Some thoughts on the repurposing of chloroquine (CQ) and hydroxychloroquine (HCQ) for coronavirus infection. /1
How might CQ or HCQ help with COVID-19?
Potential mechanisms include:
- inhibiting viral replication
- ↑endosomal pH required for cell fusion
- ↓viral binding to target cells by impairing glycosylation of the ACE2 receptor
sciencedirect.com/science/articl… /2
Potential mechanisms include:
- inhibiting viral replication
- ↑endosomal pH required for cell fusion
- ↓viral binding to target cells by impairing glycosylation of the ACE2 receptor
sciencedirect.com/science/articl… /2
This document has garnered a lot of attention, in part because its title is so declarative docs.google.com/document/d/e/2… /3 

Now I’m no virologist, but the in vitro studies are *really* intriguing.
Here’s a 2005 paper showing that CQ prevented the spread of SARS (another coronavirus) in cell culture. virologyj.biomedcentral.com/articles/10.11… /4

Here’s a 2005 paper showing that CQ prevented the spread of SARS (another coronavirus) in cell culture. virologyj.biomedcentral.com/articles/10.11… /4


As for SARS-CoV2, this study in @cell_res found that CQ inhibited viral spread in a concentration-dependent fashion nature.com/articles/s4142… /5 
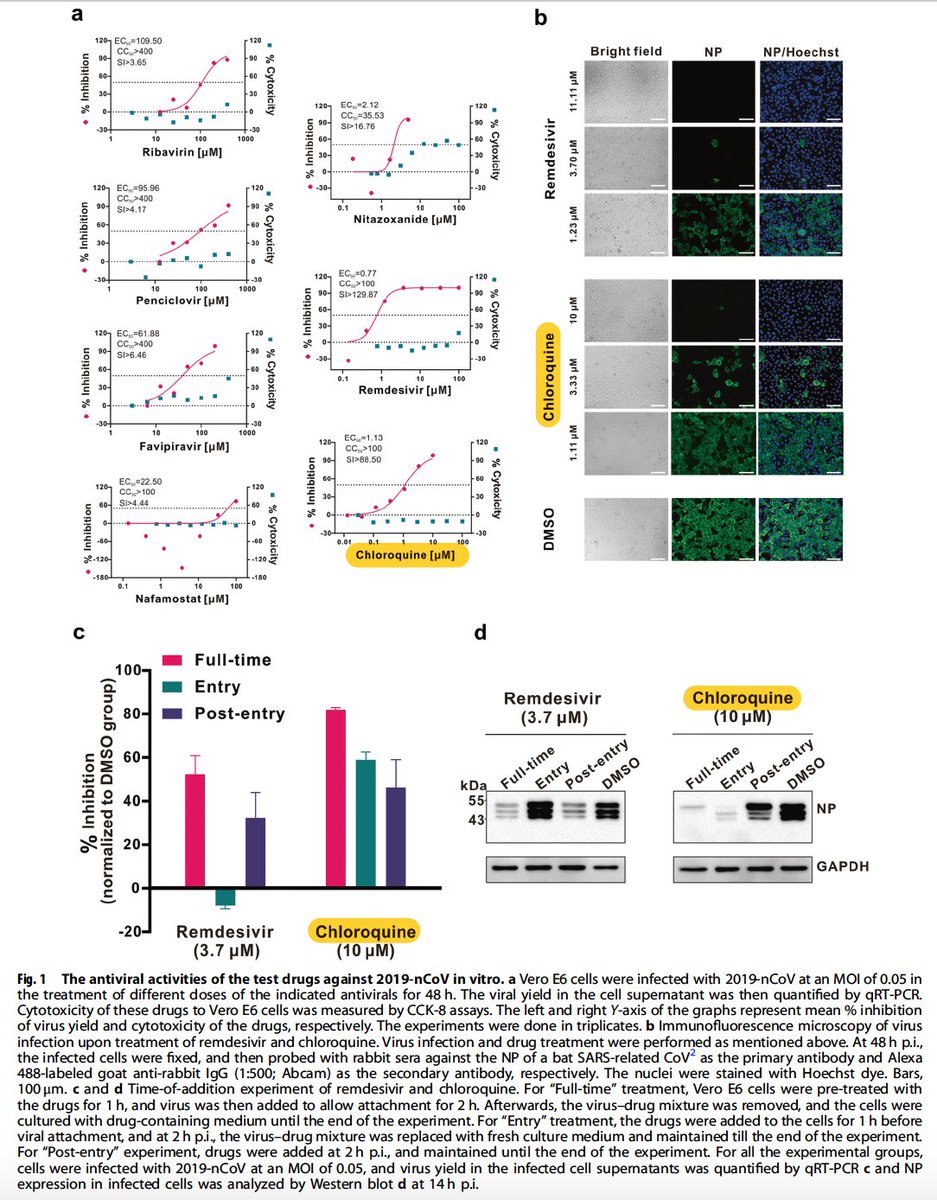
Comparing HCQ and CQ against SARS-CoV2 in vitro, HCQ is clearly more potent. That's good news because it's also better tolerated clinically. academic.oup.com/cid/advance-ar… /6 

What about clinical data? Early days, but this paper says CQ improved multiple outcomes in a study of >100 patients in China. (N.B. not much detail on methodology, and the result are from news briefing ...)
jstage.jst.go.jp/article/bst/14… /7
jstage.jst.go.jp/article/bst/14… /7

Most exciting stuff so far? This, just out from Didier Raoult’s group in Marseille drive.google.com/file/d/186Bel9…
Small, open-label study awaiting peer review. But it sure looks like HCQ (600 mg /day) hastens viral cure, maybe with a synergistic effect of azithromycin. /8

Small, open-label study awaiting peer review. But it sure looks like HCQ (600 mg /day) hastens viral cure, maybe with a synergistic effect of azithromycin. /8


While that's encouraging, here's a thoughtful commentary in @ViralRes reminding us that chloroquine failed to do much for influenza and ebolavirus, and it actually worsened matters in a primate model of chikungunya. sciencedirect.com/science/articl… /9 

What to do with all this? Not sure, but HCQ is pretty well tolerated. I'd give it a shot in confirmed COVID-19, maybe with azithromycin, until we have firmer data to guide us one way or the other.
Just my $0.02. Also, tweets are not medical advice.
/ end
Just my $0.02. Also, tweets are not medical advice.
/ end
BTW we really need studies looking at clinically important outcomes. Found this at ClinicalTrials.gov clinicaltrials.gov/ct2/results?co… 

• • •
Missing some Tweet in this thread? You can try to
force a refresh