Last week twitter was unexpectedly keen for renal registrar on-call tips, so here’s round 2️⃣ of kidney #tipsfornewdocs covering iv fluids, AKI, “renal screen” bloods, immunosuppression, electrolytes, DKA in ESKD, peritoneal dialysis, proteinuria, meds & ⬆️BP (thread)
#nephpearls
#nephpearls
Iv fluids; Renal #tipsfornewdocs 2️⃣ 1/15
✅ 1L 5% dextrose 12 hourly = 50g glucose = 55 skittles. Not same as feeding patient.
✅ “iv fluid for AKI plus furosemide to keep it off their chest” isn’t a thing - commit to goal of wetter or drier.
(specialist use only eg. ⬆️Ca, ⬆️K)
✅ 1L 5% dextrose 12 hourly = 50g glucose = 55 skittles. Not same as feeding patient.
✅ “iv fluid for AKI plus furosemide to keep it off their chest” isn’t a thing - commit to goal of wetter or drier.
(specialist use only eg. ⬆️Ca, ⬆️K)
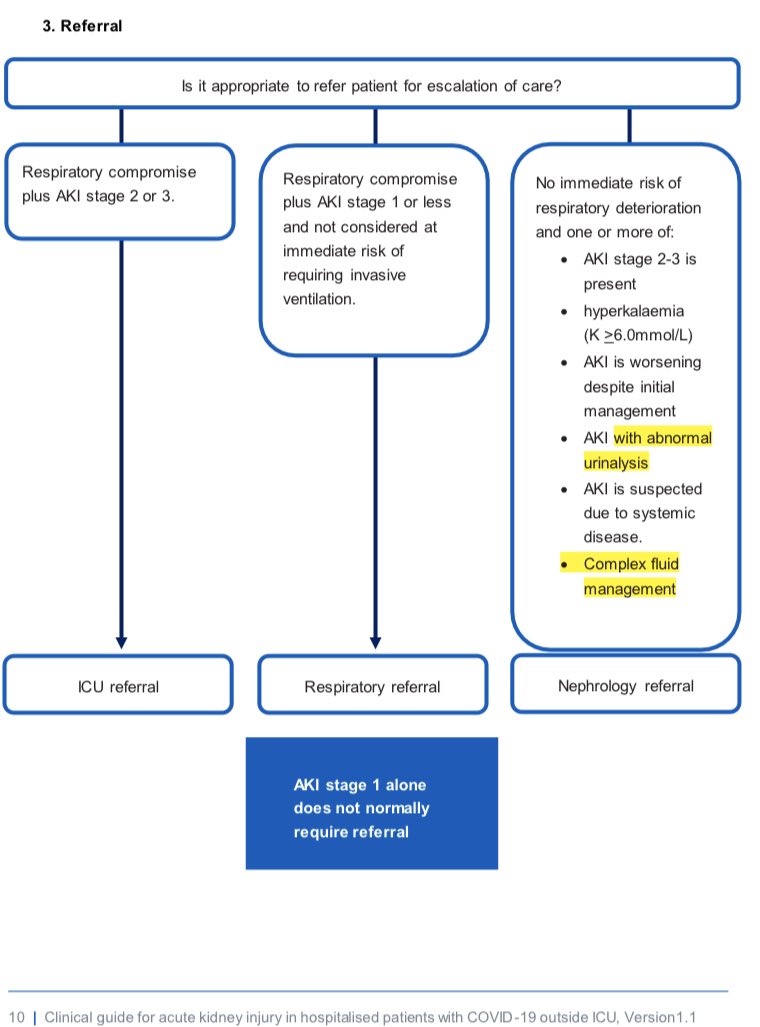
AKI; Renal #tipsfornewdocs 2️⃣ 2/15
✅ In AKI anticipate accumulating meds (eg opiates,insulin) & ⬇️dose before complications
✅ Seeing unobstructed AKI pt, BP/K/pH fine but becoming oligoanuric at 1am despite euvolaemia? It’s OK to watch + wait. Trial by drowning not obligatory.
✅ In AKI anticipate accumulating meds (eg opiates,insulin) & ⬇️dose before complications
✅ Seeing unobstructed AKI pt, BP/K/pH fine but becoming oligoanuric at 1am despite euvolaemia? It’s OK to watch + wait. Trial by drowning not obligatory.
AKI; Renal #tipsfornewdocs 2️⃣ 3/15
AKI “renal screen” bloods MIGHT include;
✔️Myeloma screen (Igs, serum EP, SFLCs)
✔️ANCA(MPO & PR3), anti-GBM, cryos, autoantibodies, C3/C4, dsDNA, ASOT, (PLA2R)
✔️Blood cultures x3
✔️CK
✔️Eosinophils (serum, not urine)
✔️HIV/Hep/Adeno/CMV/BKV
AKI “renal screen” bloods MIGHT include;
✔️Myeloma screen (Igs, serum EP, SFLCs)
✔️ANCA(MPO & PR3), anti-GBM, cryos, autoantibodies, C3/C4, dsDNA, ASOT, (PLA2R)
✔️Blood cultures x3
✔️CK
✔️Eosinophils (serum, not urine)
✔️HIV/Hep/Adeno/CMV/BKV
AKI; Renal #tipsfornewdocs 2️⃣ 4/15
“Renal screen” cont;
✔️Haemolysis screen (film, ⬆️bili,⬆️LDH,⬇️hapto, DAT)
✔️STEC PCR / ADAMTS13
✔️ACE
✔️Paracetamol/salicylate/toxic alcohol, urine for illicit
✔️Other eg. Lepto PCR, legionella, oxalate
BUT which to send depends on the story!
“Renal screen” cont;
✔️Haemolysis screen (film, ⬆️bili,⬆️LDH,⬇️hapto, DAT)
✔️STEC PCR / ADAMTS13
✔️ACE
✔️Paracetamol/salicylate/toxic alcohol, urine for illicit
✔️Other eg. Lepto PCR, legionella, oxalate
BUT which to send depends on the story!
AKI; Renal tips 2️⃣ 5/15
Ward nurses/HCAs;
✅ Meticulous input/output record in AKI is key aid in dialysis decisions
✅ For low K diet advice either ask dietitian (knows 50+ risky foods) or me (knows 🍌 = bad)
✅ Whoever writes dipstick result in medical notes = renal reg’s hero
Ward nurses/HCAs;
✅ Meticulous input/output record in AKI is key aid in dialysis decisions
✅ For low K diet advice either ask dietitian (knows 50+ risky foods) or me (knows 🍌 = bad)
✅ Whoever writes dipstick result in medical notes = renal reg’s hero
Immunosuppression; Renal #tipsfornewdocs 2️⃣ 6/15
✅ Half-life of iv hydrocortisone = 100 mins, so transplant pt on pred needs TDS/QDS dosing if NBM
✅ Continue MMF in the v well transplant pt with simple infection, suspend if v sick, inbetween talk to us 1st (talk to us anyway!)
✅ Half-life of iv hydrocortisone = 100 mins, so transplant pt on pred needs TDS/QDS dosing if NBM
✅ Continue MMF in the v well transplant pt with simple infection, suspend if v sick, inbetween talk to us 1st (talk to us anyway!)
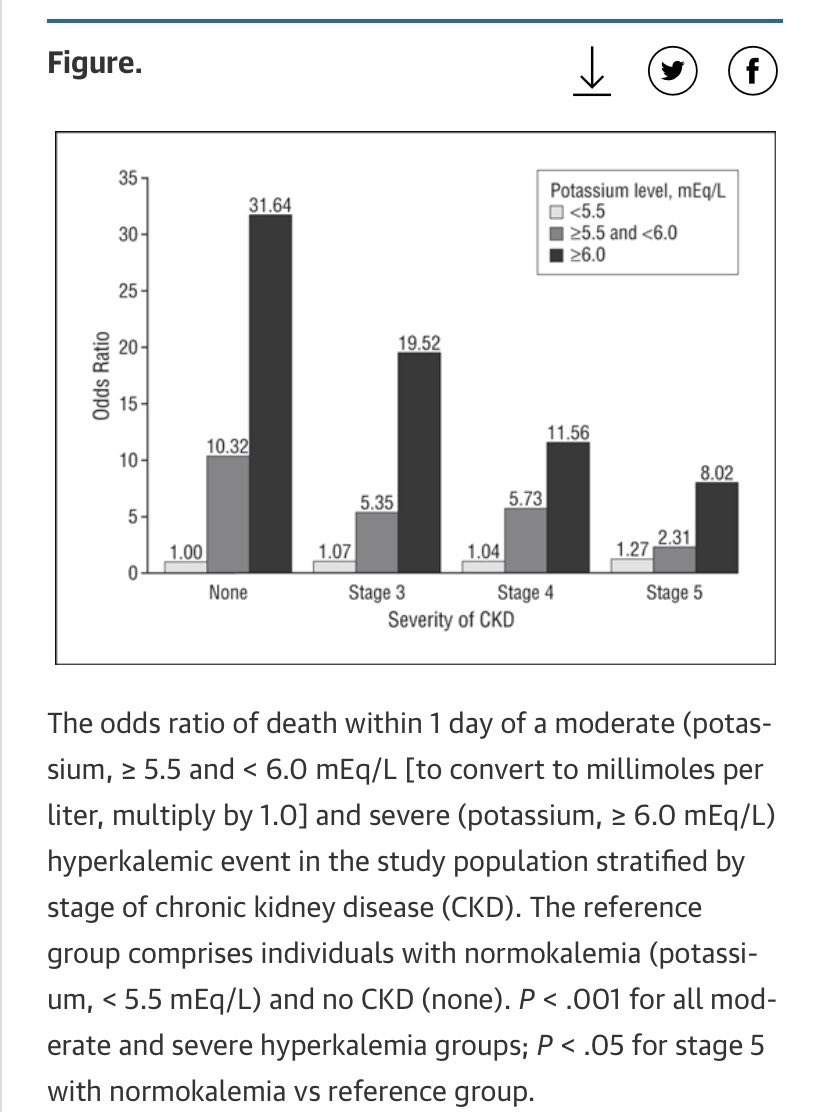
Electrolytes; Renal #tipsfornewdocs 2️⃣ 7/15
✅ You won’t correct ⬇️K if you don’t correct ⬇️Mg first (distal tubule magic). Replace Mg slowly.
✅ Diarrhoea main side-effect of PO K/PO4/Mg sachets.
✅ Electrolytes don’t always need replacing just because they’re red on the screen
✅ You won’t correct ⬇️K if you don’t correct ⬇️Mg first (distal tubule magic). Replace Mg slowly.
✅ Diarrhoea main side-effect of PO K/PO4/Mg sachets.
✅ Electrolytes don’t always need replacing just because they’re red on the screen
DKA in ESKD; Renal #tipsfornewdocs 2️⃣ 8/15
Some protection from DKA in ESKD as ⬇️insulin clearance, & less hypovolaemia as ⬇️osmotic diuresis with ⬇️nephrons
But if get DKA;
⬆️vulnerability to overload & hypos from Tx
❗️Time for individualised approach, NOT cookbook protocol❗️
Some protection from DKA in ESKD as ⬇️insulin clearance, & less hypovolaemia as ⬇️osmotic diuresis with ⬇️nephrons
But if get DKA;
⬆️vulnerability to overload & hypos from Tx
❗️Time for individualised approach, NOT cookbook protocol❗️
DKA in ESKD 9/15
☠️ If anuric & hypervolaemic in DKA need unopposed iv insulin = HDU
Anuric pt;
⬆️sugars ➡️ osmotic shift H2O intra to extracellular but without usual ⬆️urine output (+ ⬆️thirst) = intravascular EXPANSION in DKA = iv insulin on own can reverse pulmonary oedema!
☠️ If anuric & hypervolaemic in DKA need unopposed iv insulin = HDU
Anuric pt;
⬆️sugars ➡️ osmotic shift H2O intra to extracellular but without usual ⬆️urine output (+ ⬆️thirst) = intravascular EXPANSION in DKA = iv insulin on own can reverse pulmonary oedema!
Peritoneal dialysis (PD); Renal #tipsfornewdocs 2️⃣ 10/15
☠️ PD peritonitis the big concern with any of abdo pain, cloudy PD bags, GI upset. Needs PD fluid WCC & culture - phone renal unit for advice. Your iv abx are just as good as our intraperitoneal abx until transfer sorted.
☠️ PD peritonitis the big concern with any of abdo pain, cloudy PD bags, GI upset. Needs PD fluid WCC & culture - phone renal unit for advice. Your iv abx are just as good as our intraperitoneal abx until transfer sorted.
Peritoneal dialysis (PD); Renal #tipsfornewdocs 2️⃣ 11/15
‼️ Please take a sec to google what a PD catheter looks like versus a suprapubic urinary catheter - the absolute least fun conversation we can have is after a urometer has been attached to the sterile PD tube connection‼️
‼️ Please take a sec to google what a PD catheter looks like versus a suprapubic urinary catheter - the absolute least fun conversation we can have is after a urometer has been attached to the sterile PD tube connection‼️
Proteinuria; Renal #tipsfornewdocs 2️⃣ 12/15
✅ Do urine ACR or PCR, no one does 24hr collection now
✅ Nephrotic PCR = >300mg/mmol
✅ Pt with “?1st presentation CCF” & ⬇️albumin - could all be nephrotic Sx, do uPCR
✅ ⬇️alb + oedema post-sepsis with PCR 35 = sick, not nephrotic
✅ Do urine ACR or PCR, no one does 24hr collection now
✅ Nephrotic PCR = >300mg/mmol
✅ Pt with “?1st presentation CCF” & ⬇️albumin - could all be nephrotic Sx, do uPCR
✅ ⬇️alb + oedema post-sepsis with PCR 35 = sick, not nephrotic
Meds; Renal #tipsfornewdocs 2️⃣ 13/15
✅ Gabapentin in CKD = go so low & so slow eg. 100mg once daily for starters
✅ Aciclovir = must dose reduce in CKD to avoid encephalopathy
✅ Largest cause of “resistant hypertension” is nonadherence; simplifying the med schedule helps!
✅ Gabapentin in CKD = go so low & so slow eg. 100mg once daily for starters
✅ Aciclovir = must dose reduce in CKD to avoid encephalopathy
✅ Largest cause of “resistant hypertension” is nonadherence; simplifying the med schedule helps!
⬆️BP; Renal #tipsfornewdocs 2️⃣ 14/15
✅ Don’t keep ⬆️BP meds to aim great control while inpatient without gd reason & follow-up. Many take >4wks to max effect anyway (graph)
✅ HFrEF= bisop, metop, carvedilol
Portal ⬆️BP= propran, carv
Essential ⬆️BP= not BB 1st line (or 2,3,4)
✅ Don’t keep ⬆️BP meds to aim great control while inpatient without gd reason & follow-up. Many take >4wks to max effect anyway (graph)
✅ HFrEF= bisop, metop, carvedilol
Portal ⬆️BP= propran, carv
Essential ⬆️BP= not BB 1st line (or 2,3,4)

Renal #tipsfornewdocs 2️⃣ 15/15
Bonus;
❌ Writing “GP repeat U&Es in 3 days” on discharge letter isn’t OK. Write why, 📞 to book.
✅ Self-discharge forms assess capacity to hold a pen, for capacity to self-discharge need to see pt & write in notes (also give meds & 🆘 advice).
Bonus;
❌ Writing “GP repeat U&Es in 3 days” on discharge letter isn’t OK. Write why, 📞 to book.
✅ Self-discharge forms assess capacity to hold a pen, for capacity to self-discharge need to see pt & write in notes (also give meds & 🆘 advice).
Again, sometimes hard to give short tips you think are helpful that don’t all come across a bit negative - my apologies!
Some stolen following @CharlieTomson @HotKidneyAction @Yuv90 @RenalMed on twitter.
Thanks Tim Ellam for input.
Some stolen following @CharlieTomson @HotKidneyAction @Yuv90 @RenalMed on twitter.
Thanks Tim Ellam for input.
• • •
Missing some Tweet in this thread? You can try to
force a refresh