1/
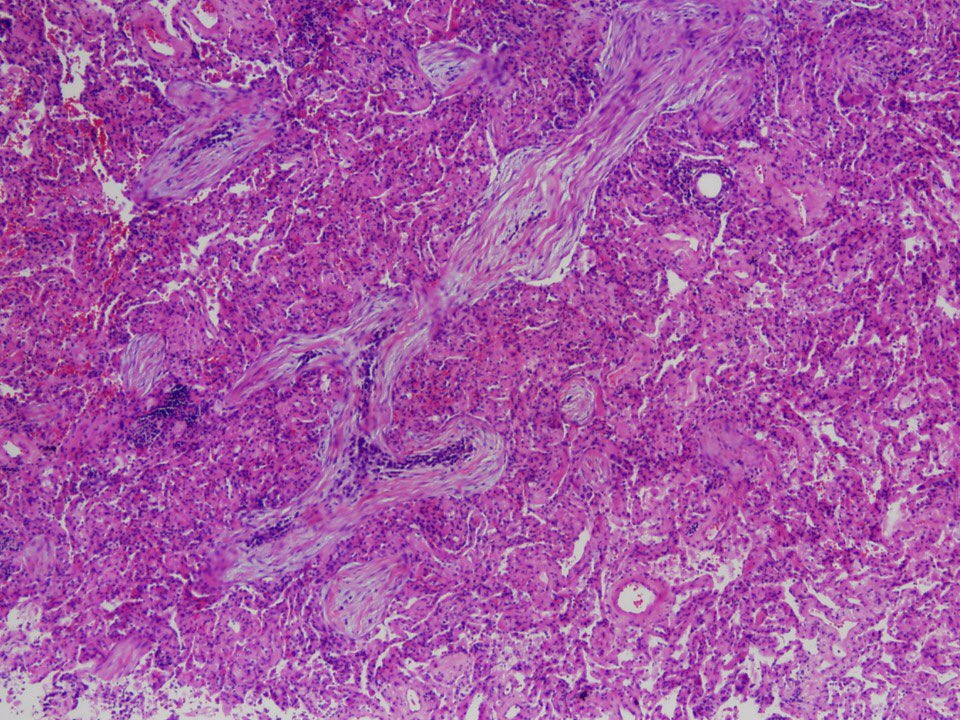
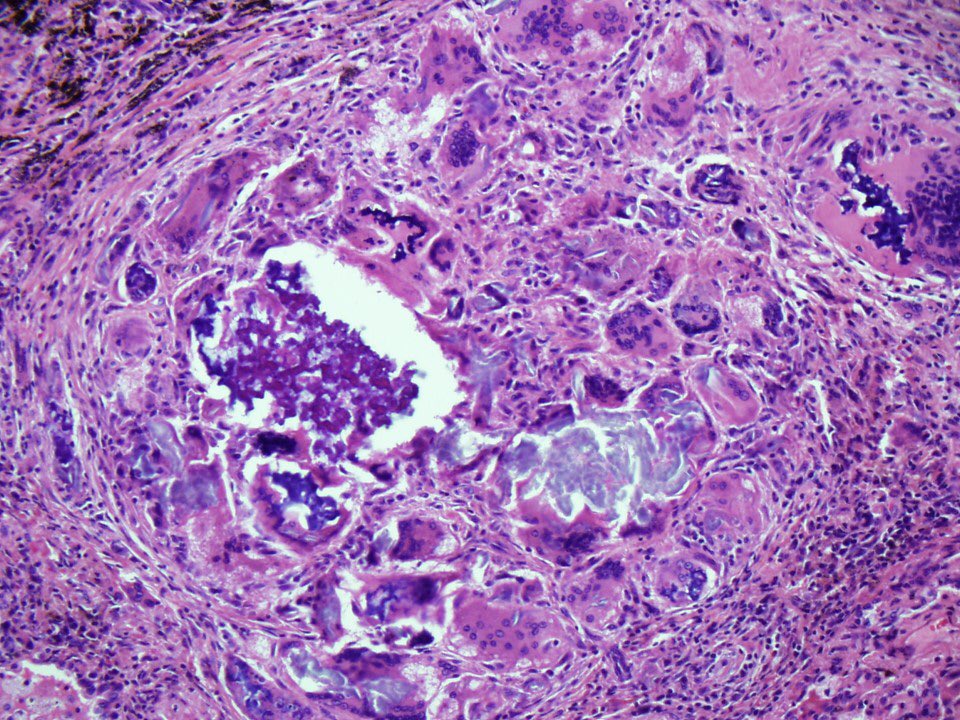
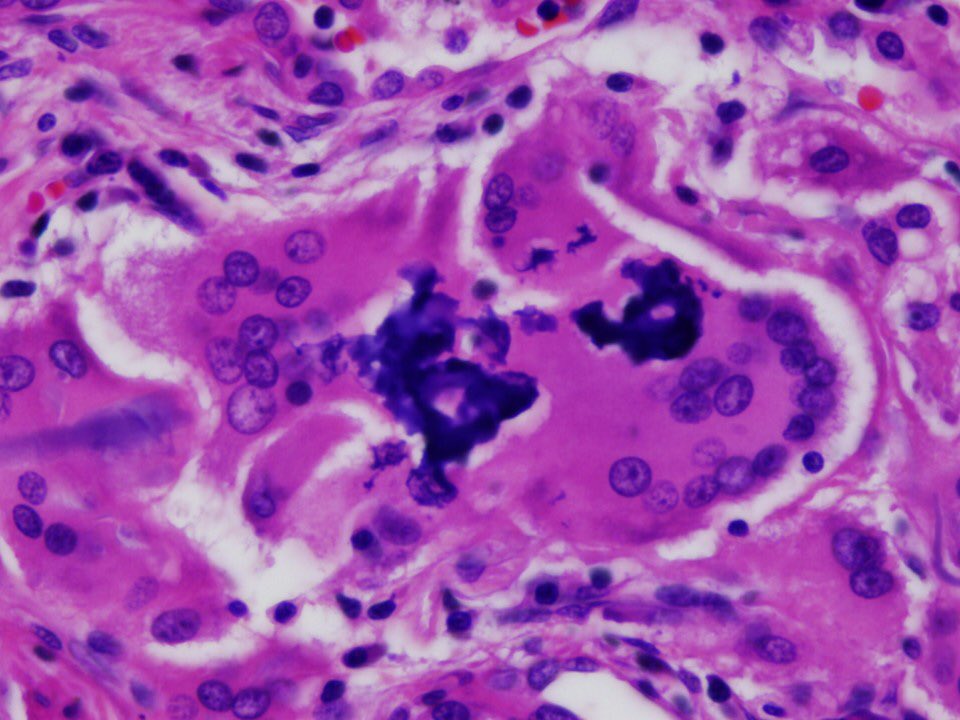
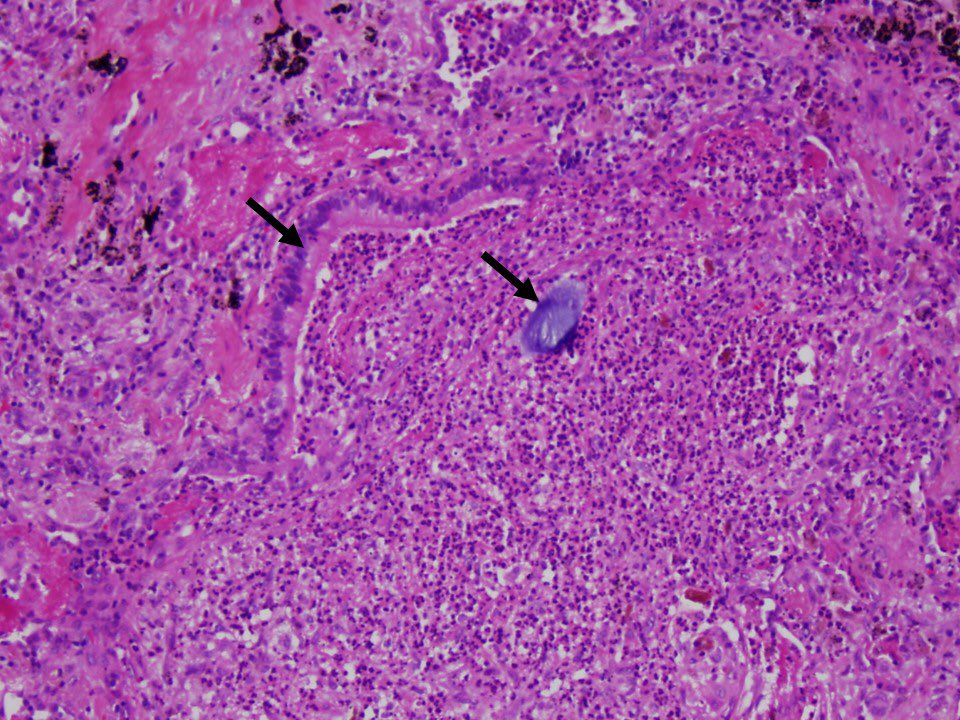
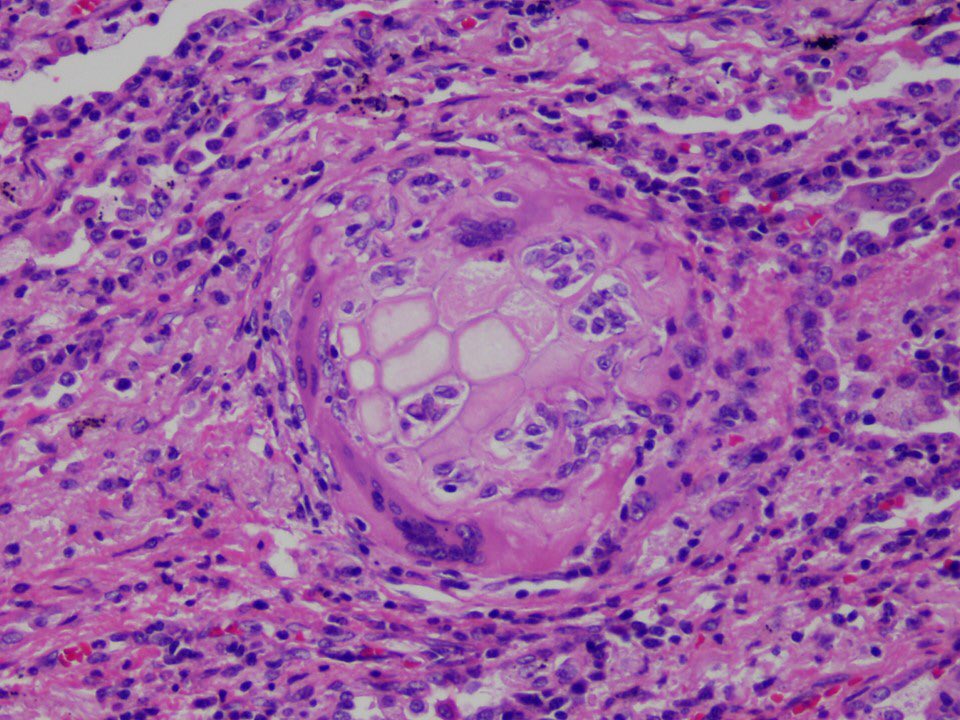
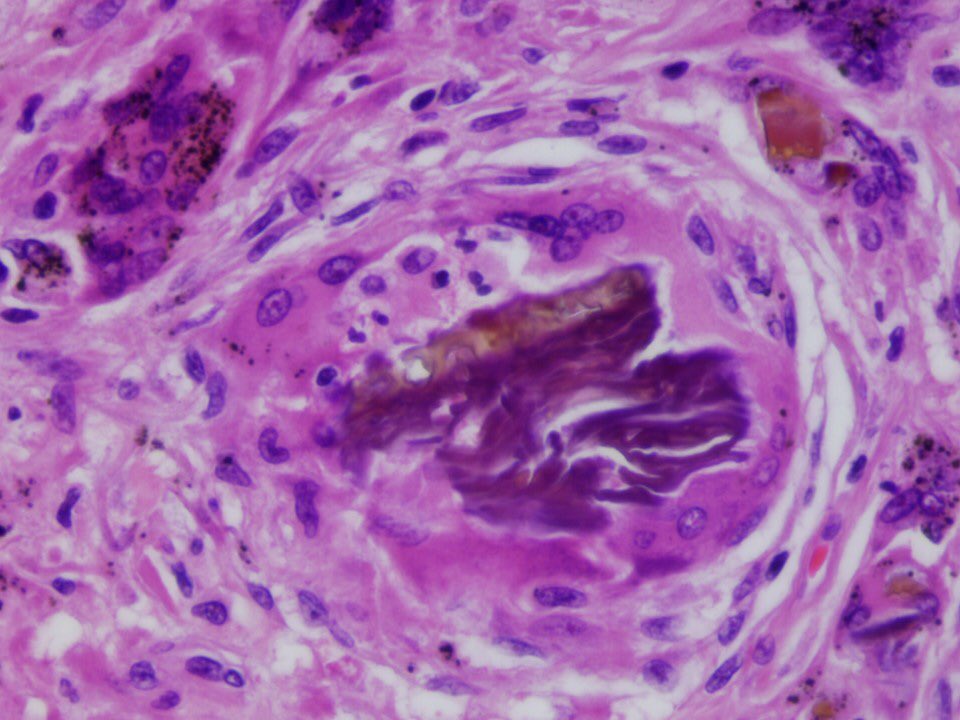
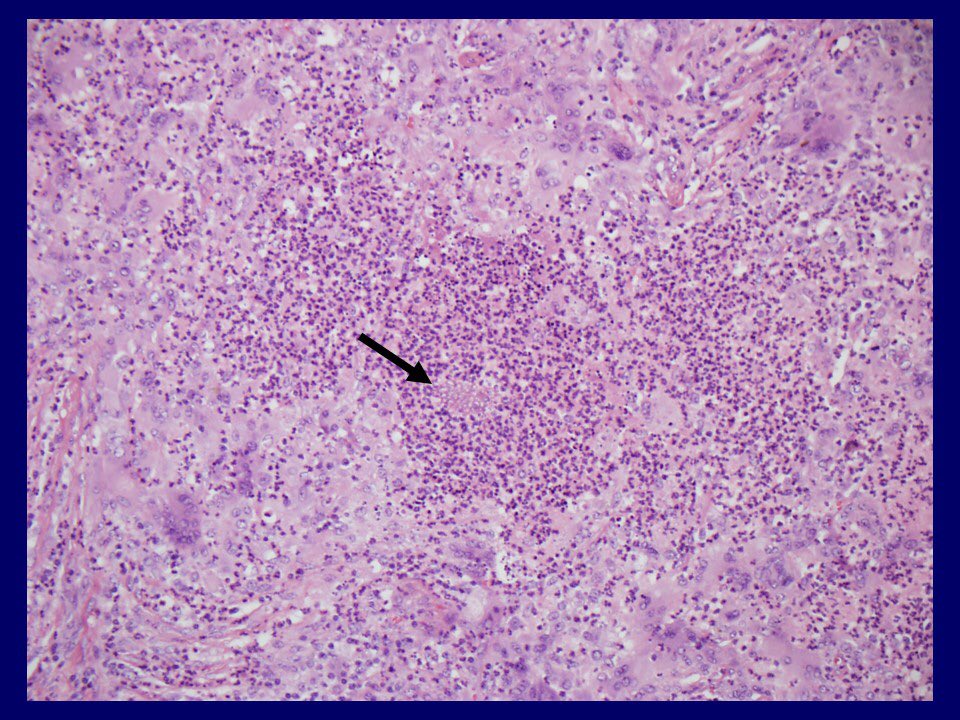
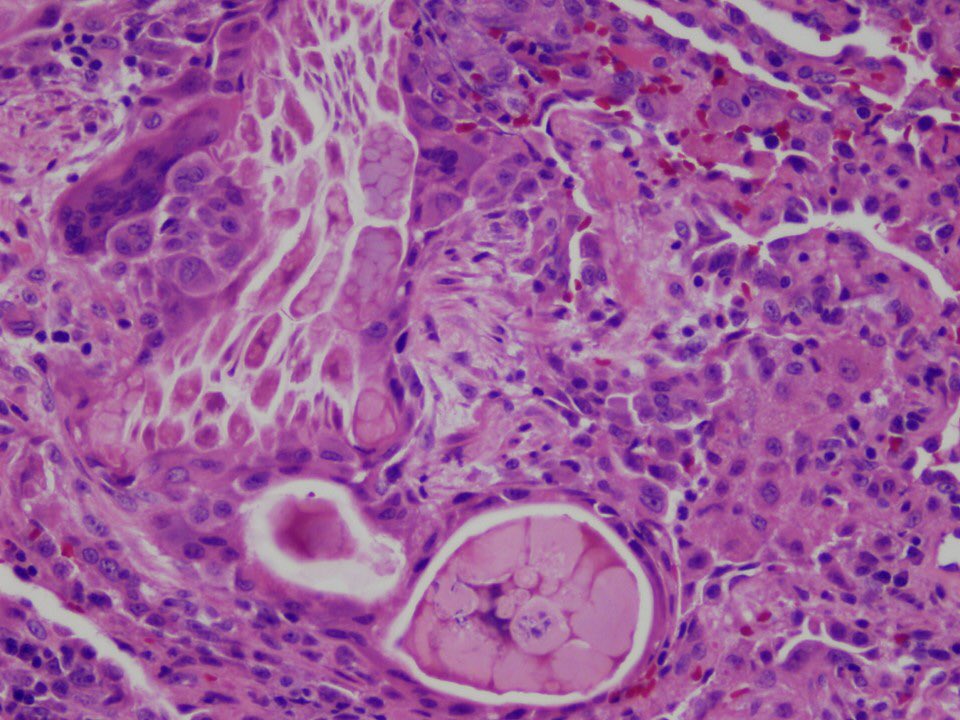
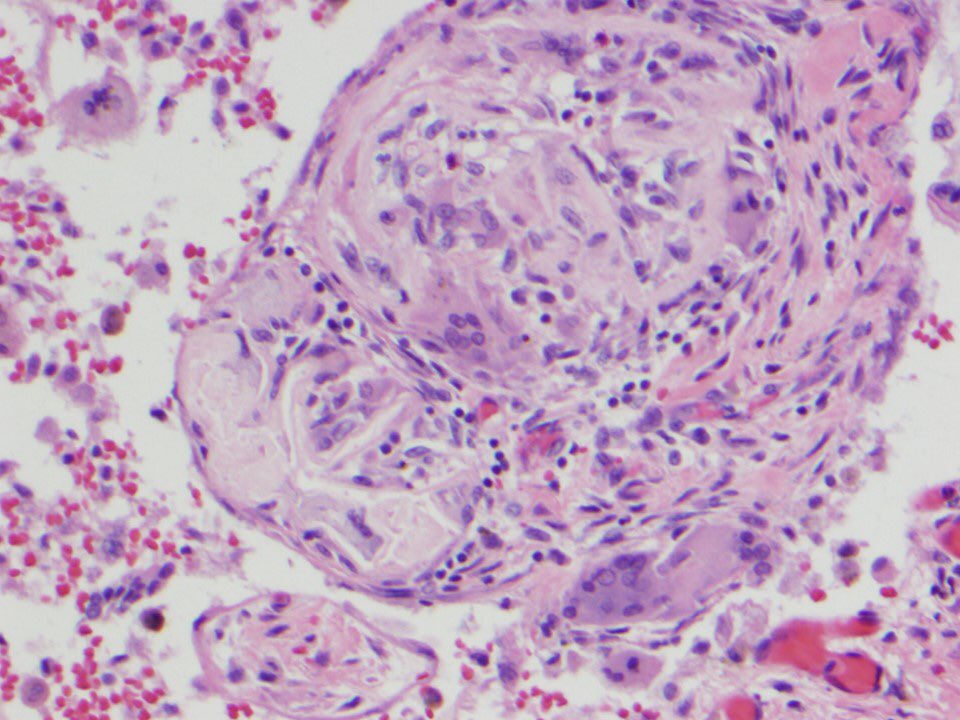
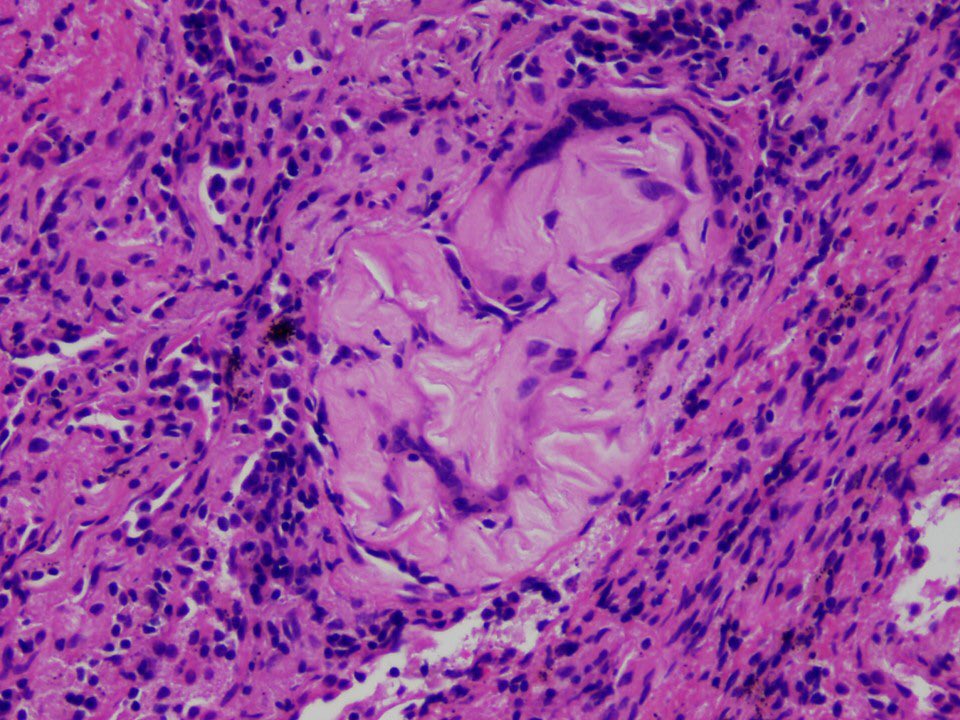
This is the beginning of a #tweetorial or #pathtweetorial on a mystery topic. Fear not, it’ll become evident soon what we’re talking about. But first I’ll show you an image. These serpiginous fibroblast plugs are diagnostic if organizing pneumonia (formerly BOOP)
This is the beginning of a #tweetorial or #pathtweetorial on a mystery topic. Fear not, it’ll become evident soon what we’re talking about. But first I’ll show you an image. These serpiginous fibroblast plugs are diagnostic if organizing pneumonia (formerly BOOP)
2/
In MOST cases of organizing pneumonia seen on lung biopsy, the etiology is not evident on histology. But sometimes, there is a clue. Examine this pic closely and then see if you can answer the quiz in the next tweet in this thread.
In MOST cases of organizing pneumonia seen on lung biopsy, the etiology is not evident on histology. But sometimes, there is a clue. Examine this pic closely and then see if you can answer the quiz in the next tweet in this thread.
3/
What does the pic in the previous tweet show?
What does the pic in the previous tweet show?
4/
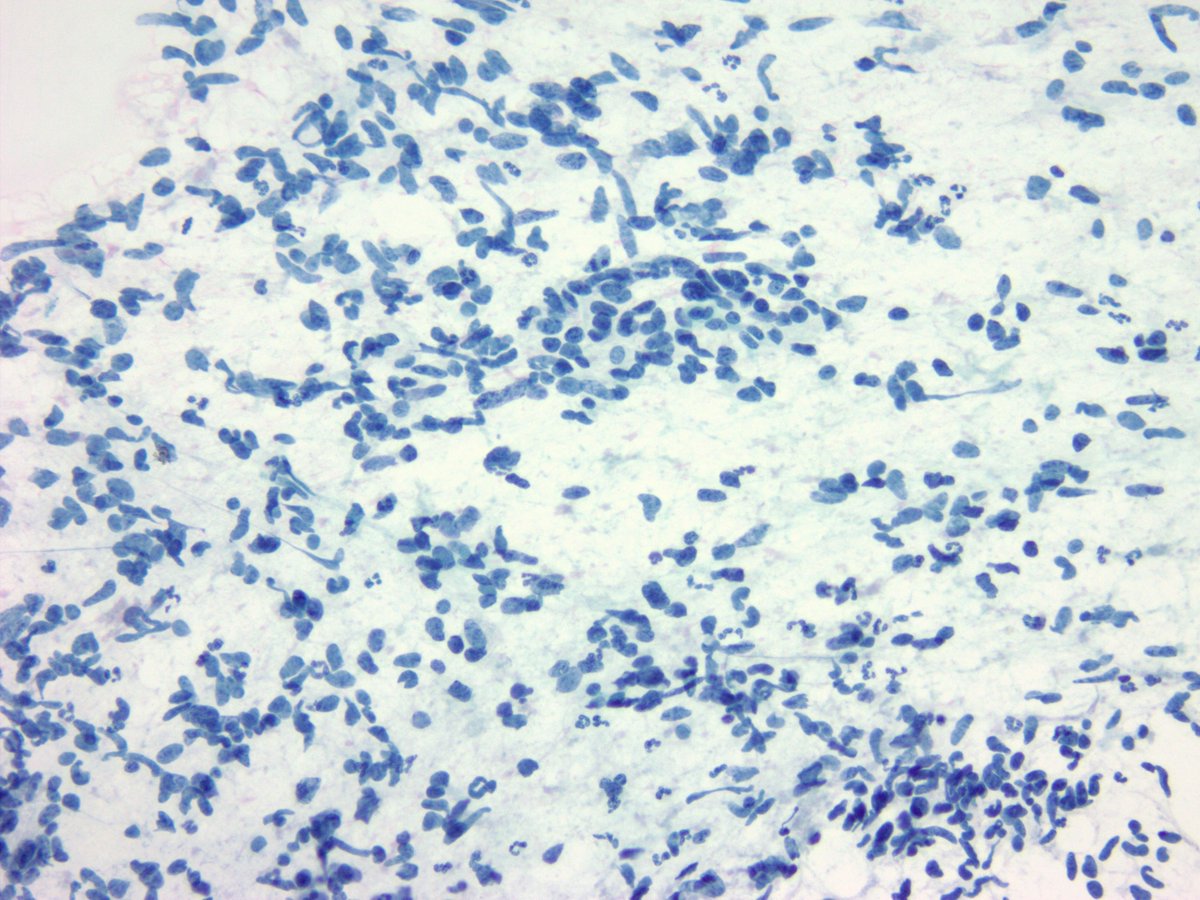
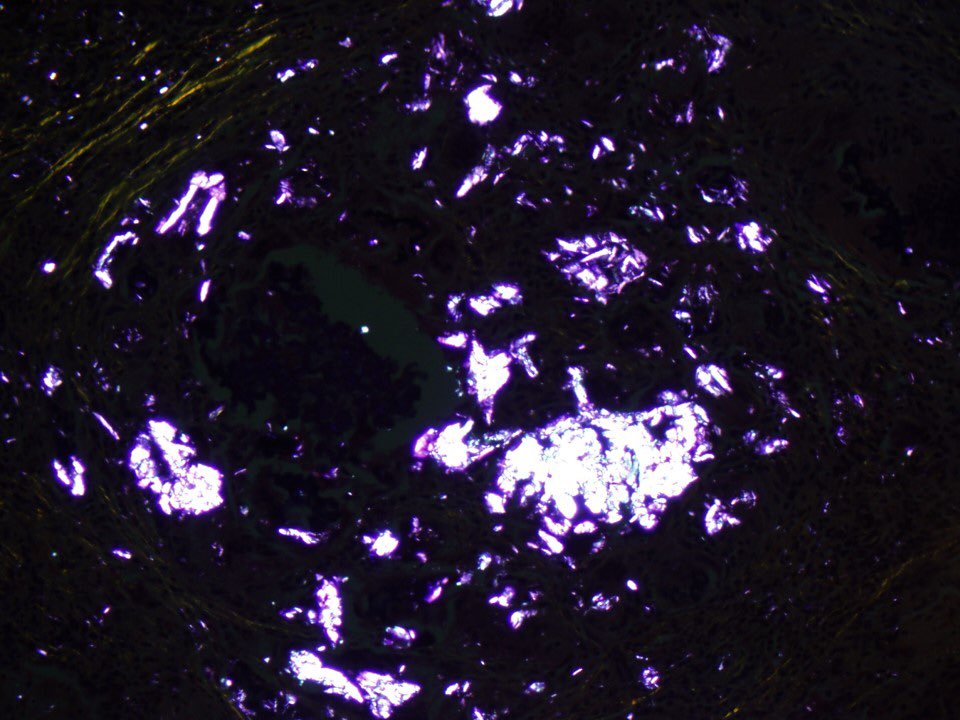
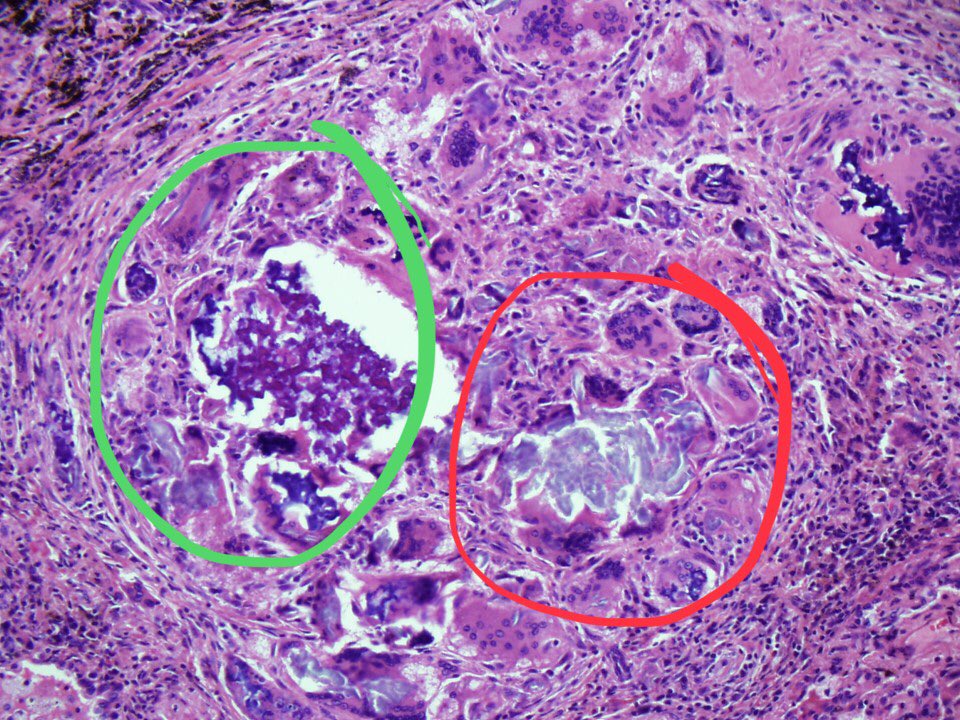
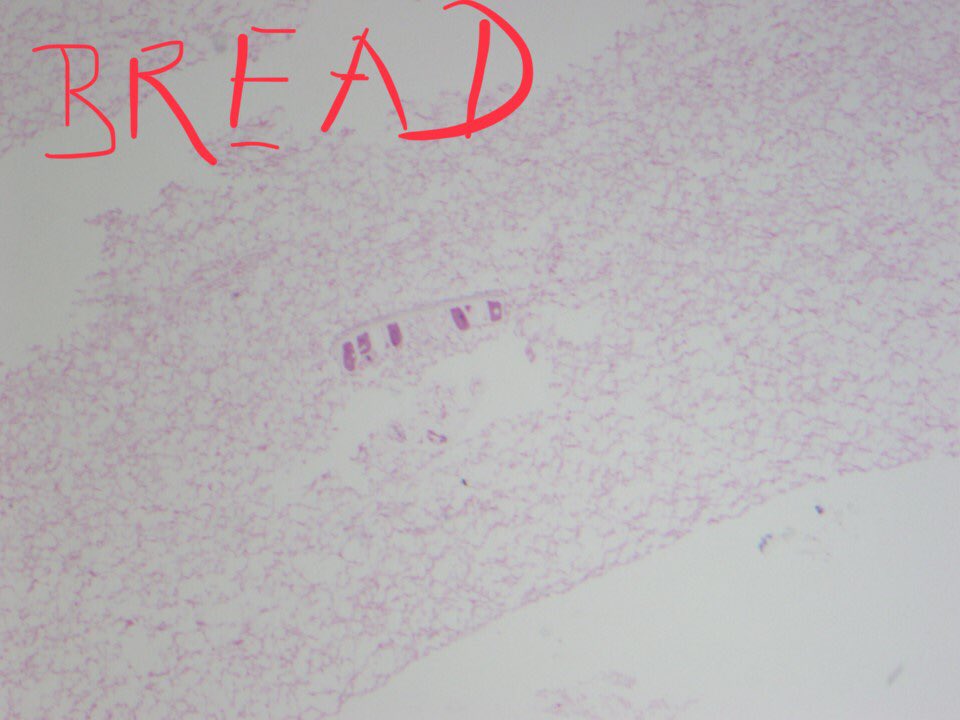
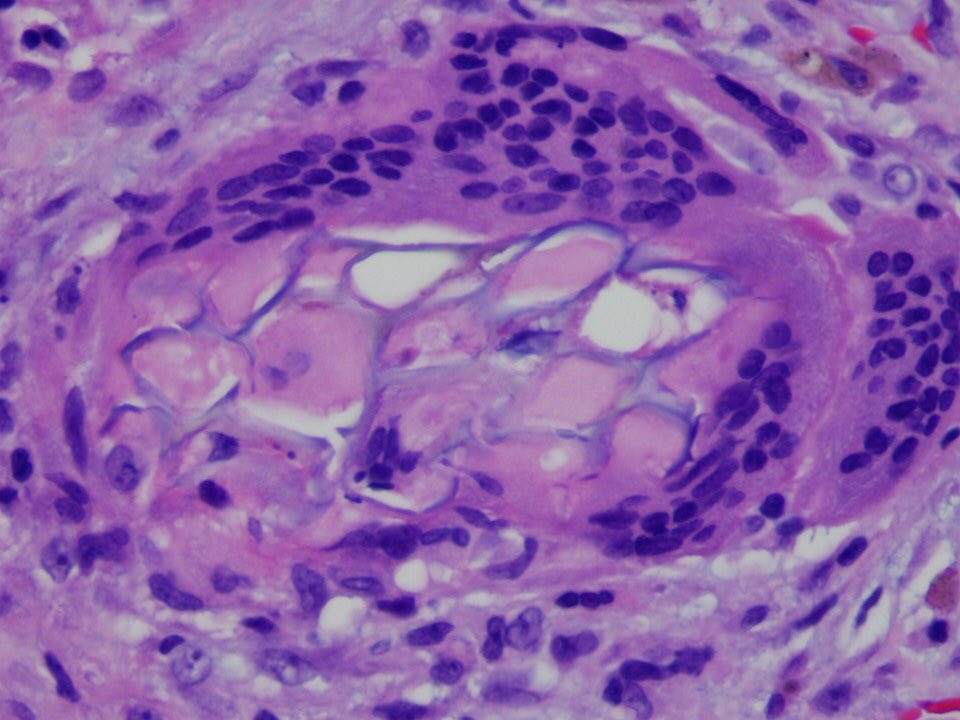
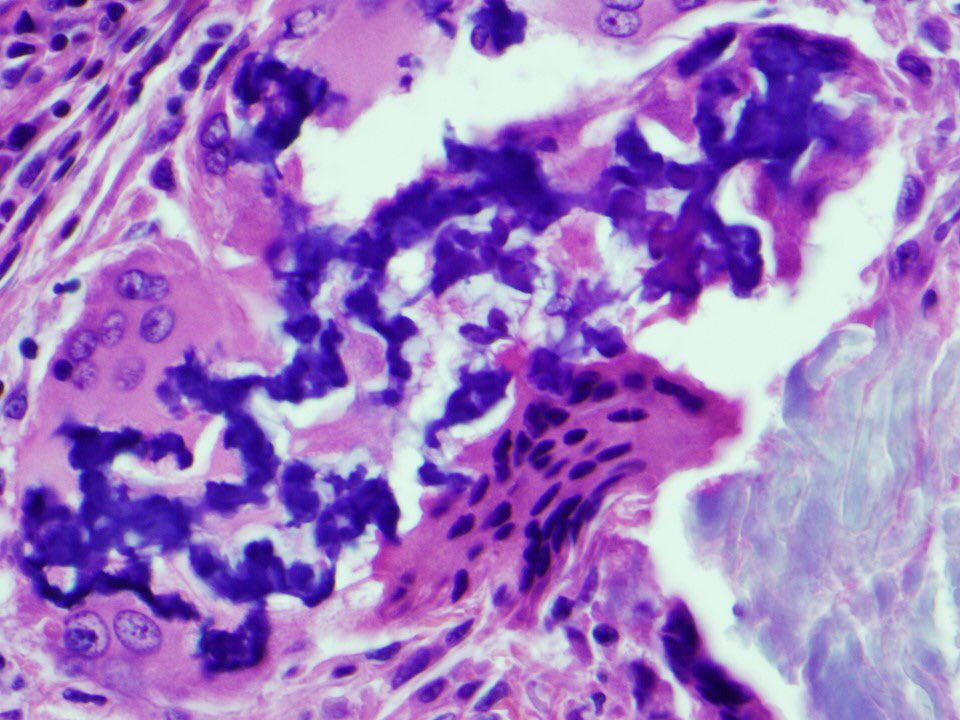
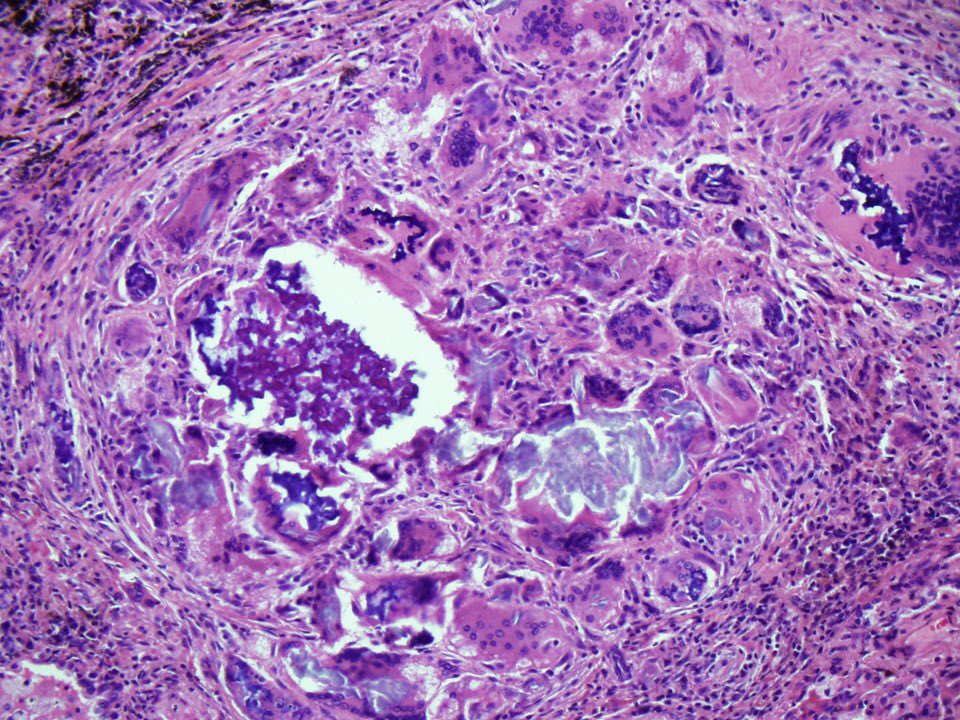
Before I reveal the answer, let me show you what happened when I looked at the same field under polarized light. The particles at bottom right were birefringent but not the ones at top left. Do you know why? #pathology #pulmpath
Before I reveal the answer, let me show you what happened when I looked at the same field under polarized light. The particles at bottom right were birefringent but not the ones at top left. Do you know why? #pathology #pulmpath
5/
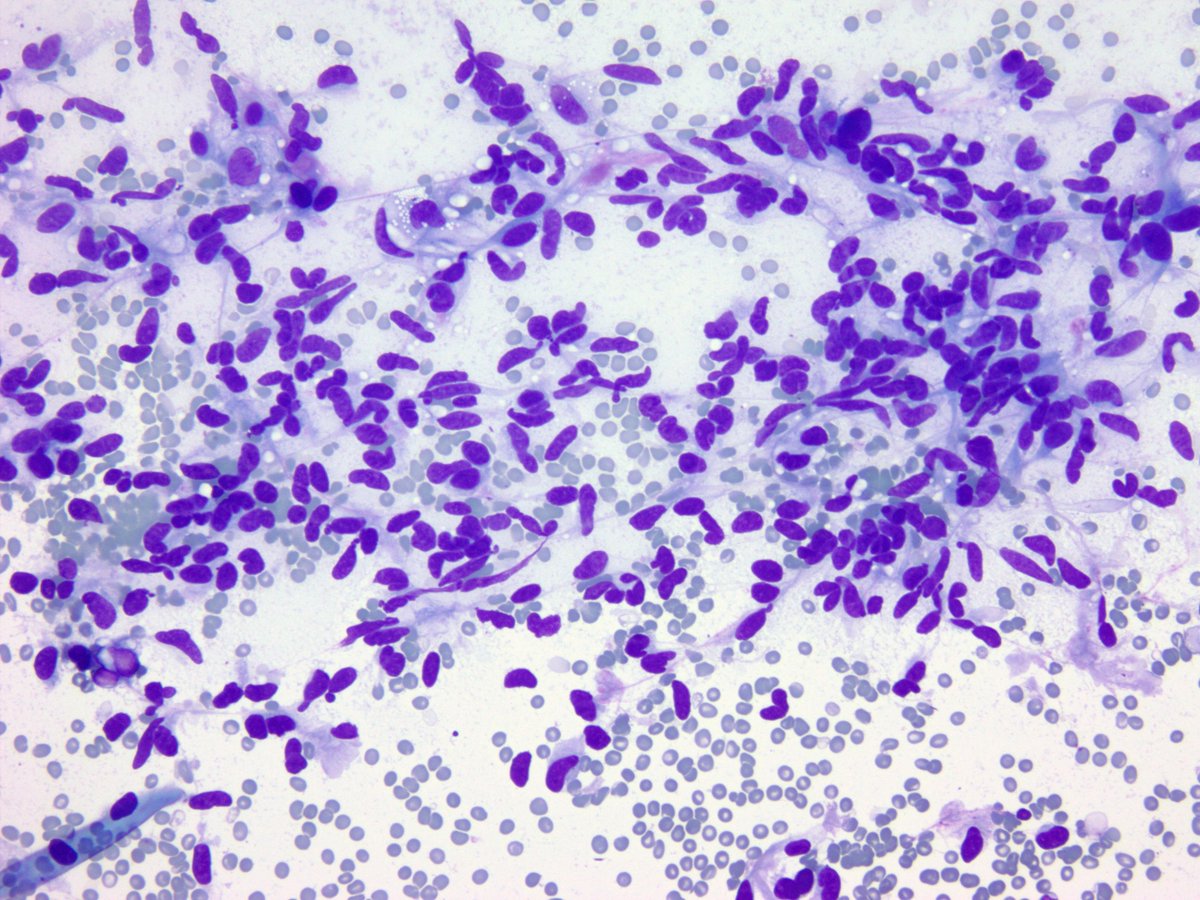
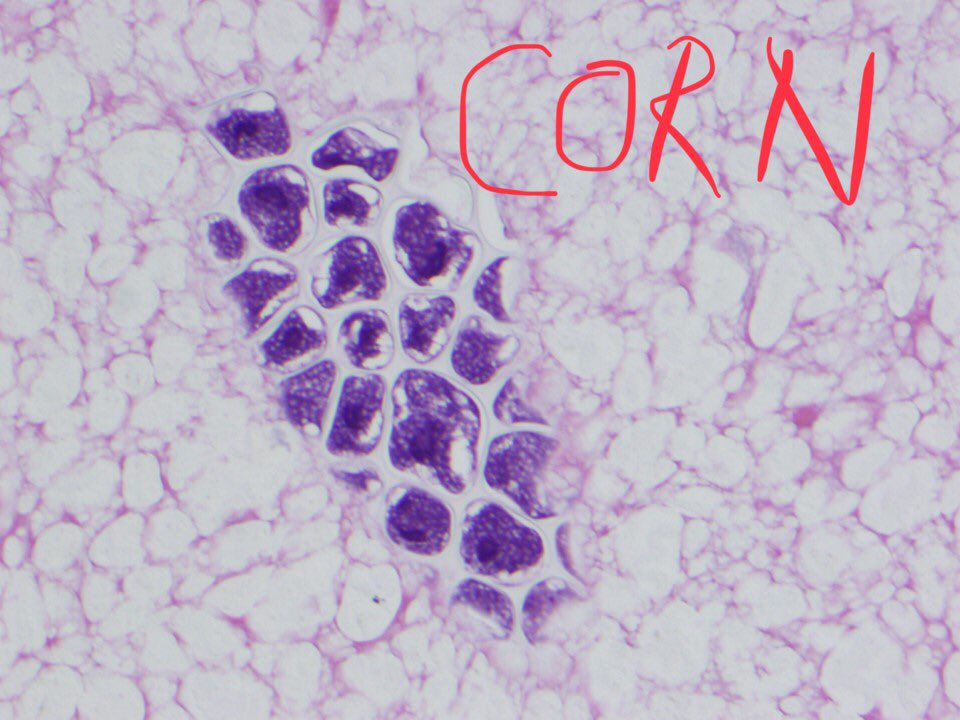
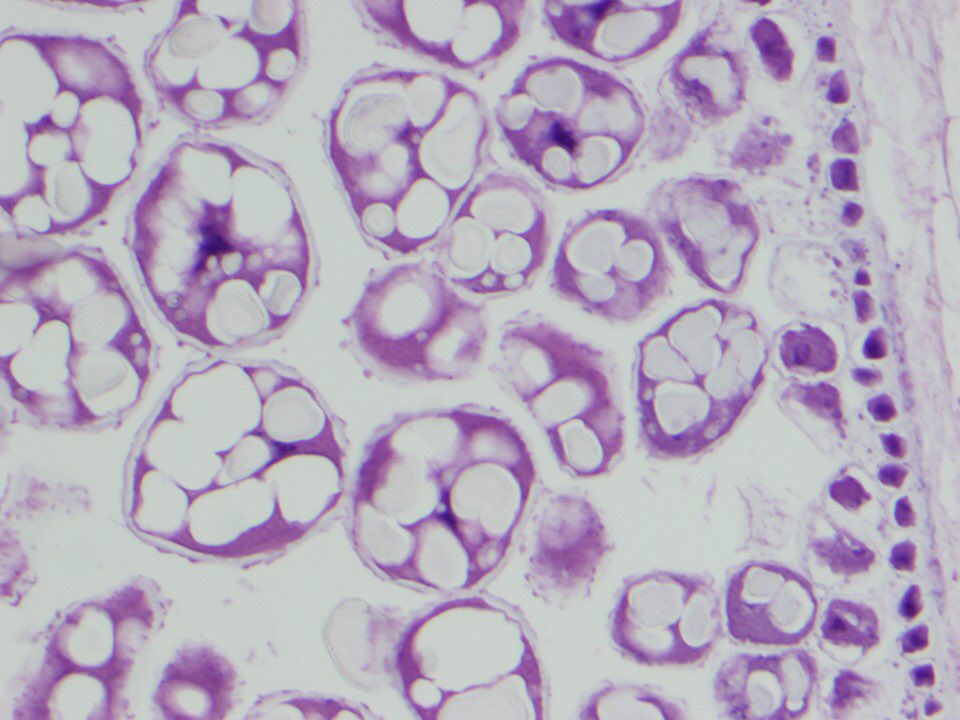
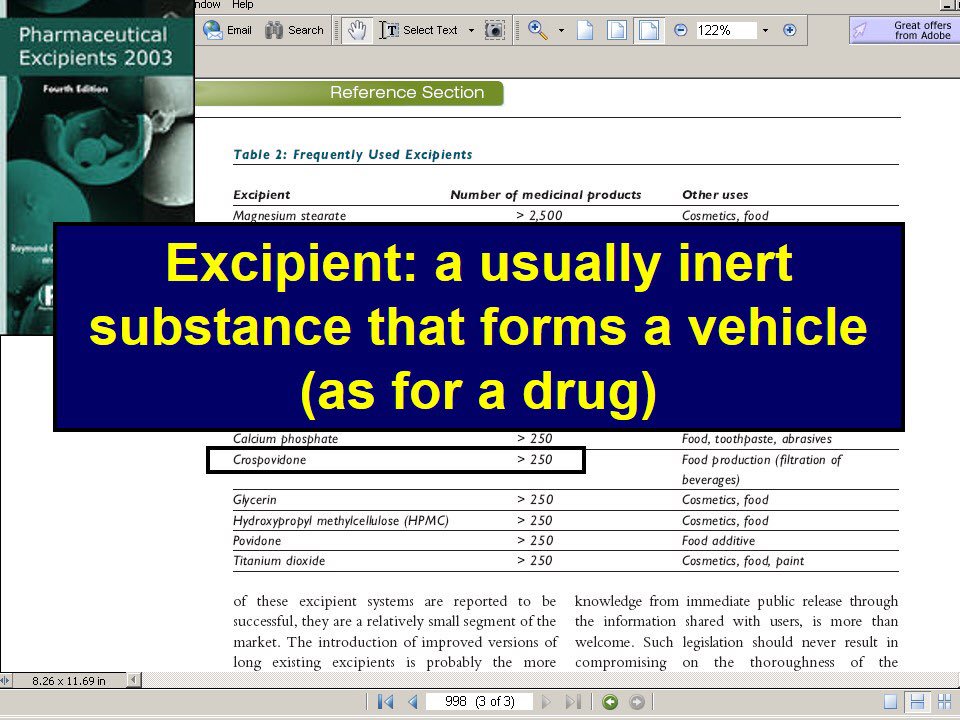
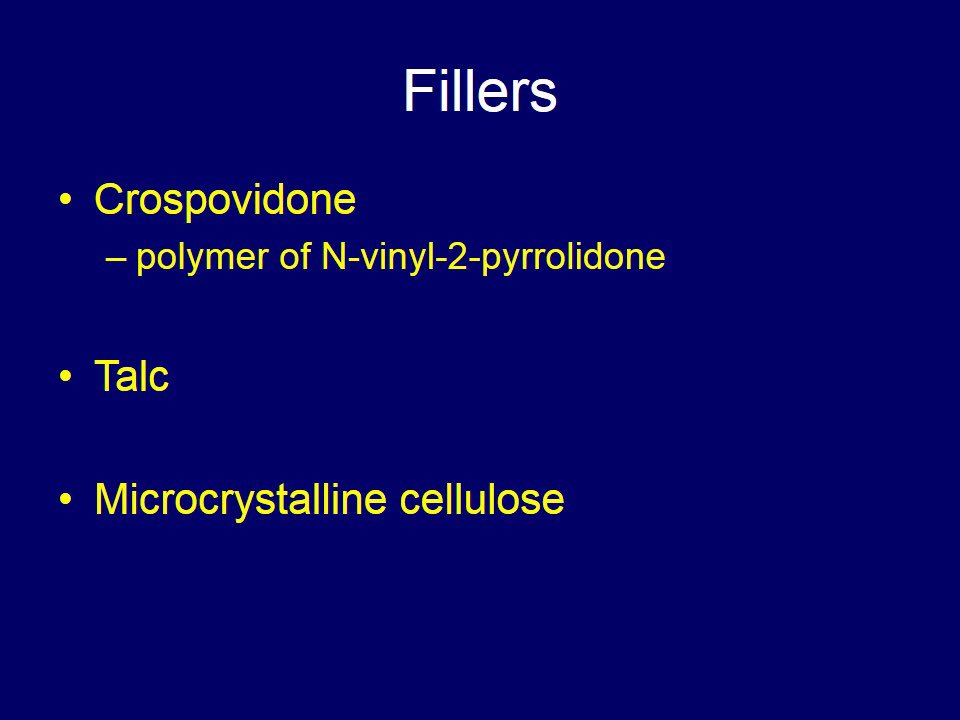
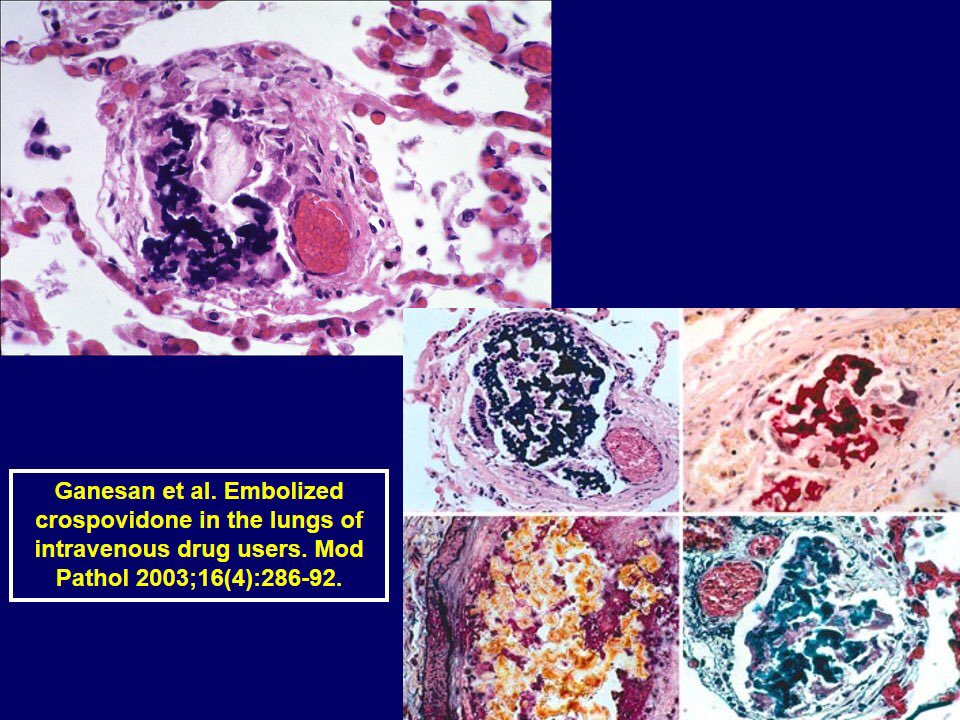
It’s because there are 2 types of pill fillers (excipients) in this image. Microcrystalline cellulose (red circle) and crospovidone (green circle). The former is colorless and brightly birefringent. The latter is purple but not birefringent. Both provide bulk to oral pills.
It’s because there are 2 types of pill fillers (excipients) in this image. Microcrystalline cellulose (red circle) and crospovidone (green circle). The former is colorless and brightly birefringent. The latter is purple but not birefringent. Both provide bulk to oral pills.
6/
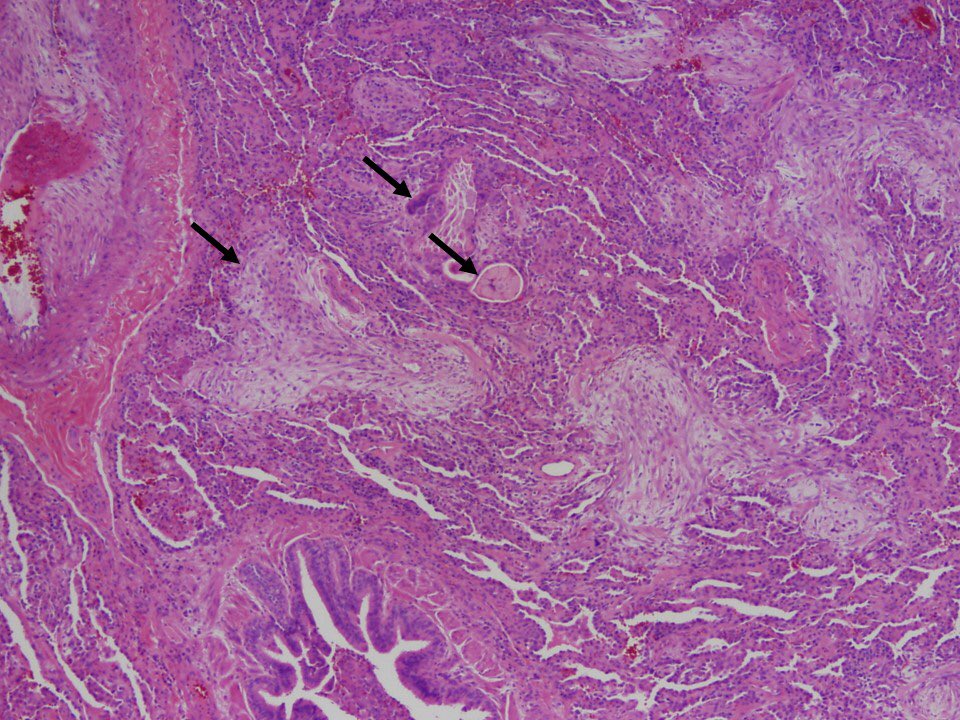
Although pill fillers are most commonly seen in the lung in cases where people infect their pain pills intravenously (talc granulomatosis), this was not the case here. In this case, the pills were aspirated into the lung. This is “particulate matter aspiration”
Although pill fillers are most commonly seen in the lung in cases where people infect their pain pills intravenously (talc granulomatosis), this was not the case here. In this case, the pills were aspirated into the lung. This is “particulate matter aspiration”
7/
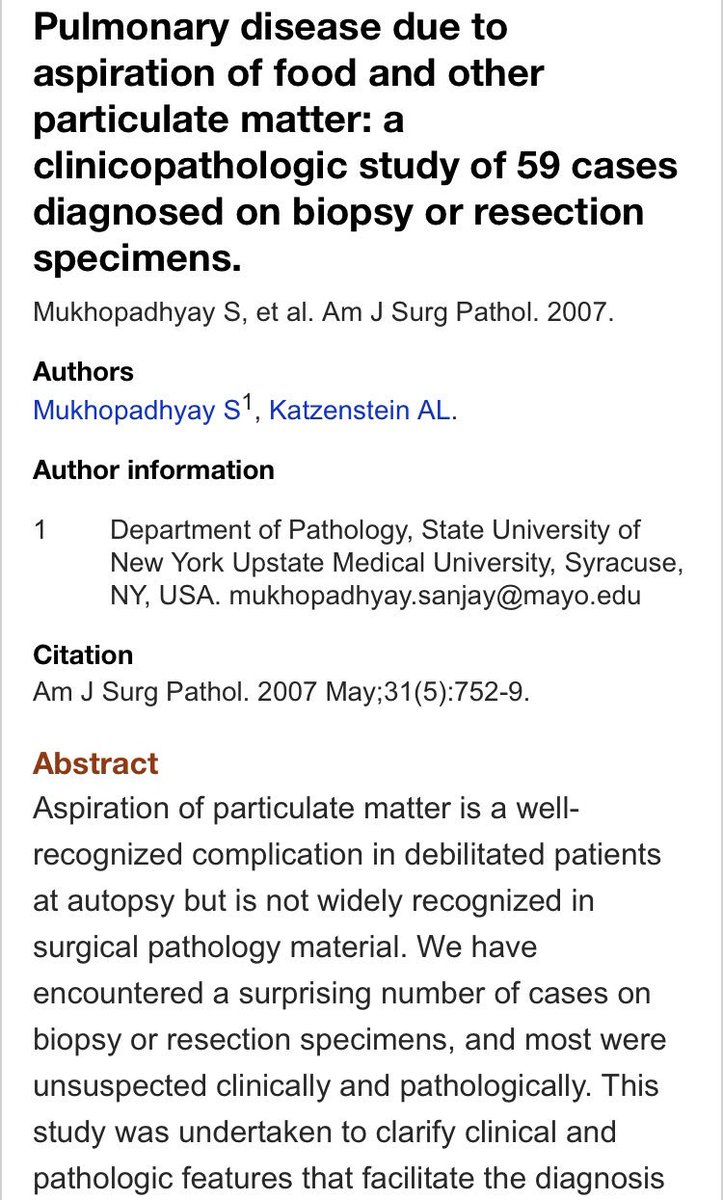
Several years ago, I did a study on cases like this diagnosed on lung biopsies by Dr. Katzenstein. It taught me a lot about the power of pathology as a diagnostic tool in some situations where clinical features and imaging can be VERY misleading.
ncbi.nlm.nih.gov/pubmed/1746046…
Several years ago, I did a study on cases like this diagnosed on lung biopsies by Dr. Katzenstein. It taught me a lot about the power of pathology as a diagnostic tool in some situations where clinical features and imaging can be VERY misleading.
ncbi.nlm.nih.gov/pubmed/1746046…
8/
This is NOT the aspiration pneumonia you learn about in medical school or as a pulmonologist or ID doc.
These are not debilitated patients with GERD and a dilated esophagus, right lower lobe infiltrates and aspiration of oral flora into the lung. ❌
This is different...
This is NOT the aspiration pneumonia you learn about in medical school or as a pulmonologist or ID doc.
These are not debilitated patients with GERD and a dilated esophagus, right lower lobe infiltrates and aspiration of oral flora into the lung. ❌
This is different...
9/
An important difference is that this involves aspiration of MICROSCOPIC particles (presumably from gastric contents), not bacteria from the mouth.
Also, this is not the same as finding a peanut in a bronchus. Completely different sequence of events. See next tweet...
An important difference is that this involves aspiration of MICROSCOPIC particles (presumably from gastric contents), not bacteria from the mouth.
Also, this is not the same as finding a peanut in a bronchus. Completely different sequence of events. See next tweet...

10/
What are these aspirated particles that can show up in lung biopsies?
1. Vegetable particles
2. Meat particles (rare)
3. Pill fillers (rare)
4. Kayexalate (rare)
Meat (skeletal muscle) can be seen at autopsy but gets rapidly destroyed so is seldom seen in biopsies.
What are these aspirated particles that can show up in lung biopsies?
1. Vegetable particles
2. Meat particles (rare)
3. Pill fillers (rare)
4. Kayexalate (rare)
Meat (skeletal muscle) can be seen at autopsy but gets rapidly destroyed so is seldom seen in biopsies.
11/
When these particles enter the lung, this is the inflammatory sequence:
1. Acute bronchopneumonia and acute bronchiolitis (neutrophils) ➡️ EARLY
2. Organizing pneumonia
3. Foreign body giant cells and granulomas ➡️ late
The late changes are the most challenging...
When these particles enter the lung, this is the inflammatory sequence:
1. Acute bronchopneumonia and acute bronchiolitis (neutrophils) ➡️ EARLY
2. Organizing pneumonia
3. Foreign body giant cells and granulomas ➡️ late
The late changes are the most challenging...
12/
The imaging starts to get weird and deviates from standard descriptions of aspiration. You get:
1. Tree in bud opacities (reflects bronchiolitis)
2. Nodules
3. Opacities in any lobe (people aspirate when laying down)
4. Recurrent infiltrates or “recurrent pneumonia”
The imaging starts to get weird and deviates from standard descriptions of aspiration. You get:
1. Tree in bud opacities (reflects bronchiolitis)
2. Nodules
3. Opacities in any lobe (people aspirate when laying down)
4. Recurrent infiltrates or “recurrent pneumonia”
13/
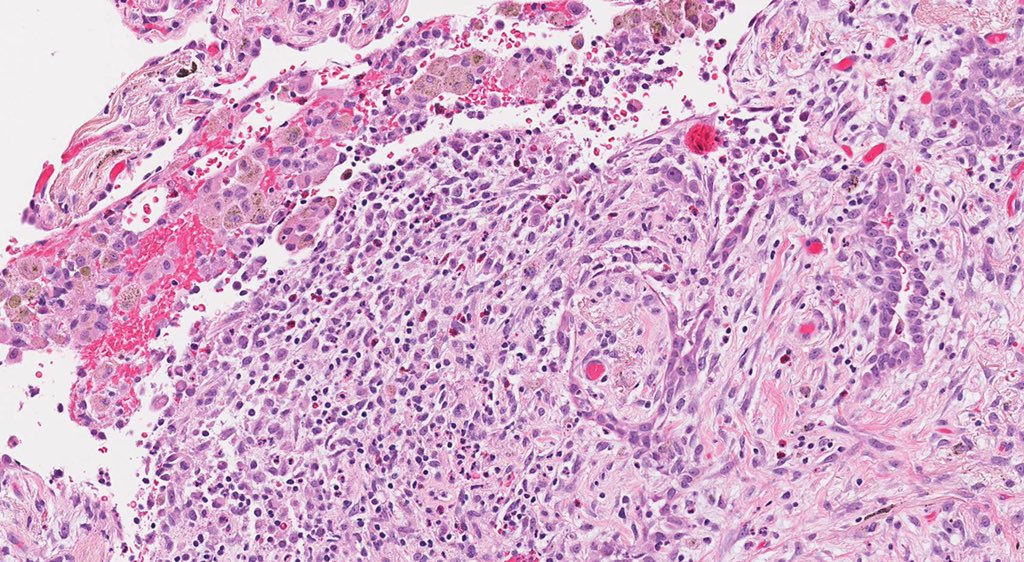
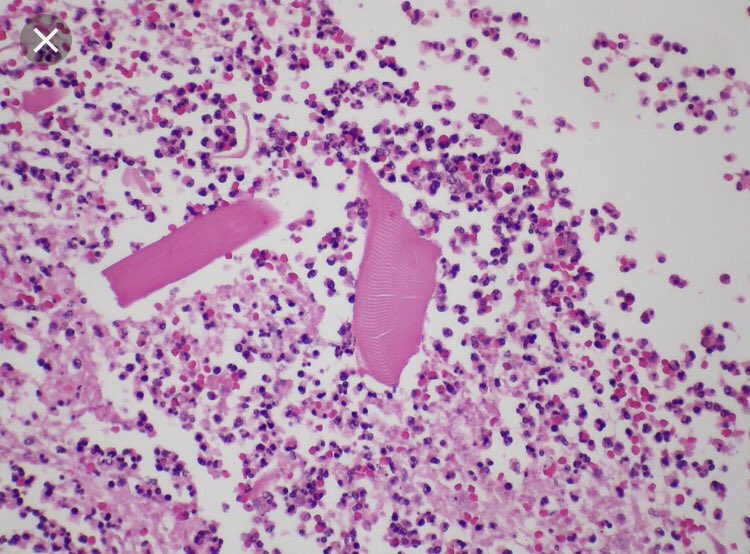
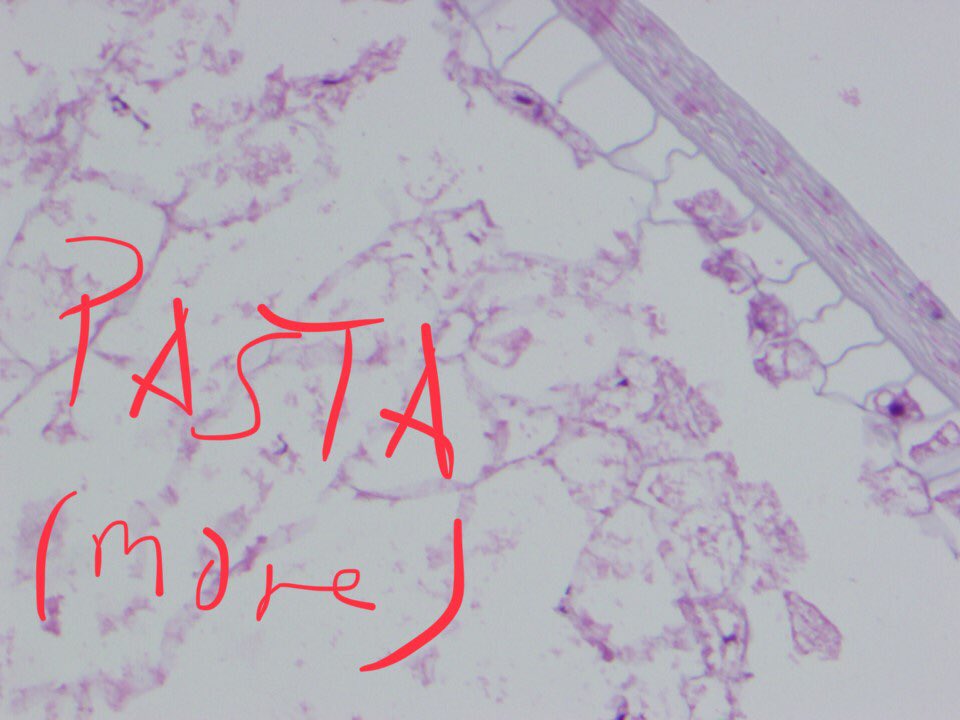
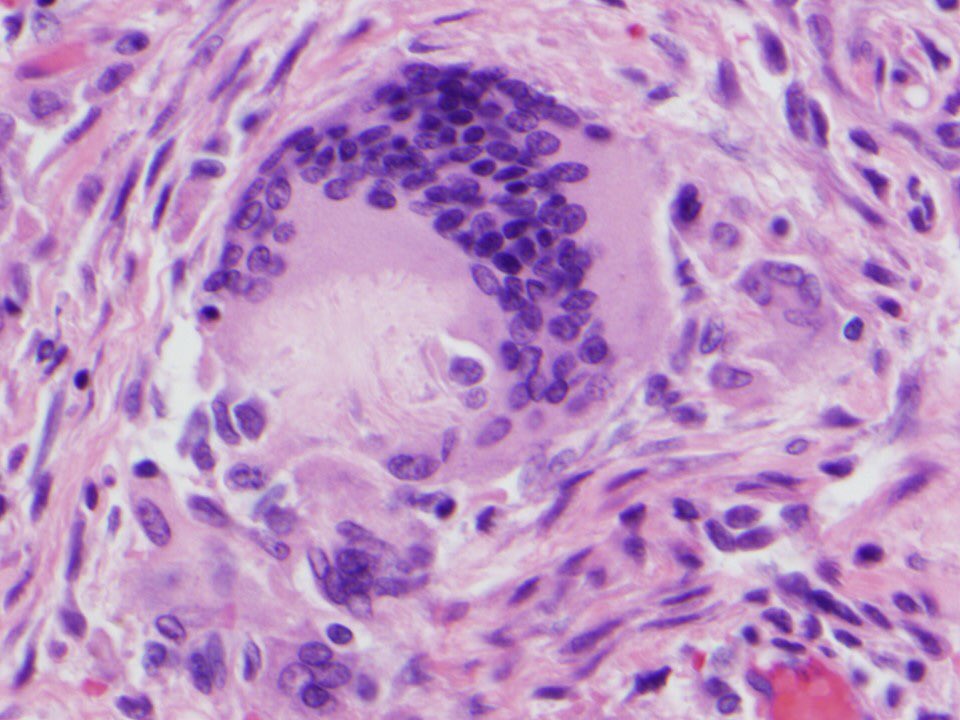
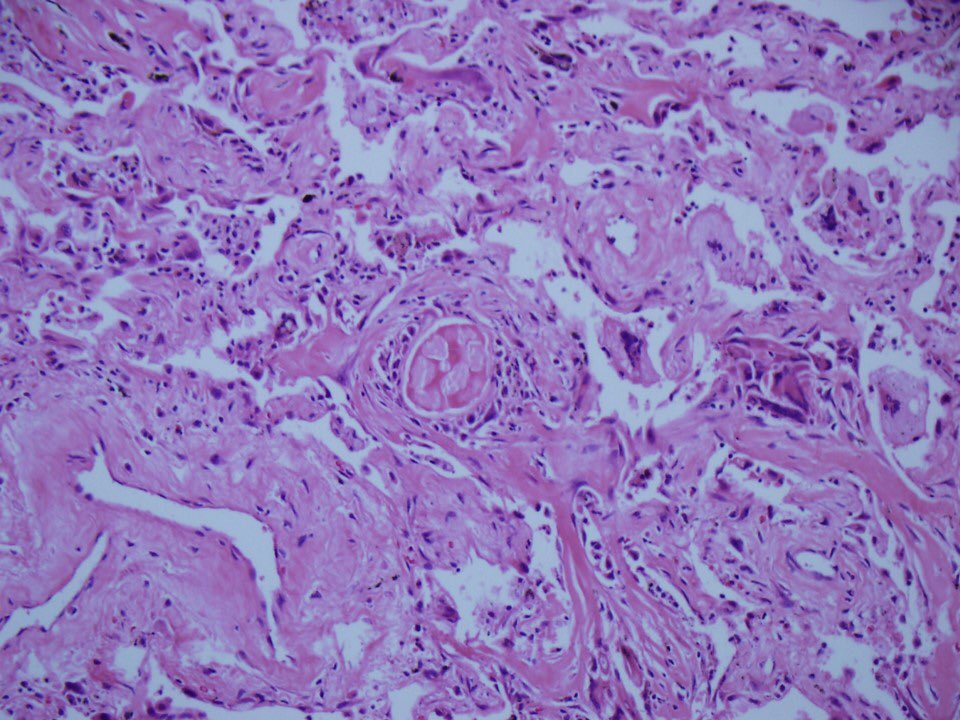
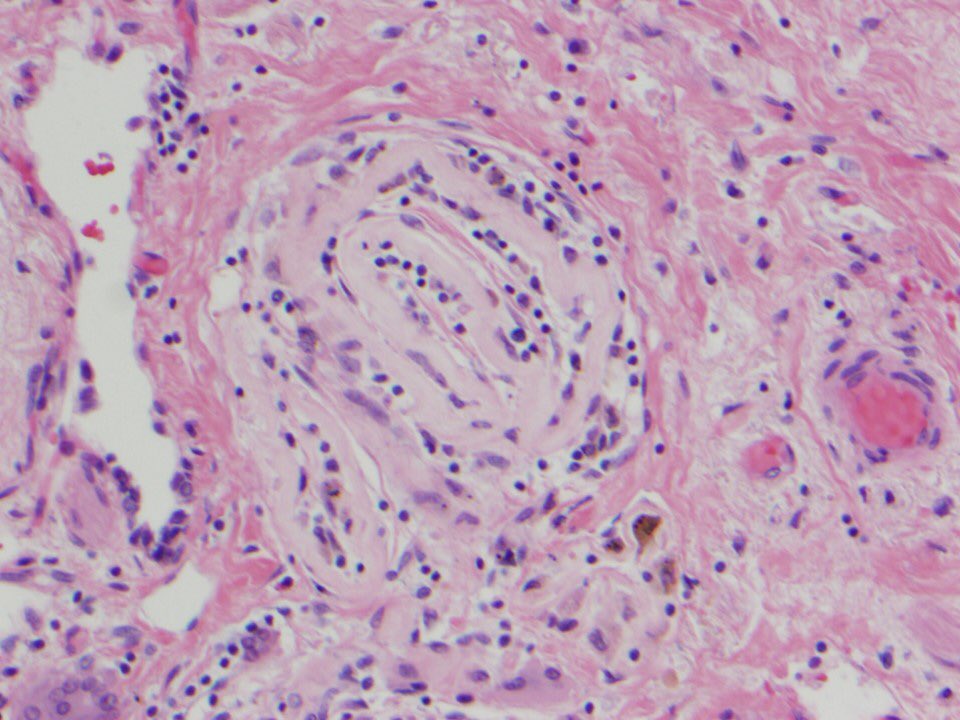
And the pathology gets REALLY weird. It deviates from what you expect to see in aspiration pneumonia. You expect to see INTACT food particles WITHIN bronchi or bronchioles associated with acute inflammation, right? A bit like this? 👇🏾👇🏾👇🏾(that’s potato, by the way)


And the pathology gets REALLY weird. It deviates from what you expect to see in aspiration pneumonia. You expect to see INTACT food particles WITHIN bronchi or bronchioles associated with acute inflammation, right? A bit like this? 👇🏾👇🏾👇🏾(that’s potato, by the way)
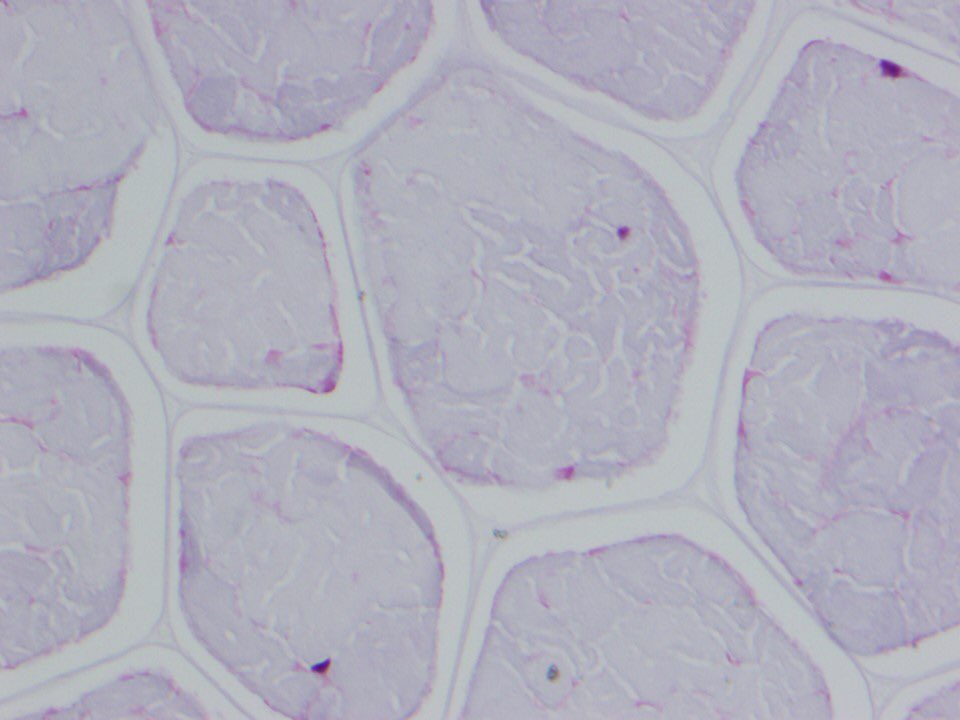
14/
How do I know that’s potato? When I was doing the study I embedded a bunch of different foods to see what they look like under the microscope. This was fun but of no use in real life because food degenerates when attacked by inflammatory cells for months...see next tweet



How do I know that’s potato? When I was doing the study I embedded a bunch of different foods to see what they look like under the microscope. This was fun but of no use in real life because food degenerates when attacked by inflammatory cells for months...see next tweet
15/
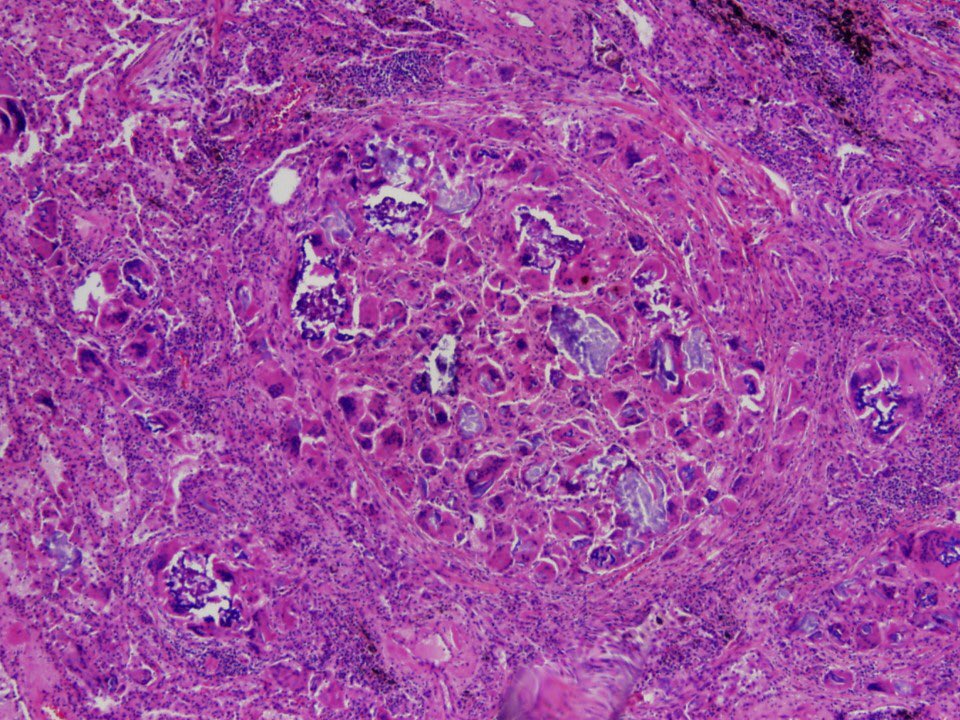
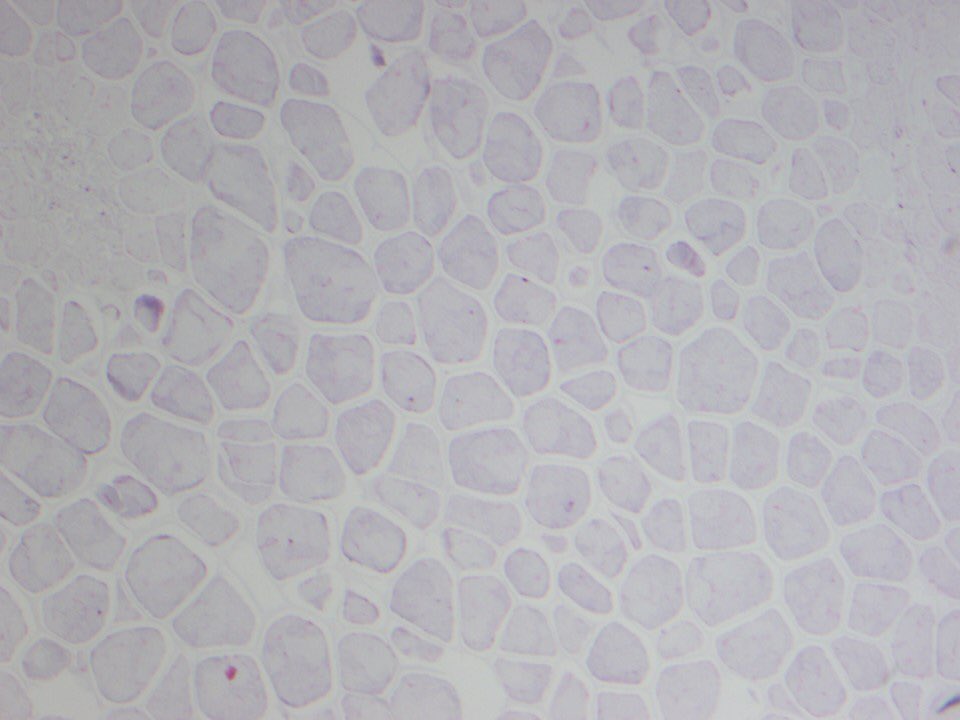
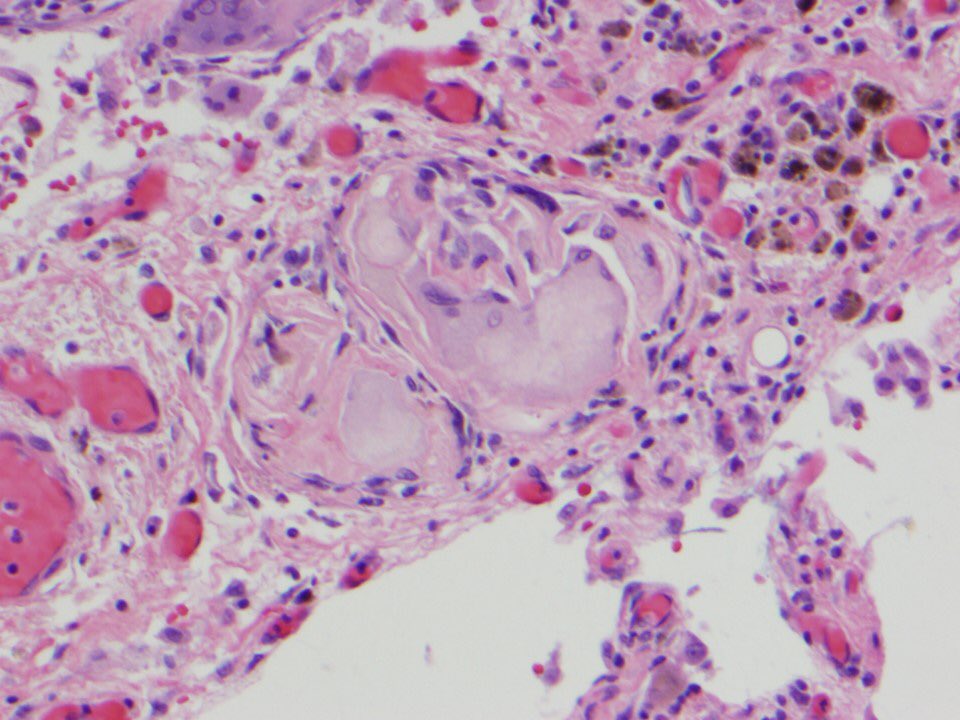
In lung biopsies with particulate matter aspiration, you will see intact and degenerated vegetable particles ANYWHERE in the parenchyma, not necessarily in a lumen. There is usually a giant cell around the material, and organizing pneumonia is common.



In lung biopsies with particulate matter aspiration, you will see intact and degenerated vegetable particles ANYWHERE in the parenchyma, not necessarily in a lumen. There is usually a giant cell around the material, and organizing pneumonia is common.
16/
The finding of food/vegetable matter in the context of an appropriate inflammatory reaction in the lung is diagnostic of aspiration.
Food WITHIN the lung. Surrounded by inflammation!! What can be more pathognomonic of aspiration?
¯\_(ツ)_/¯

The finding of food/vegetable matter in the context of an appropriate inflammatory reaction in the lung is diagnostic of aspiration.
Food WITHIN the lung. Surrounded by inflammation!! What can be more pathognomonic of aspiration?
¯\_(ツ)_/¯
17/
Over the years, I have heard odd responses to this diagnosis:
🔴 the barium swallow is normal!
🔴 she doesn’t have GERD!
🔴 the infiltrate is not in the RLL
Yet, folks have no problem attributing any infiltrate in someone with a dilated esophagus to aspiration ¯\_(ツ)_/¯
Over the years, I have heard odd responses to this diagnosis:
🔴 the barium swallow is normal!
🔴 she doesn’t have GERD!
🔴 the infiltrate is not in the RLL
Yet, folks have no problem attributing any infiltrate in someone with a dilated esophagus to aspiration ¯\_(ツ)_/¯
18/
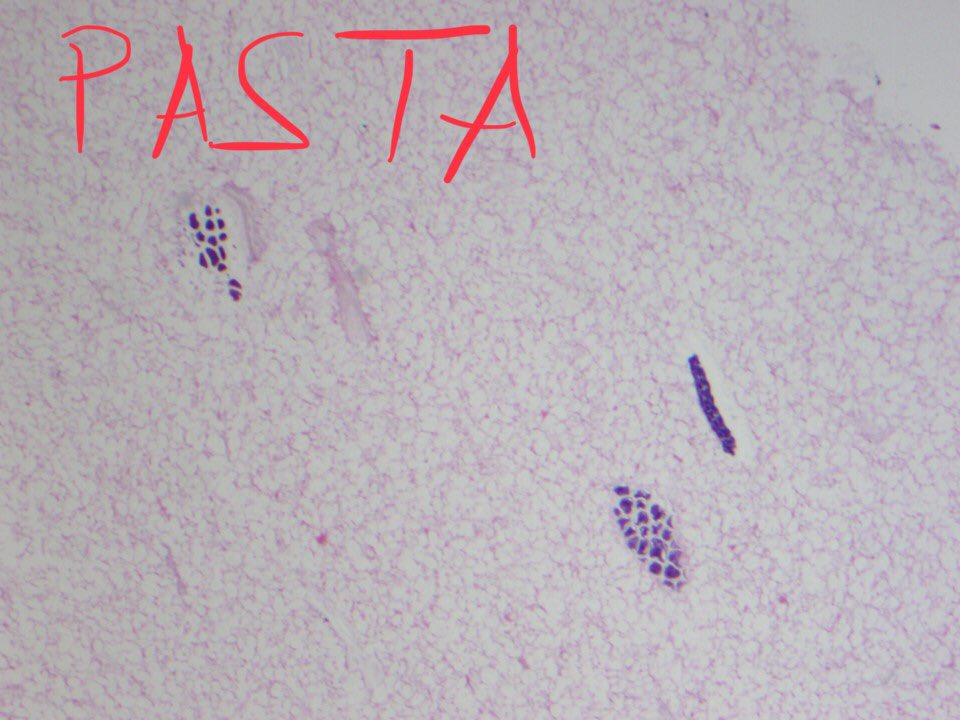
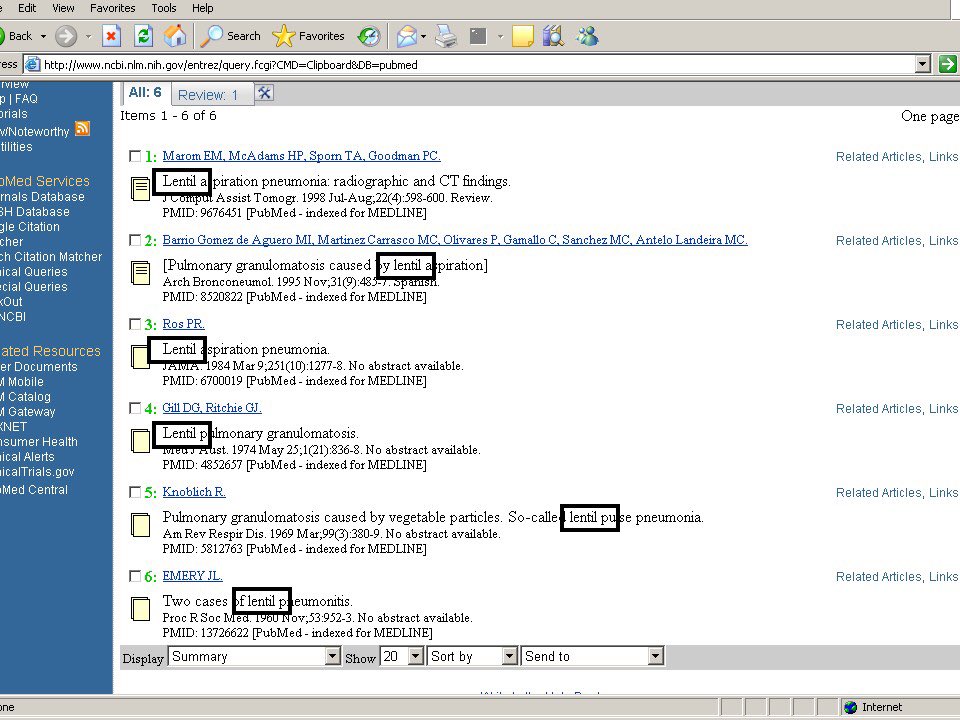
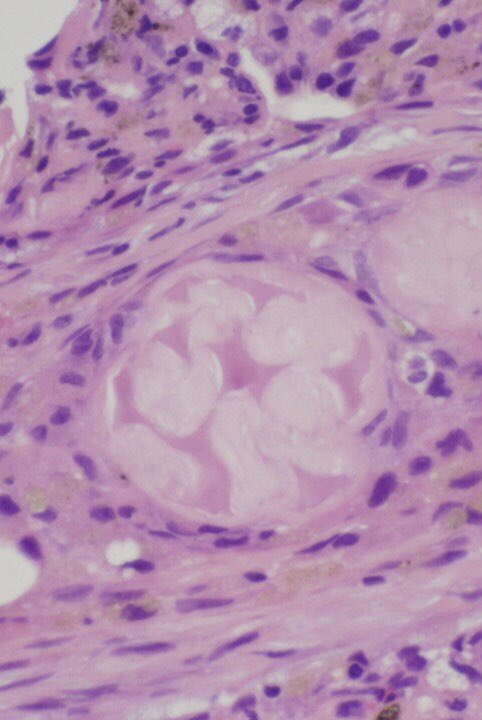
One of the most classic aspirated particles in this disease is the so-called “lentil”. It’s essentially a legume, which for some reason is aspirated a LOT and survives in the lung. First pic is a navy bean I embedded. Others are examples of lentil aspiration.



One of the most classic aspirated particles in this disease is the so-called “lentil”. It’s essentially a legume, which for some reason is aspirated a LOT and survives in the lung. First pic is a navy bean I embedded. Others are examples of lentil aspiration.
19/
Pill fillers or excipients only rarely show up in aspiration pneumonia. They are insoluble, so they can persist for long periods in the lung
Fillers in interstitium = think talc granulomatosis
Fillers associated with organizing pneumonia = consider aspiration

Pill fillers or excipients only rarely show up in aspiration pneumonia. They are insoluble, so they can persist for long periods in the lung
Fillers in interstitium = think talc granulomatosis
Fillers associated with organizing pneumonia = consider aspiration
20/
Microcrystalline cellulose and crospovidone are often found together, presumably because they’re both used in the same pills to provide bulk and other physical properties.
Remember what they look like! This will also help you to diagnose intravenous injection of pills.


Microcrystalline cellulose and crospovidone are often found together, presumably because they’re both used in the same pills to provide bulk and other physical properties.
Remember what they look like! This will also help you to diagnose intravenous injection of pills.
21/
And finally, you should try to learn to recognize food particles even when they’ve undergone advanced degeneration. This can be the key to making a specific diagnosis of particulate matter aspiration.



And finally, you should try to learn to recognize food particles even when they’ve undergone advanced degeneration. This can be the key to making a specific diagnosis of particulate matter aspiration.
22/
Now let’s repeat the quiz I gave in the beginning of this Tweetorial to see if we made some headway and learned something. The quiz (see next tweet in thread) is based on this pic 👇🏾
Thanks to @tony_breu for the idea to do this.
Now let’s repeat the quiz I gave in the beginning of this Tweetorial to see if we made some headway and learned something. The quiz (see next tweet in thread) is based on this pic 👇🏾
Thanks to @tony_breu for the idea to do this.
23/
What does the pic in the previous tweet show?
What does the pic in the previous tweet show?
24/
For clinicians: patients with this form of aspiration often have a history of esophageal or gastric surgery (like gastric bypass) or other abnormalities, CNS diseases or drug abuse. A history of recurrent pneumonia is classic.
🔬end of Tweetorial 🔬

For clinicians: patients with this form of aspiration often have a history of esophageal or gastric surgery (like gastric bypass) or other abnormalities, CNS diseases or drug abuse. A history of recurrent pneumonia is classic.
🔬end of Tweetorial 🔬
• • •
Missing some Tweet in this thread? You can try to
force a refresh