.
We previously identified two subphenotypes of ARDS using 9 routinely collected clinical variables.


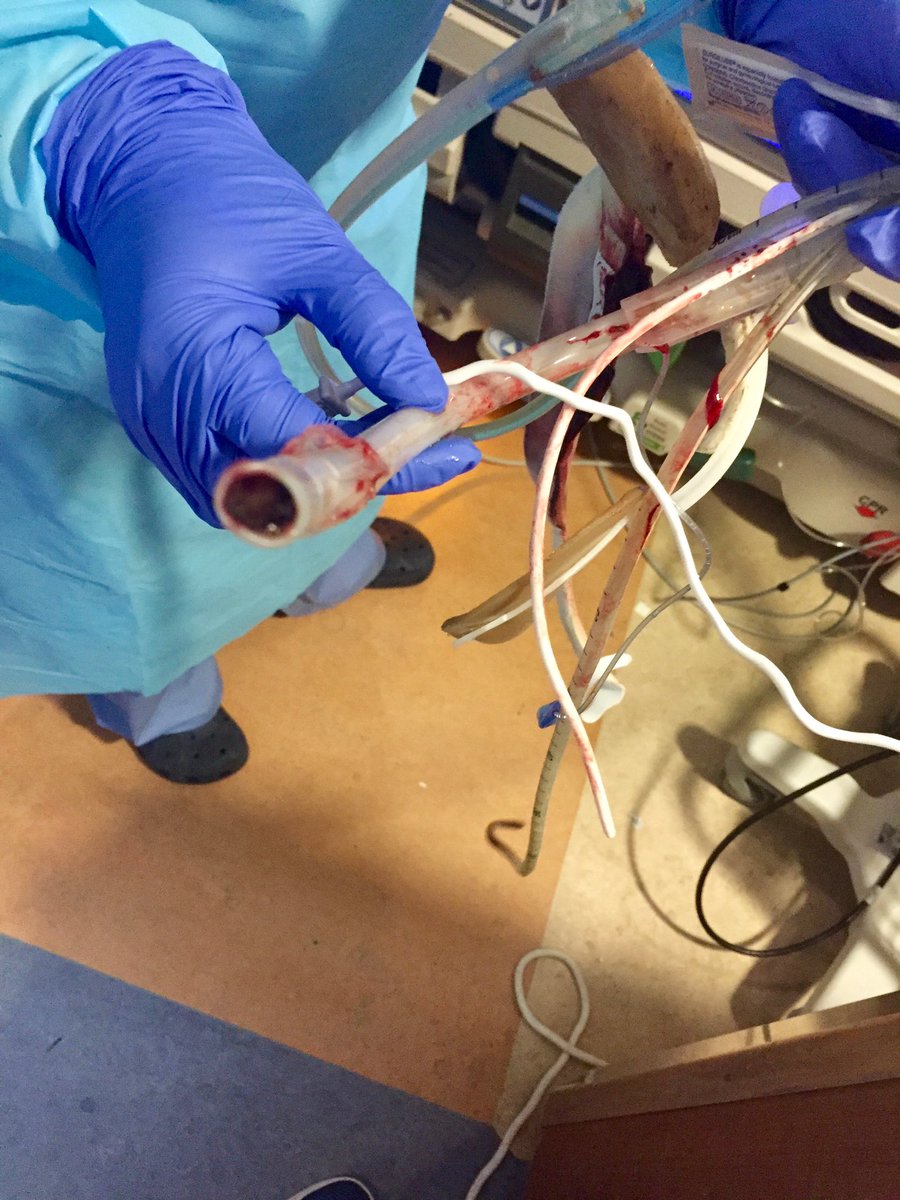
 As a bonus, we compared to quantitative measurement using an ICU monitor and a CVP transducer set. The "peritoneal cavity" here was a saline bag.
As a bonus, we compared to quantitative measurement using an ICU monitor and a CVP transducer set. The "peritoneal cavity" here was a saline bag.


 Oh and btw I’ll give the case conclusion and explanation tomorrow so there’s enough time to accumulate some crowd answers and wisdom!
Oh and btw I’ll give the case conclusion and explanation tomorrow so there’s enough time to accumulate some crowd answers and wisdom!


 A few editorial points:
A few editorial points:
 A few take aways that resonated:
A few take aways that resonated:
 A team member called me to say “We need you at the bedside NOW”, without further details, but with a higher sense of urgency than I’m used to from this person, so I ran to the bedside.
A team member called me to say “We need you at the bedside NOW”, without further details, but with a higher sense of urgency than I’m used to from this person, so I ran to the bedside.
 WOB is moderately elevated.
WOB is moderately elevated.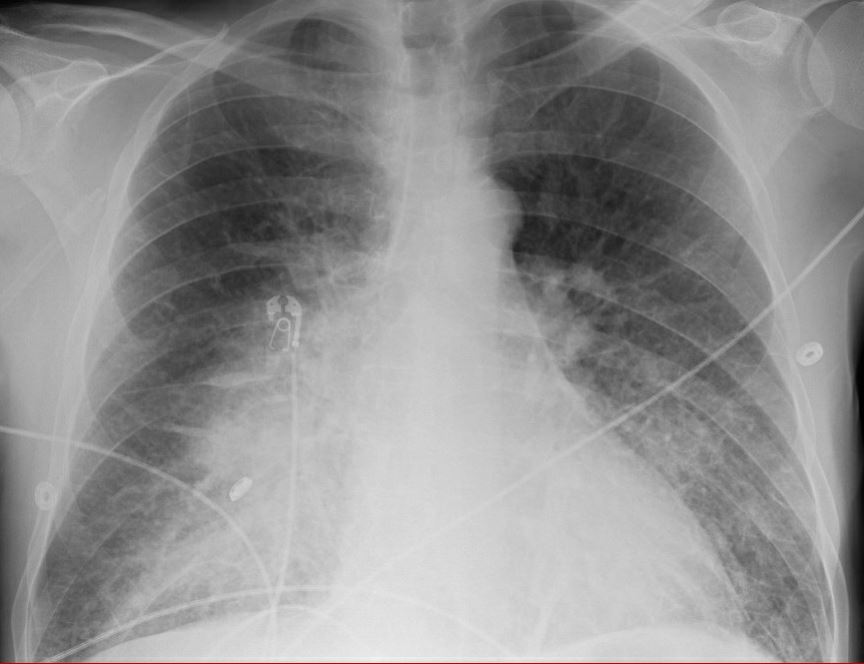
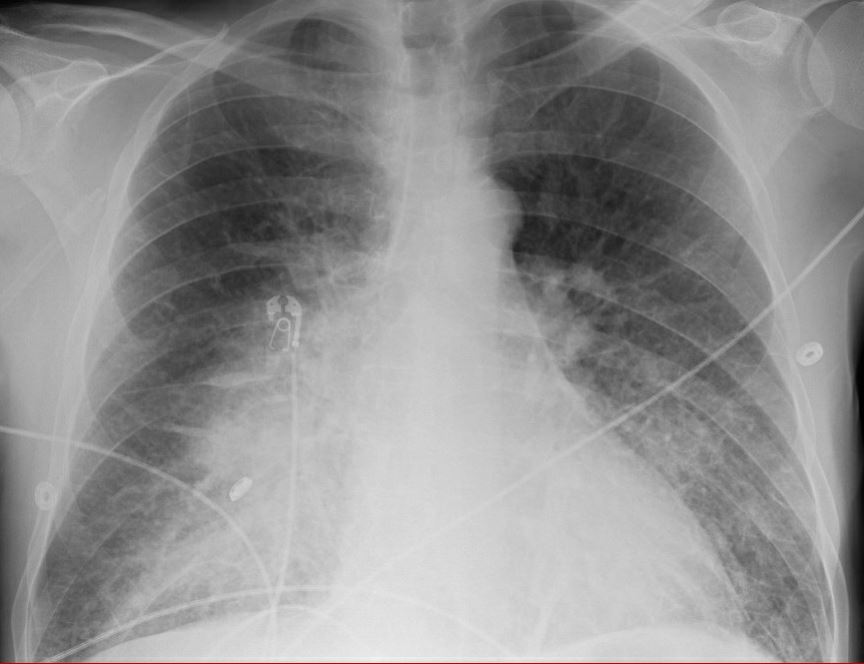 On arrival to the ICU he develops shock requiring vasopressors. Abx staretd. Mottling on knees. What's the next step?
On arrival to the ICU he develops shock requiring vasopressors. Abx staretd. Mottling on knees. What's the next step?


 First step is to examine the flow waveform. In this case a patient in volume control, to observe how passive expiration is changed by changing time constant.
First step is to examine the flow waveform. In this case a patient in volume control, to observe how passive expiration is changed by changing time constant.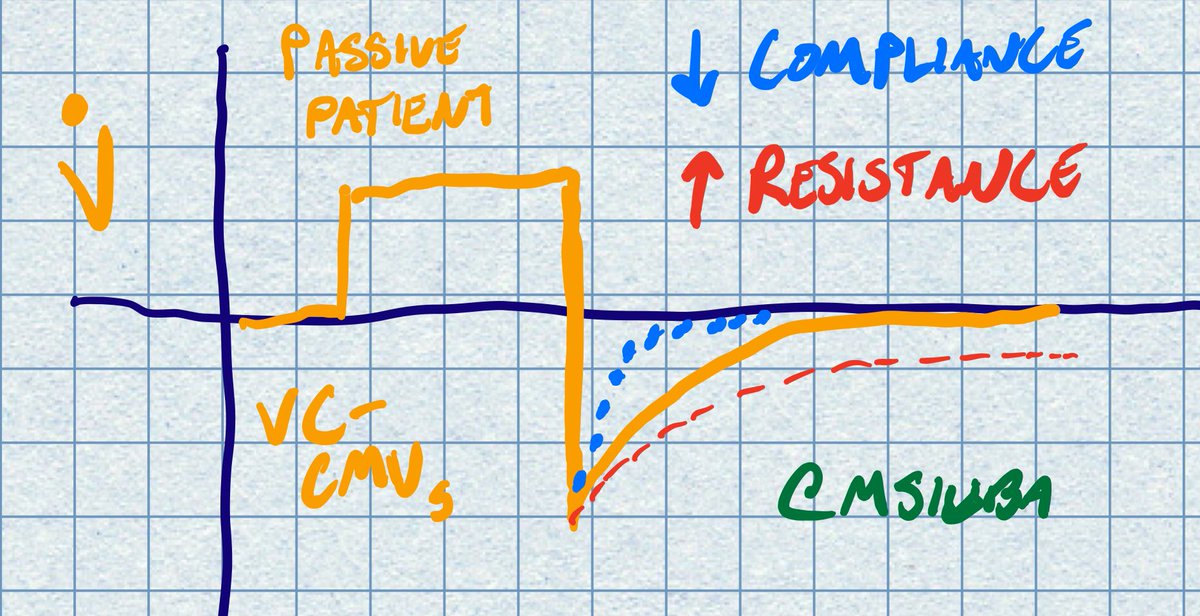

https://twitter.com/msiuba/status/1224514558984933378The most obvious issue here is flow starvation. The patient's effort suggests they want a much higher flow and/or Vt. Compare the waveform to the idealized VC waveform of a passive patient. The flow goes below the PEEP baseline!