Well, it’s (all but) official:
The AAMC has recommended that residency programs offer only virtual interviews for the upcoming season.
Who wins, and who loses? Let’s find out!
(thread)
The AAMC has recommended that residency programs offer only virtual interviews for the upcoming season.
Who wins, and who loses? Let’s find out!
(thread)
WINNER: Homegrown applicants.
Every year, many students choose to stay at the same institution for residency. Many PDs will be eager to snap up these “known quantities” from an otherwise more uncertain applicant pool.
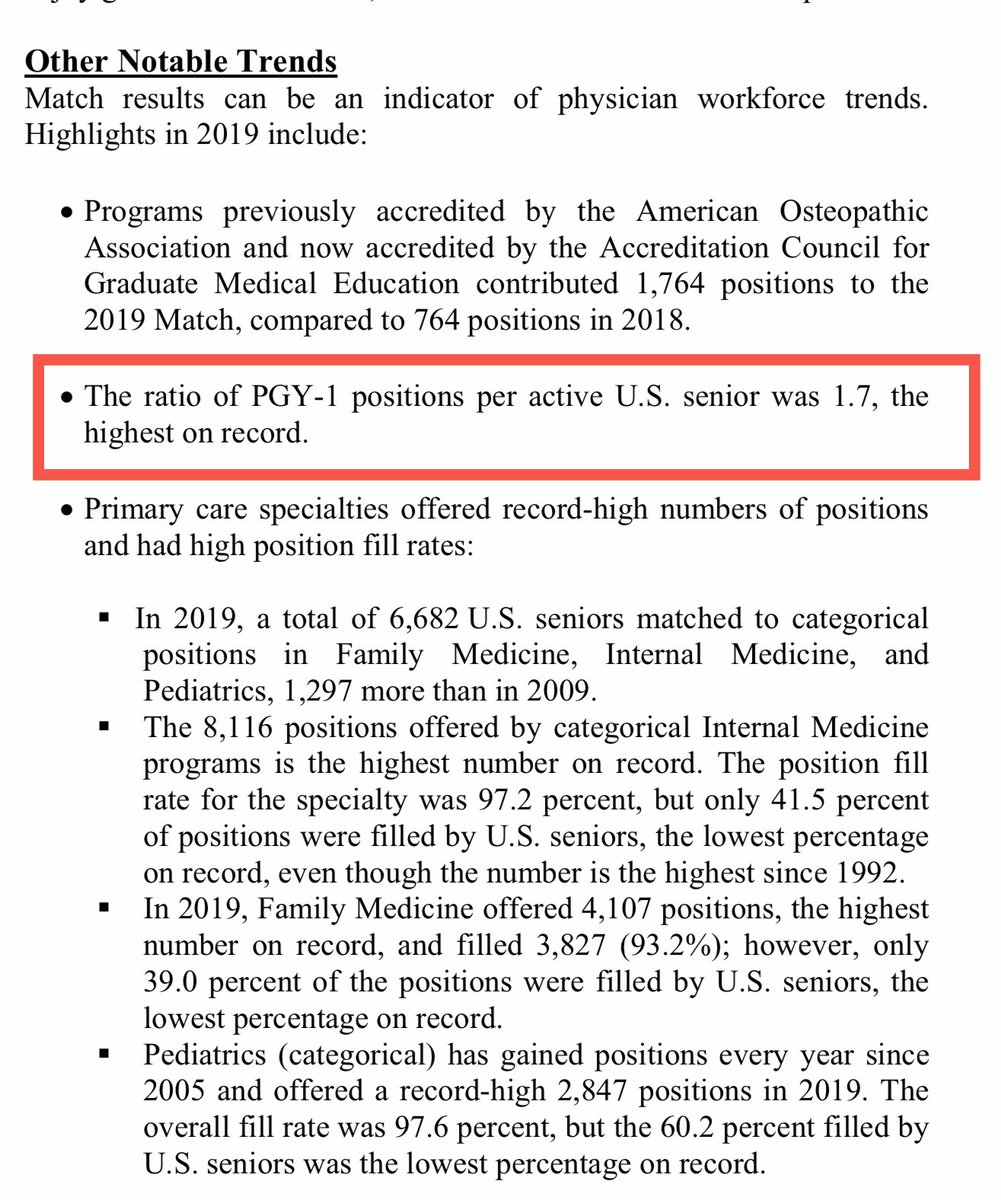
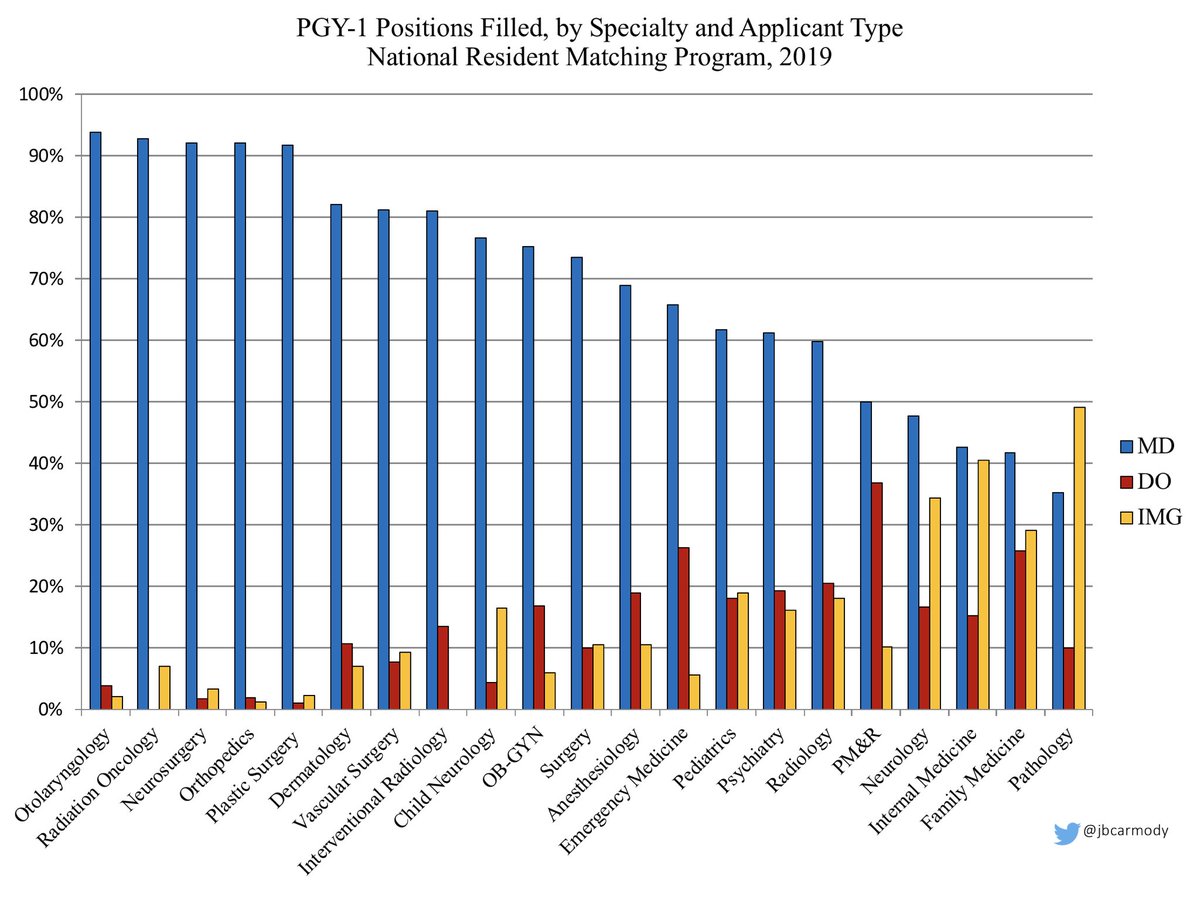
LOSER: DOs and IMGs, who may not have a “home” program.
Every year, many students choose to stay at the same institution for residency. Many PDs will be eager to snap up these “known quantities” from an otherwise more uncertain applicant pool.
LOSER: DOs and IMGs, who may not have a “home” program.
WINNER: Student travel budgets.
Previously, many applicants spent upwards of five figures traveling to in-person interviews. You gotta try *really* hard to spend that kind of money sitting in your living room doing Zoom and WebEx interviews.
Previously, many applicants spent upwards of five figures traveling to in-person interviews. You gotta try *really* hard to spend that kind of money sitting in your living room doing Zoom and WebEx interviews.
LOSER: Student ERAS budgets.
For years, the number of programs to which students apply has been steadily increasing. Throw in all the extra uncertainties of this application season, and I think it’s safe to expect a new record for 2020-2021.
For years, the number of programs to which students apply has been steadily increasing. Throw in all the extra uncertainties of this application season, and I think it’s safe to expect a new record for 2020-2021.

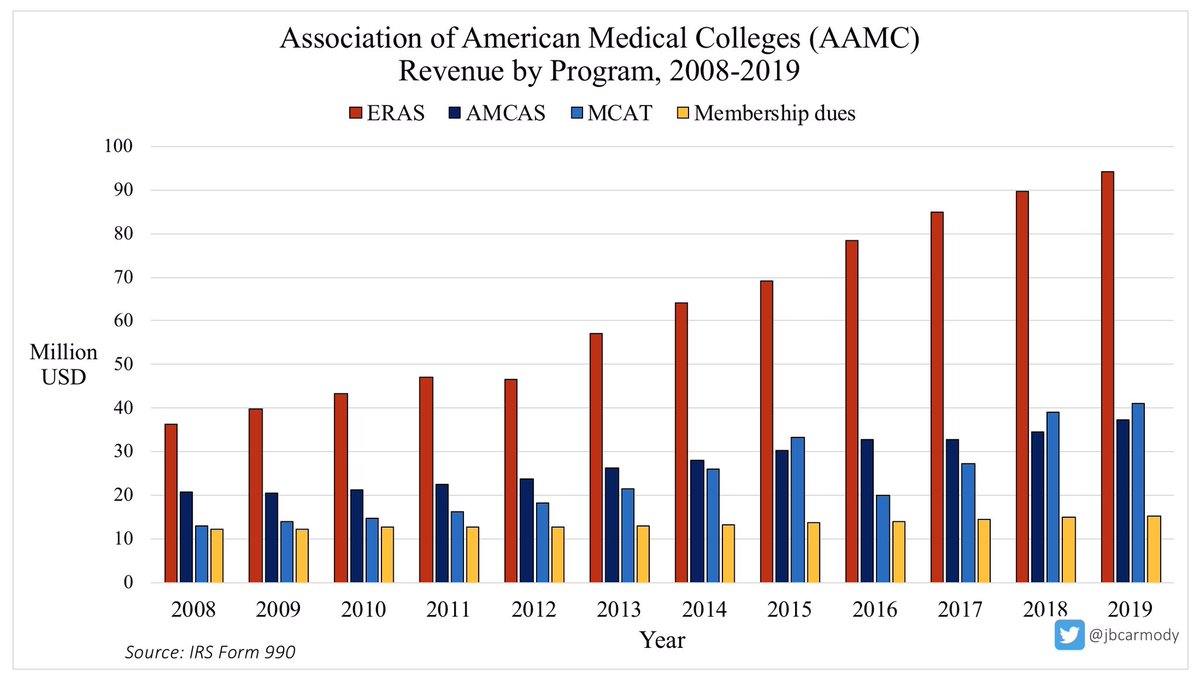
WINNER: The AAMC.
ERA$ was already the AAMC’s cash cow. And if applications climb even higher this season - which they will unless we impose some limits - it will benefit no one more than the AAMC.
ERA$ was already the AAMC’s cash cow. And if applications climb even higher this season - which they will unless we impose some limits - it will benefit no one more than the AAMC.
LOSER: Community and lesser-known programs.
If you can’t see the program in real life, which program would YOU rank more highly?
A) a lesser-known program
B) whatever the Doximity/USNWR rankings say is the “best” program
(Yeah, me too.)
If you can’t see the program in real life, which program would YOU rank more highly?
A) a lesser-known program
B) whatever the Doximity/USNWR rankings say is the “best” program
(Yeah, me too.)
WINNER: Residency programs with good web-designers, Instagram managers, and videographers.
If you’re asking applicants to come to your program sight unseen, you’d better show them as much as you can online. Those that do it well will prosper on Match Day.
If you’re asking applicants to come to your program sight unseen, you’d better show them as much as you can online. Those that do it well will prosper on Match Day.
LOSER: Programs that don’t increase the number of applicants interviewed.
Last year, a qualified applicant with 50 interview offers had to choose ~15 programs to travel to. Now, they can interview at all 50. Programs that don’t interview more applicants will risk going unfilled.
Last year, a qualified applicant with 50 interview offers had to choose ~15 programs to travel to. Now, they can interview at all 50. Programs that don’t interview more applicants will risk going unfilled.
WINNER: The attractive and non-obese.
Already, these applicants enjoy an advantage equivalent to around 10 points on USMLE Step 1. You’ve got to think that will be magnified even more when all PDs have to go on is somebody’s head on a screen.
journals.lww.com/academicmedici…
Already, these applicants enjoy an advantage equivalent to around 10 points on USMLE Step 1. You’ve got to think that will be magnified even more when all PDs have to go on is somebody’s head on a screen.
journals.lww.com/academicmedici…
LOSER: Women and under-represented minorities.
Will a short virtual interview be more bias-affirming than a more in-depth in person interview? (I fear it might... but I’d be happy to be wrong on this one.)
Will a short virtual interview be more bias-affirming than a more in-depth in person interview? (I fear it might... but I’d be happy to be wrong on this one.)
WINNER: Public health.
I have deep reservations about the consequences of this recommendation... but we’re all in the business of helping patients, and it’s hard to justify having 40,000 applicants flying from hospital to hospital this fall/winter. Less travel = lives saved.
I have deep reservations about the consequences of this recommendation... but we’re all in the business of helping patients, and it’s hard to justify having 40,000 applicants flying from hospital to hospital this fall/winter. Less travel = lives saved.
• • •
Missing some Tweet in this thread? You can try to
force a refresh