#COVID19FOAM
#StopTheSpread
#ProtectHealthCareWorkers
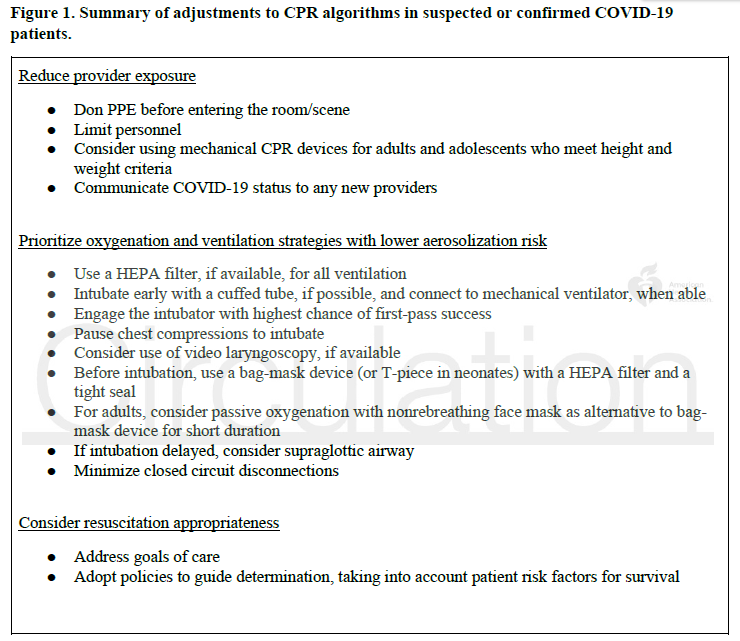
Joint effort from @American_Heart @ACEPNow @SOCCA_CritCare @AmerAcadPeds @aarc_tweets @ASALifeline guiding #resuscitation efforts in #cardiacarrest in suspected/confirmed #COVID19
bit.ly/3e8QplH
@CircAHA



General Principles of #ProtectHealthCareWorkers have always applied to first responders in prior #resuscitation guidelines. Remember, first things first:
👉Assess the safety of the scene, make sure that victim, yourself and bystanders are safe
#GetMePPE
Minimize the number of people in the room
👉 Whenever able, mechanical CPR devices can reduce the number of rescuers required & provide consistent high-quality compressions
1⃣1st assess the rhythm and defibrillate ventricular arrhythmias
2⃣ back to ABC: Airway- Breathing- Circulation.
Yup, the brain will have to wait for the perfusion as we secure the airway to lower the risk of aerosolization using a close circuit with HEPA filter
And, in this context, it is OKAY to pause chest compressions to intubate.
For those already intubated at the time of #cardiacarrest, keep them on the vent preserve the close circuit with HEPA filter
👉adjust the ventilator settings to allow for asynchronous ventilation
👉 set the trigger Off
👉FiO2 100%, RR 10/min
@emcrit input for settings?
If prone at time of #cardiacarrest
👉place back on supine if native airway to facilitate intubation/SGA
👉prone CPR (!) with pads in A/P position, chest compressions over T7/T10
If you are proning patients routinely, please practice quick turns for emergencies

I am sure some contention will arise surrounding the lack of evidence for a few things (prone CPR in particular), but it is important that we share a mental model of #resuscitation approaches to #COVID19 #cardiacarrest
Safety first
Address goals of care early and often
FIN