More on IOs from LITFL litfl.com/intraosseous-a…
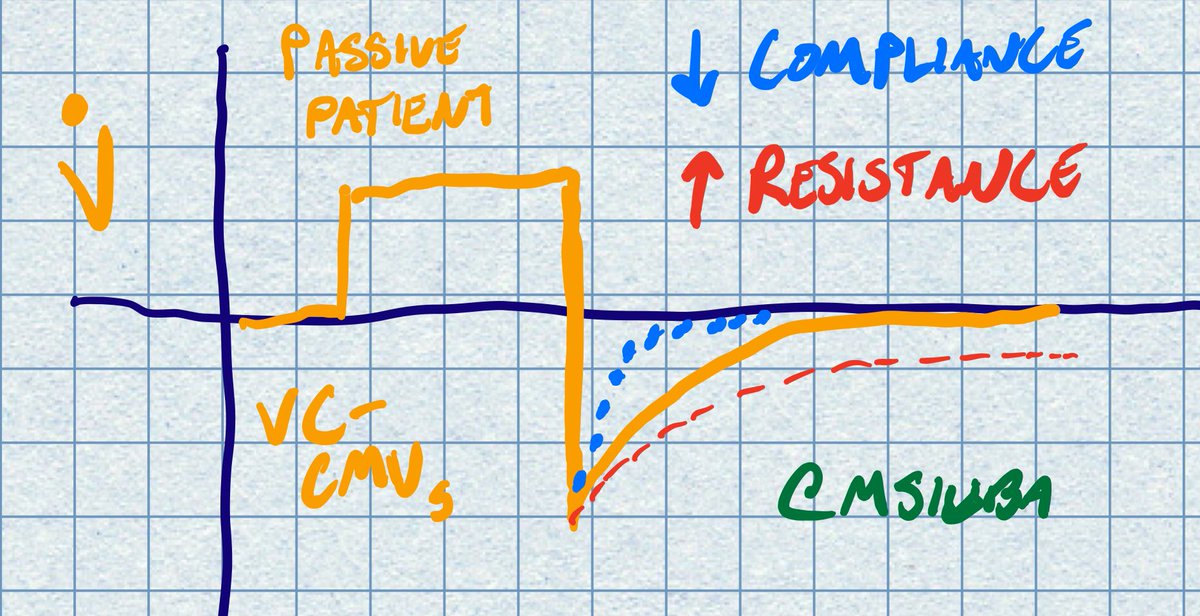
Also, the vent is alarming for high peak pressures (45 cm H2O consistently). What next?
Disconnecting vent is reasonable, but not diagnostic.
Plateau pressure is 42. What is *not* a possible explanation?
Your colleague is grabbing the POCUS machine. The *first* thing you do now is lower the tidal volume to 6 ml/kg. Airway pressures now Ppeak 34 and Pplat 31 on PEEP 8.
Notable RUSH Exam Findings (sorry for paucity of images given emergency):
Echo: no effusion, normal LV/RV size and fxn. Midrange IVC with respirophasic variation
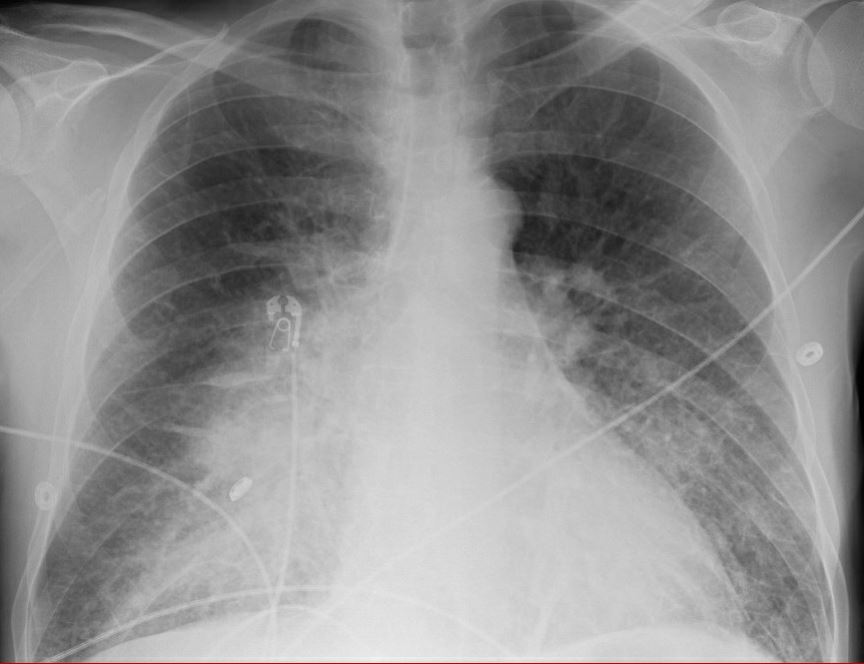
L: A lines throughout with +lung slide
R: Apical A lines, mid B lines, basilar consolidation with this septated effusion
RUSH otherwise neg. More on exam here: emcrit.org/rush-exam/orig…

Case resolution to follow tomorrow!
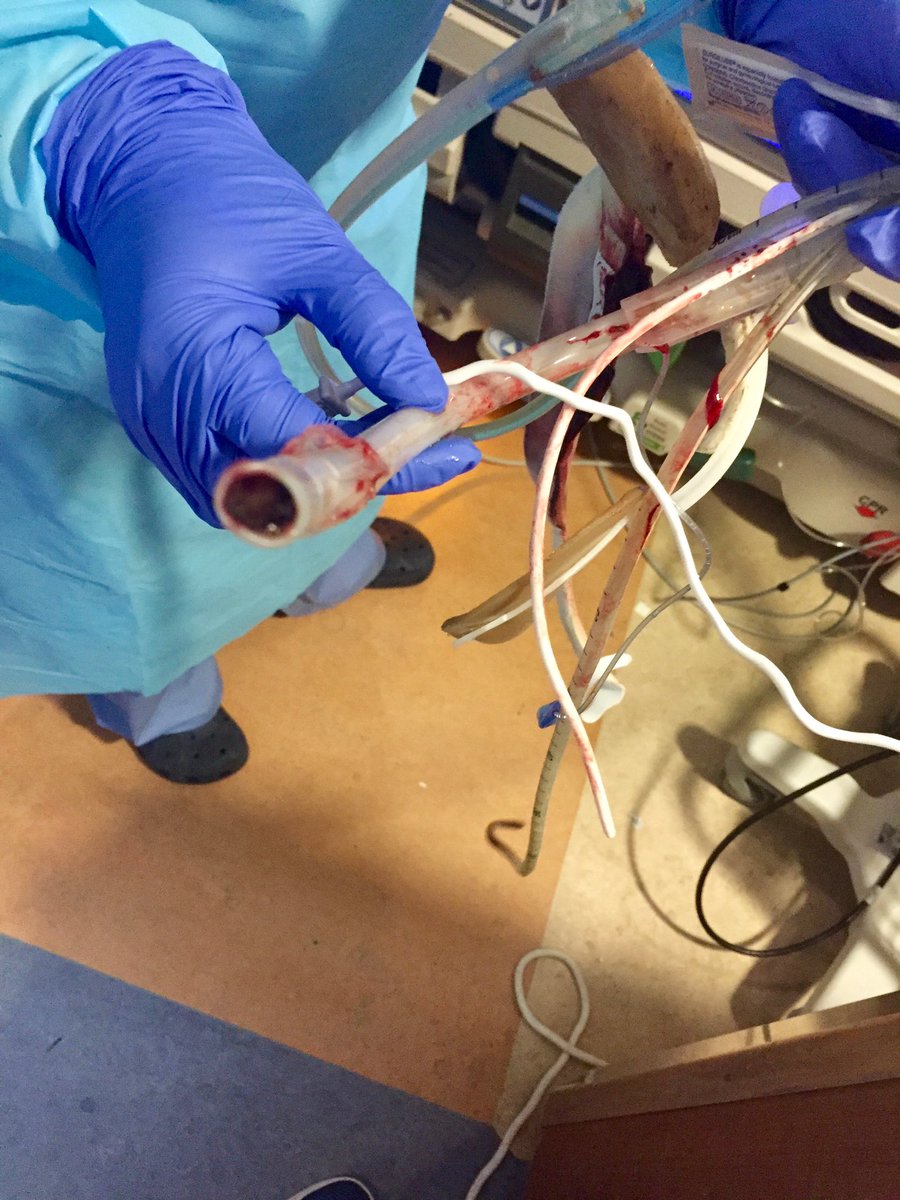
Effusion was situated anterior-laterally, with septations. Any other interventions you'd take?
TPA/DNAse was instilled. One hour later, additional 100 ml of frank purulent drainage was obtained.
Over the next 24 hours, pressors weaned off. 24 hours after that, the patient is extubated, quickly move out of ICU
#GoldenHour mentality (cc @ogi_gajic): We placed IO, tweaked the vent, gave antibiotics & hydrocortisone in the first hour in ICU.
However, we aim to apply *just* the right amount of intervention to right the ship. This is required (esp in terms of ABCs, time to abx, source control) in order to prevent further harm and needed interventions
Thanks for playing along!
What else did you learn or think of in this case? /end