Yes, it’s true:
The reason a physician in graduate medical education training is called a “resident” is because back in the day, they *literally* lived in the hospital.
(a short thread)
The reason a physician in graduate medical education training is called a “resident” is because back in the day, they *literally* lived in the hospital.
(a short thread)
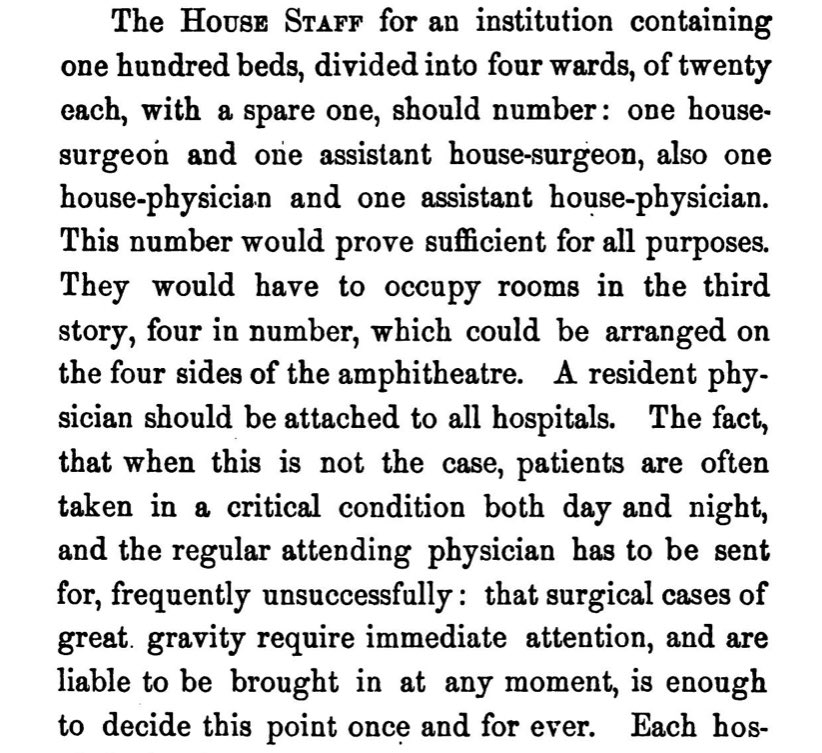
One text recommended two medical and two surgical residents per 100 beds, a number which would “prove sufficient for all purposes.”
(If you’re wondering why the residents lived on the upper floors, it’s because “in case of fire, they, being in good health, could easily escape.”)
(If you’re wondering why the residents lived on the upper floors, it’s because “in case of fire, they, being in good health, could easily escape.”)
But that’s not all.
A century ago, residency had no fixed time endpoint - training could last any amount of time.
Most programs also had a ‘pyramid’ structure, in which many interns competed for fewer resident positions at each level and ultimately just one chief resident spot.
A century ago, residency had no fixed time endpoint - training could last any amount of time.
Most programs also had a ‘pyramid’ structure, in which many interns competed for fewer resident positions at each level and ultimately just one chief resident spot.
Once you were chief, you stayed until a suitable faculty position became available.
For example:
Dr. Kenneth Blackfan - one of the most accomplished pediatricians of the era - served as a chief resident for 11 YEARS before becoming faculty.
en.wikipedia.org/wiki/Kenneth_B…
For example:
Dr. Kenneth Blackfan - one of the most accomplished pediatricians of the era - served as a chief resident for 11 YEARS before becoming faculty.
en.wikipedia.org/wiki/Kenneth_B…
(For anyone interested, last year I wrote a little bit about how we ended up with our residency training system.)
thesheriffofsodium.com/2019/12/22/why…
thesheriffofsodium.com/2019/12/22/why…
• • •
Missing some Tweet in this thread? You can try to
force a refresh