That is our comfort zone.

Overnight, poof, you’re an adult ICU staffed with healthcare providers that have been trained to work with children and not with “grown ups”.
Today I do not want to be a doctor.
Nobody is getting any better.
Those who were well are sick again
and those who were sick are sicker.
The dying think they will live.
The healthy think they are dying.
Someone has taken too many pills.
A woman is losing her husband.
A husband is losing his wife.
The lame want to walk.
The blind want to drive.
The deaf are making too much noise.
The depressed are not making enough.
The asthmatics are smoking.
The alcoholics are drinking.
The mad are beginning to make sense.
Everyone’s cholesterol is high.
Disease will not listen to me
Even when I shake my fist.
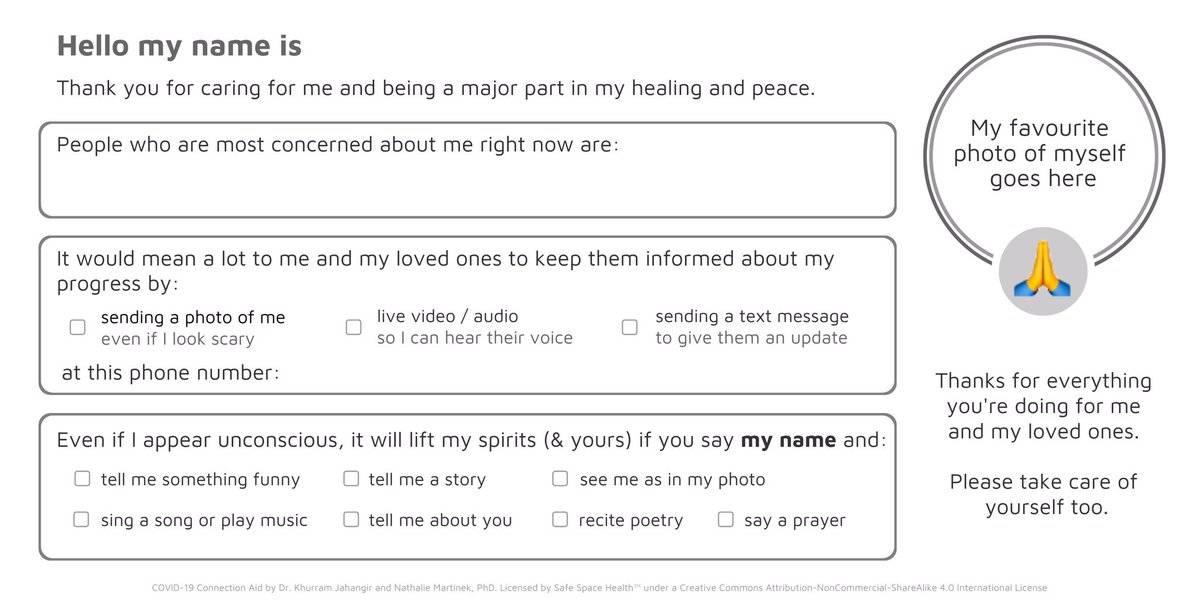
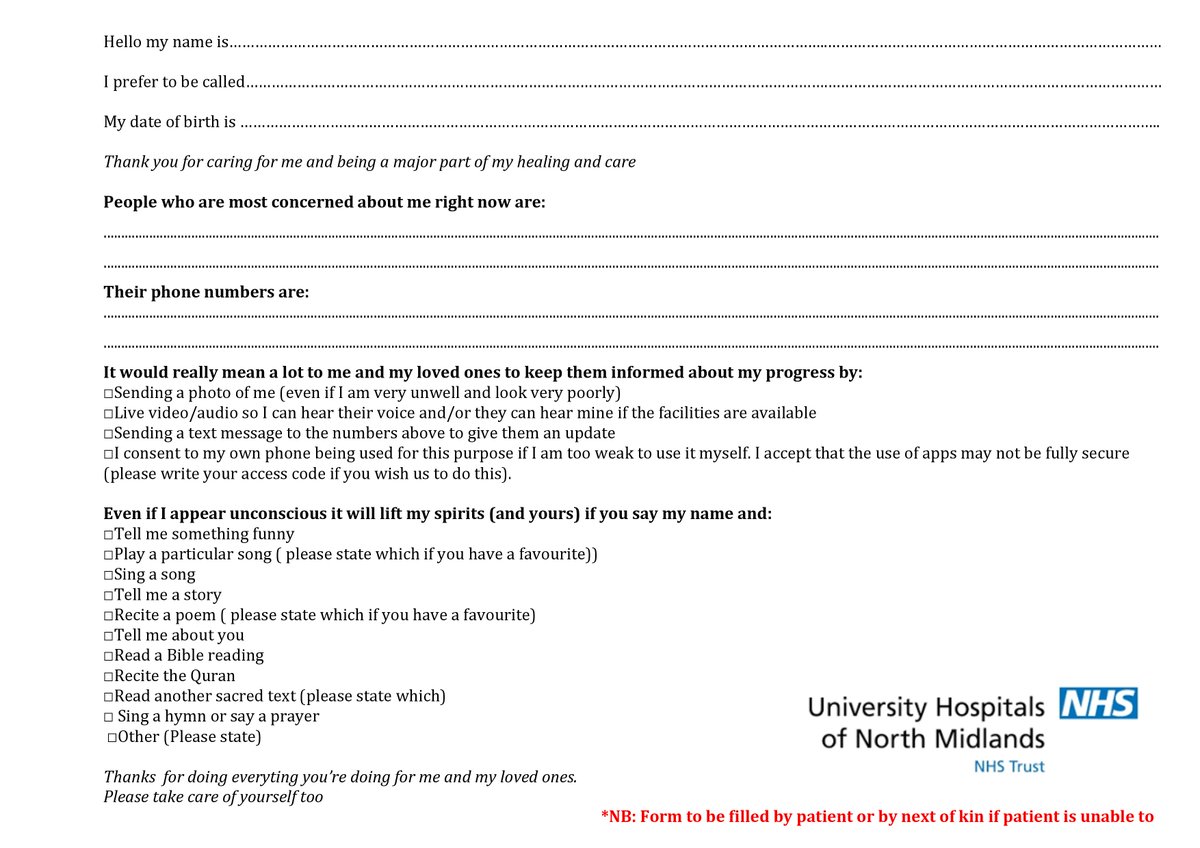
The first time she heard her daughters voice over a video call, in her own dialect, there were tears of joy. Not just from Mrs X but everyone else on the unit. From that point on Mrs X was galvanized.