#MedTweetorial
#Case: 26 y/o M presents to the ED after a syncopal episode. The patient lost consciousness for approximately 5 minutes. No tonic-clonic activity or urinary incontinence. Now experiencing generalized weakness, dyspnea, diaphoresis and palpitations.
#MedTwitter
PMHx: No prior PMHx or PSHx
Social Hx: Computer programmer – has been working 18 hour days x 1 month. Denies any alcohol, tobacco or illicit drug use.
Meds: None reported.
Case from: jmedicalcasereports.biomedcentral.com/articles/10.40…
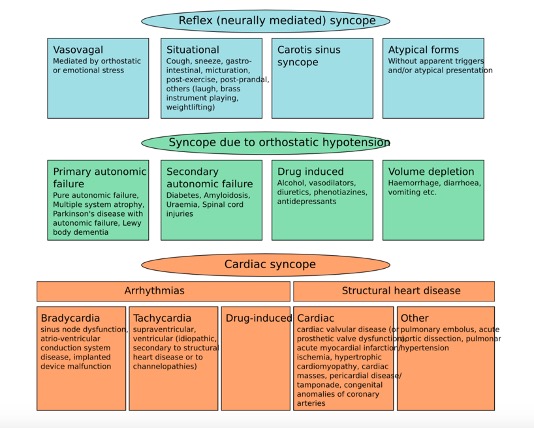
Brain Review of neurally-mediated, cardiac, and orthostatic induced syncopal causes.
Read More: ncbi.nlm.nih.gov/books/NBK44200…
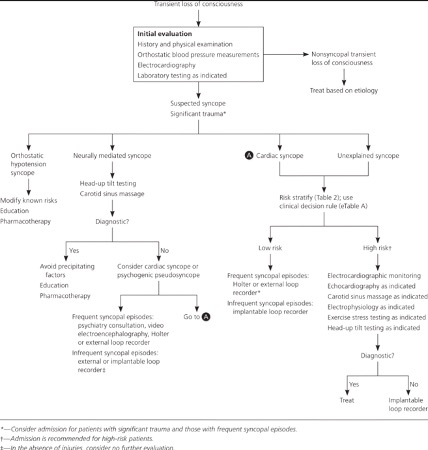
Great flow chart from: textbookofcardiology.org/wiki/Syncope
🩸Diagnostic workup for syncope: CBC, CMP, EKG, Troponin, Chest X-ray, cardiac monitoring, orthostatic vital signs, echocardiogram, d-dimer (sensitive not specific). Head trauma or neurologic symptoms? Consider a CT head without contrast.
Read More: aafp.org/afp/2017/0301/…
Poll: Which of the following is currently a top differential diagnosis?
🦪 Clinical Pearl: S1Q3T3 – S wave in lead I, Q wave in lead III, inverted T-waves in lead III.
Neither sensitive nor specific for PE. Only present in approximately 20% of patients with PE. It can be a life-saving identification on EKG indicating further PE workup.
🩺 Physical Exam:
General: Diaphoretic.
Head/Neck: Atraumatic/Normocephalic
Lungs: Dyspneic. Reduced breath sounds to auscultation of the bilateral bases.
Chest: Tachycardic. No murmurs, rubs, or gallops.
Extremities: Unilateral LLE swelling. Homan’s sign positive.
Well’s Criteria:
(+3 pts) – Clinical symptoms of DVT
(+3 pts) – PE is #1 DDx
(+1.5 pts) – HR > 100
(+ 1.5 pts) – Immobilization > 3 days/surgery in the past 4 weeks
(+ 1.5 pts) – Prior DVT/PE diagnosis
(+1 pts) – Hemoptysis
(+1 pts) – Malignancy with treatment < 6 months
PERC Rule: RULES OUT PE - ONLY Accurate when used for LOW-risk patients
H: Hormones (estrogen)
A: Age > 50
D: DVT/PE Hx
C: Coughing up blood
L: LE swelling
O: O2 < 95%
T: Tachycardia
S: Surgery/Trauma in the past 4 days
“HAD CLOTS”
Our patient: PERC Rule = +3; WELL's = +9
🧪 Initial Labs:
Normal: CBC, CMP, and Chest X-Ray
ABG: PO2 = 58 mm Hg (hypoxia)
Transthoracic echo reveals mild pulmonary hypertension (42 mm Hg) and normal LV function. No patent foramen ovale, ASD or VSD identified.
DVT identified upon LLE US.
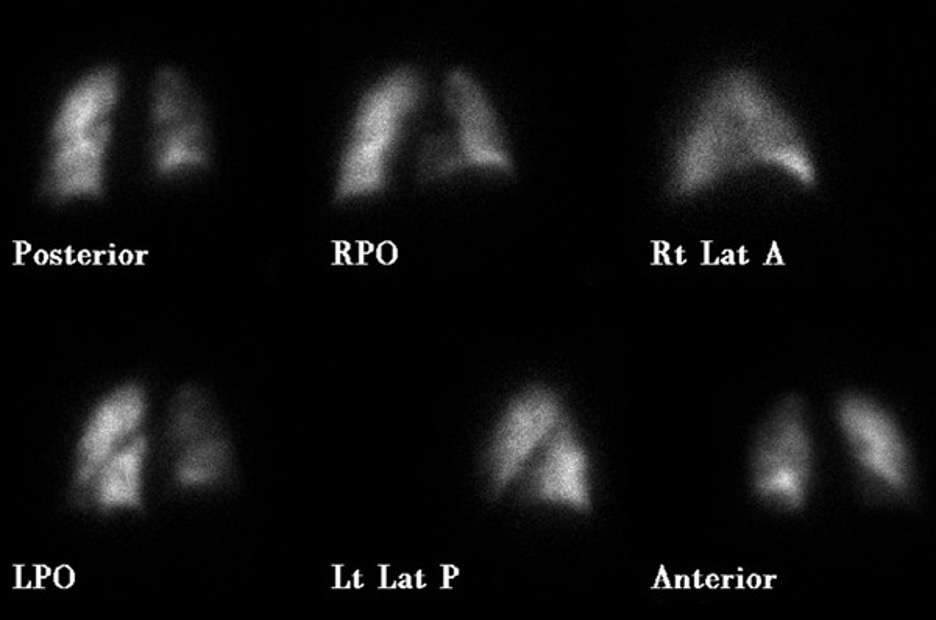
Lungs V/Q scan
Figure 1: Perfusion measured with TC-99 revealing decreased perfusion to the right lower lobe (as seen on RPO)
Figure 2: Ventilation scan with Xe-133 gas showing no diminished ventilation.
jmedicalcasereports.biomedcentral.com/articles/10.40…
Microscope Case recap!
Atypical presentation of pulmonary embolism as a syncopal episode. Positive V/Q mismatch, S1Q3T3 EKG pattern. Patient was treated with unfractionated heparin and oral warfarin therapy.
Read more regarding syncope and pulmonary embolism correlation: journals.sagepub.com/doi/pdf/10.119…
Or learn more from a similar case with syncope as an atypical presentation of pulmonary embolism
nejm.org/doi/full/10.10…
Review Q!
What is the most sensitive physical exam finding indicating an acute pulmonary embolism?
Review Q answer explained.
Answer: B. Hypoxia (96.9% sensitivity) correlates with tachypnea (respiratory rate > 20/min). The clot occludes the pulmonary artery, leading to an increase in pulmonary ventilation without an increase in perfusion leading to a VQ mismatch.
The chemoreceptors (innervated by CN IX and CN X) detect the increased CO2 + decreased O2 content, increasing the innervation of the dorsal respiratory group. CO2 readily diffuses across the blood-brain barrier into a specific subdivision of the dorsal
respiratory group located in the rostral dorsolateral pons, the pneumotaxic center. CO2 and H+ ions have a direct effect on the respiratory center, causing an increased inspiratory/expiratory rate, leading to physiologic tachypnea. Oxygen, however, has no direct effect on
the respiratory center and acts almost entirely on chemoreceptors located in the carotid and aortic bodies. The leading cause of this tachypnea has been discovered to be excitation of the chemosensitive neurons by hydrogen ions stimulated by the crossing of CO2 into
the brain and its dissociation into H+ and HCO3-.
Emergency Medicine junkies – Check out this awesome website and podcast episode on pulmonary embolism!
emergencymedicinecases.com/episode-21-res…



