To celebrate 1 yr of taking referrals as the renal registrar on-call, it’s time for some kidney-themed #tipsfornewdocs covering high K, AKI, “nephrotoxins”, medications, iv contrast, hypertension, & caring for kidney transplant & dialysis patients. #nephpearls (thread)
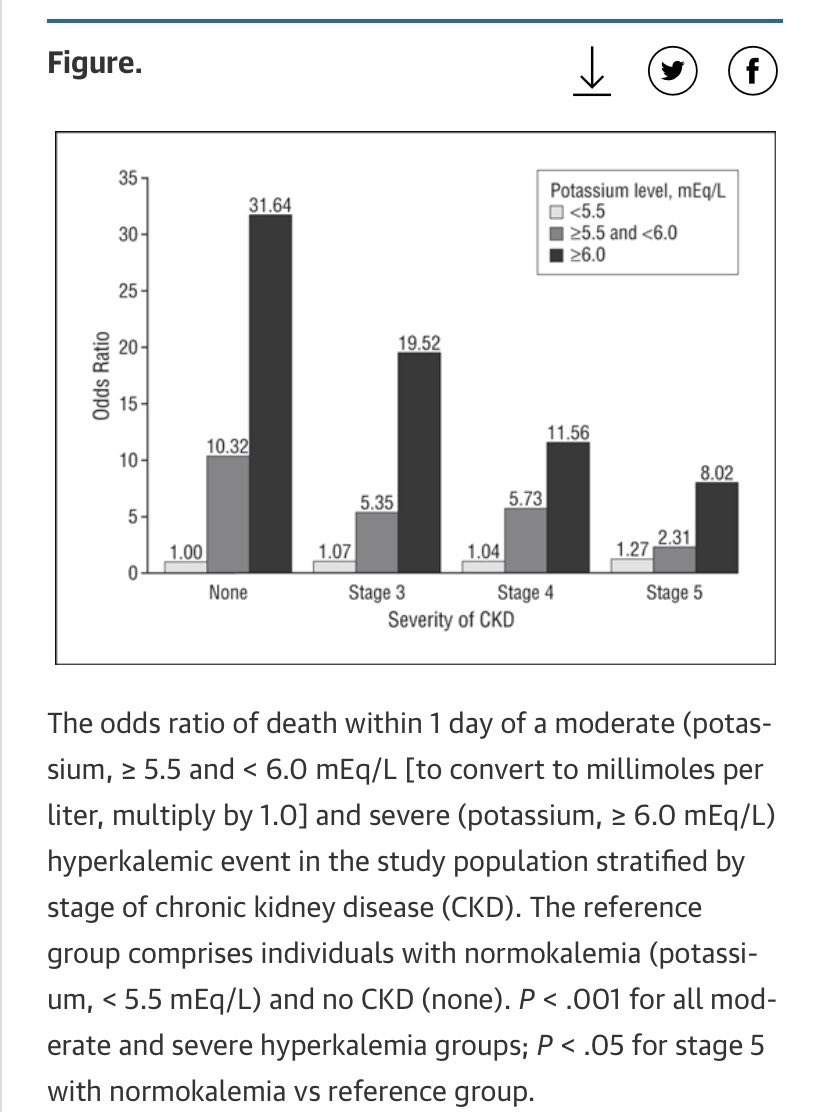
⬆️K - Renal #tipsfornewdocs 1/18
✅ Insulin-dextrose is not benign (⬇️BM risk) & does not get rid of K (only hides it), therefore rather than give round after round do phone us for help!
✅ Repeat ECG, re-bolus calcium gluconate if persistent changes
✅ Salbutamol dose = 10-20mg
✅ Insulin-dextrose is not benign (⬇️BM risk) & does not get rid of K (only hides it), therefore rather than give round after round do phone us for help!
✅ Repeat ECG, re-bolus calcium gluconate if persistent changes
✅ Salbutamol dose = 10-20mg
⬆️K - Renal #tipsfornewdocs 2/18
✅ Get a bicarb level (correct acidaemia to help ⬇️K)
✅ No one who can’t name 3 side-effects of bicarb should decide to give bicarb (not a bad rule for any drug!)
✅ Review NSAIDs, ACEi, A2RBs, spironactone, beta-blockers, trimethoprim, diet
✅ Get a bicarb level (correct acidaemia to help ⬇️K)
✅ No one who can’t name 3 side-effects of bicarb should decide to give bicarb (not a bad rule for any drug!)
✅ Review NSAIDs, ACEi, A2RBs, spironactone, beta-blockers, trimethoprim, diet
AKI - Renal #tipsfornewdocs 3/18
✅ Using eGFR in steady state CKD is fine but it isn’t helpful in AKI - use creatinine
✅ You can say you’ve sent “renal screen” but we’ll still ask what you’ve actually sent
✅ Avoid urinary catheters if bottles will measure urine output fine
✅ Using eGFR in steady state CKD is fine but it isn’t helpful in AKI - use creatinine
✅ You can say you’ve sent “renal screen” but we’ll still ask what you’ve actually sent
✅ Avoid urinary catheters if bottles will measure urine output fine
AKI - Renal #tipsfornewdocs 4/18
✅ AKI doesn’t respond to giving litre upon litre of IVT to euvolaemic, normotensive patients
✅ It’s always obstruction in older men until proven otherwise
✅ In wet patients with AKI, continuing diuresis will almost always be our answer
✅ AKI doesn’t respond to giving litre upon litre of IVT to euvolaemic, normotensive patients
✅ It’s always obstruction in older men until proven otherwise
✅ In wet patients with AKI, continuing diuresis will almost always be our answer
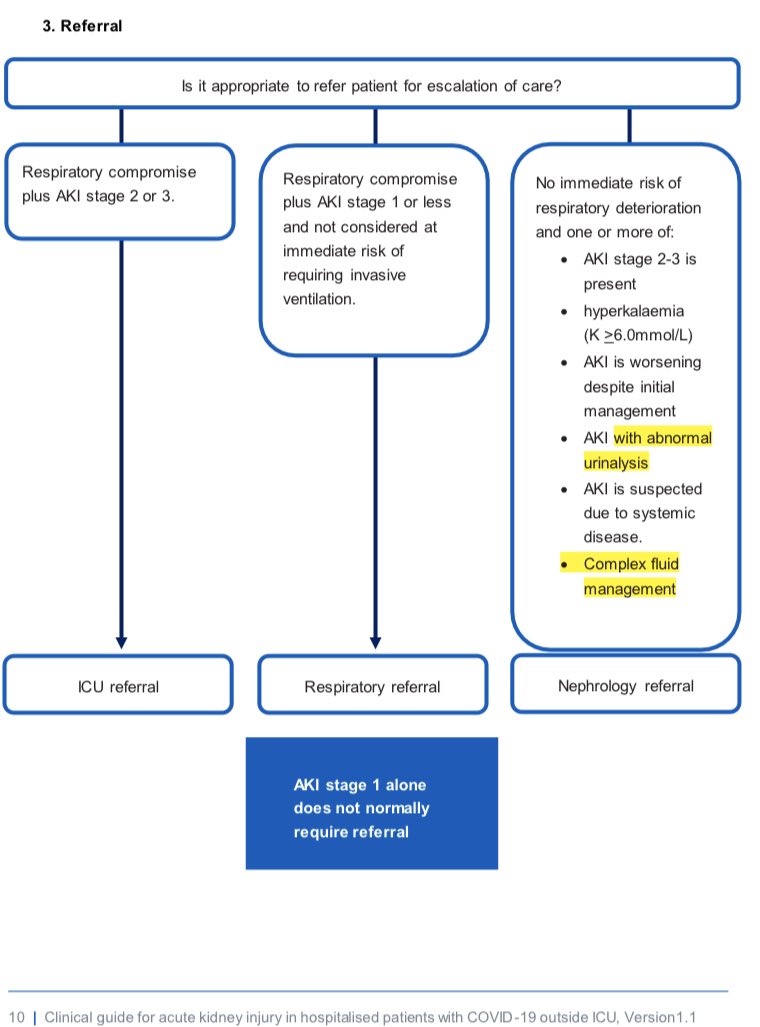
AKI - Renal #tipsfornewdocs 5/18
At referral, we’re thinking 4 qs;
1. Differential diagnosis? Hence we need historical creatinines, volume status, urine dip, imaging results, all events & bloods this admission, new & prev meds
2. Patient safe to transfer? Need current obs, K, pH
At referral, we’re thinking 4 qs;
1. Differential diagnosis? Hence we need historical creatinines, volume status, urine dip, imaging results, all events & bloods this admission, new & prev meds
2. Patient safe to transfer? Need current obs, K, pH
AKI - Renal #tipsfornewdocs 6/18
3. Safe to biopsy? Correct coag, valid group & save, r/v anti-platelets, control ⬆️BP
4. Safe to dialyse? Urgent BBV serology = avoid dialysing in isolation = ⬆️efficiency of dialysis nurse time. Octenisan & naseptin = lines safer with ⬇️SA load
3. Safe to biopsy? Correct coag, valid group & save, r/v anti-platelets, control ⬆️BP
4. Safe to dialyse? Urgent BBV serology = avoid dialysing in isolation = ⬆️efficiency of dialysis nurse time. Octenisan & naseptin = lines safer with ⬇️SA load
“Nephrotoxins” - Renal #tipsfornewdocs 7/18
❌ Most common reason for re-admission after AKI = pulmonary oedema
❌ Likely factor = ACEi and/or diuretics stopped (possibly appropriately in short term) but without review in patients who needed them going forwards
❌ Most common reason for re-admission after AKI = pulmonary oedema
❌ Likely factor = ACEi and/or diuretics stopped (possibly appropriately in short term) but without review in patients who needed them going forwards
“Nephrotoxins” - Renal #tipsfornewdocs 8/18
✅ ACEi in heart failure with reduced ejection fraction (HFrEF) = one of most beneficial drugs known to man
✅ If you wouldn’t stop chemotherapy without review plan, don’t stop ACEi in HFrEF without one (benefit often many fold higher)
✅ ACEi in heart failure with reduced ejection fraction (HFrEF) = one of most beneficial drugs known to man
✅ If you wouldn’t stop chemotherapy without review plan, don’t stop ACEi in HFrEF without one (benefit often many fold higher)
“Nephrotoxins” - Renal #tipsfornewdocs 9/18
✅ Don’t tell HFrEF patient “those ACEi drugs poisoned your kidneys” - creates massive headache when comes to restarting the life-saving drug
✅ Diuretics can actually can be good for the kidneys - especially if patient congested
✅ Don’t tell HFrEF patient “those ACEi drugs poisoned your kidneys” - creates massive headache when comes to restarting the life-saving drug
✅ Diuretics can actually can be good for the kidneys - especially if patient congested
Medications - Renal #tipsfornewdocs 10/18
❌ No clarithromycin for patients on tacrolimus
❌ Metformin is a “good day” only drug
❌ No baclofen in later stage CKD/dialysis
❌ Try to avoid trimethoprim / co-trimoxazole in AKI as pushes up creatinine (& ⬆️K) & muddies the waters
❌ No clarithromycin for patients on tacrolimus
❌ Metformin is a “good day” only drug
❌ No baclofen in later stage CKD/dialysis
❌ Try to avoid trimethoprim / co-trimoxazole in AKI as pushes up creatinine (& ⬆️K) & muddies the waters
Iv contrast - Renal #tipsfornewdocs 11/18
☠️ If you or your reg are worried your patient with AKI or CKD could have ischaemic bowel then do the contrast CT scan - there’s no value protecting the appearance of the kidneys on autopsy.
(if iv contrast would have hurt at all....)
☠️ If you or your reg are worried your patient with AKI or CKD could have ischaemic bowel then do the contrast CT scan - there’s no value protecting the appearance of the kidneys on autopsy.
(if iv contrast would have hurt at all....)
⬆️BP - Renal #tipsfornewdocs 12/18
✅ Think of asymptomatic inpatient ⬆️BP as a chronic problem = STAT doses of meds are rarely required (also, treat pain!)
✅ Amlodipine takes 8 hrs to reach peak concentration; lower re-check BP 30mins after STAT dose is regression to the mean
✅ Think of asymptomatic inpatient ⬆️BP as a chronic problem = STAT doses of meds are rarely required (also, treat pain!)
✅ Amlodipine takes 8 hrs to reach peak concentration; lower re-check BP 30mins after STAT dose is regression to the mean
Transplant pts - Renal #tipsfornewdocs 13/18
✅ We want to know they’re in, esp if immunosuppression issue (NBM, infection - double pred!), or AKI (get urgent US for starters)
✅ Tacrolimus & ciclosporin at 10am & 10pm (gives phlebotomy time to take trough levels before AM dose)
✅ We want to know they’re in, esp if immunosuppression issue (NBM, infection - double pred!), or AKI (get urgent US for starters)
✅ Tacrolimus & ciclosporin at 10am & 10pm (gives phlebotomy time to take trough levels before AM dose)
Haemodialysis (HD) pts on wards - Renal #tipsfornewdocs 14/18
Let us know if they;
✅ Bleed; we’ll avoid heparin on HD
✅ Need surgery; need HD re-arranged
✅ Get sick; outpatient HD unit mightn’t be safest place for them
✅ Need routine bloods; easy on HD days, saves extra stab
Let us know if they;
✅ Bleed; we’ll avoid heparin on HD
✅ Need surgery; need HD re-arranged
✅ Get sick; outpatient HD unit mightn’t be safest place for them
✅ Need routine bloods; easy on HD days, saves extra stab
Haemodialysis pts on wards - Renal #tipsfornewdocs 15/18
❌ Creatinine & urea build up again after HD; this doesn’t mean they need IVT
❌ Post-HD K often low; this doesn’t mean it needs replaced (K rapidly builds-up again)
✅ Renal pharmacists are great asset if can find them
❌ Creatinine & urea build up again after HD; this doesn’t mean they need IVT
❌ Post-HD K often low; this doesn’t mean it needs replaced (K rapidly builds-up again)
✅ Renal pharmacists are great asset if can find them
Dialysis pts on wards - Renal #tipsfornewdocs 16/18
✅ If still pee, protect residual renal function
✅ If anuric, think of them like closed box - any fluid you put in has to get out somehow. Never for bag upon bag of “maintenance iv fluids”. If need bolus, 250ml & re-assess.
✅ If still pee, protect residual renal function
✅ If anuric, think of them like closed box - any fluid you put in has to get out somehow. Never for bag upon bag of “maintenance iv fluids”. If need bolus, 250ml & re-assess.
Renal #tipsfornewdocs 17/18
Things we’ll (almost) always say no to;
❌ “Can I take blood from the fistula?”
❌ “Can we use the tunnelled dialysis line as routine iv access?”
❌ “Do you want to see this patient with renal colic?”
❌ “Would EPO help with anything at 2am?”
Things we’ll (almost) always say no to;
❌ “Can I take blood from the fistula?”
❌ “Can we use the tunnelled dialysis line as routine iv access?”
❌ “Do you want to see this patient with renal colic?”
❌ “Would EPO help with anything at 2am?”
Renal #tipsfornewdocs 18/18
Other way to save a life;
✅ If swapping to meropenum plus more IVT for a recurrent temp spike with worsening AKI, ask “Could this be vasculitis?”
Easiest way to save a life;
✅ Remember IVT is one of the most dangerous drugs you prescribe
Other way to save a life;
✅ If swapping to meropenum plus more IVT for a recurrent temp spike with worsening AKI, ask “Could this be vasculitis?”
Easiest way to save a life;
✅ Remember IVT is one of the most dangerous drugs you prescribe
Apologies if tone of above a bit negative at times!! We are nice and helpful really!
Would like to hear anyone else’s top tips too.
Would like to hear anyone else’s top tips too.
• • •
Missing some Tweet in this thread? You can try to
force a refresh